*Corresponding Author:
Laura Tyler Perryman,
Stimwave Technolo- gies, Incorporated1310 Park Central Boulevard South, Pompano Beach Florida 33064, USA
Tel: +1 8009655134
Email: laura@stimwave. com
Abstract
Background: Incidence of low back pain is showing increasing trend and back surgery is reported to have nearly 20% failures. Spinal Cord Stimulation (SCS) is cost effective in managing pain following Failed Back Surgery Syndrome (FBSS). In order to improve results and acceptability of the neuromodulation there is a need for lowering complications.
Objective: To report a minimally invasive neuromodulation technology in the treatment of chronic intractable back pain patients as a result of failed back surgery.
Material and Methods: Patients suffering from refractory back pain were included in the studies of this minimally invasive wireless method of neuromodulation. Compared to the standard SCS with multiple connecting and large footprint implantable components, the wireless device employs an implantable electrode with a receiver that is placed in the inner lumen of the device with an external power generator. Both low and high frequency stimulation parameters with variable pulse widths can be included in the treatment protocol within the following ranges: amplitude: 1 24 mA, pulse width: 10 1000 microseconds, frequency: 5 20,000 Hz. A VAS pain rating scale, Oswestry Disability Index, EQ-5D-5L Quality of Life Questionnaire (QLQ) and Global Impression scale (PGIC) were administered at 3, 5, 8, 12 weeks post-implantation.
Results: In this prospective review, study patients included 28 FBSS cases with epidural spinal cord stimulator placements and 18 cases with exiting nerve Dorsal Root Ganglion (DRG) and dorsal horn placements. A consistent relief of pain of more than 50% ensued in all the patients. There was also improvement in the QLQ, disability and PGIC. The procedure was well tolerated and no significant complications were observed. Electrode migration in a case of an existing nerve root placement required a revision. Both low and high frequency stimulation were effective as required by the patient condition and preference.
Conclusion: Minimally invasive wireless neuromodulation yielded satisfactory improvements in pain, disability and QLQ. The procedure was safe and further studies in larger number of patients are required for an expanded utility in a wider variety of pain disorders.
Keywords
Back pain; FBSS; Neuromodulation; Neuropathy; Wire- less stimulation
Introduction
Center for Disease Control (CDC) published data showed that in adult age groups low back pain has increased in incidence studied between 1997 and 2013 [1]. At any given point of time nearly 13 million Americans suffer from low back pain according to a NEJM report [2,3]. These numbers, according to the above CDC report have worsened over the past decade. The incidence of lumbar spine surgery is 5 per 10,000 people in the UK with failure rates between 10-40% (approximately 20% on average) [3-5]. For the chronic intractable pain following spine surgery several options including medical and interventional are recommended. Spinal Cord Stimulation (SCS), among these, has been established as a cost effective treatment for neuropathic back and leg pain [6-9].
The National Institute for Health and Clinical Excellence has shown that SCS is the treatment of choice in selected patients for refractory neuropathic pain of FBSS apart from cases with neuropathic pain, critical limb ischemia and refractory angina [10]. Traditionally SCS technology has utilized four components: an electrode array, an extension that connects the electrode area to the implantable pulse generator, the implanted pulse generator itself, and the external remote control programmer. The first three components are surgically implanted inside the patient body, but moreover have a surface area footprint that is large encompassing up to 40 cc or more of space and requiring a large subcutaneous surgical pocket. Apart from being not possible to make this placement in thinner patients that do not have the body mass index to have a large amount of subcutaneous tissue, the SCS results are affected by complications resulting from this extensive implantation system and in over 15-20% of the patients, this large surgical pocket is causing enough pain that patients are removing the system [11,12]. Although over the years further improvements ensued in the battery longevity and form factor from some manufacturers, extensive surgery is still required as well as large multiple incisions and extensive tunneling to place these systems some of which are over 40 cc in volume. A minimally invasive approach that involves placement of only the electrodes attached to a catheter that houses the receiver at a total of 5% of the volume of the others to yield equally effective stimulation is described here. This technology utilizes an external, (non-implantable) wireless power generator which is worn by the patient in clothing lining.
This presentation introduces a novel minimally invasive wireless neuromodulation technology in the management of chronic refractory pain, mainly FBSS, along with observations from pilot studies and case series.
Material and Methods
The technology described here has been in clinical use for over one year. The applications for the relief of back pain and leg pain in- clude Spinal Cord Stimulation (SCS) and Dorsal Root Ganglion stim- ulation (DRG) administered through a transforminal and transgrade approach with electrodes over both the DRG and the dorsal horn as- pect of the epidural space.
Subjects were implanted with one or more wireless stimulator systems (Stimwave LLC, Pompano Beach, FL, USA) each containing four or eight contacts (3 mm in diameter with 4 mm spacing). The stimulator system utilizes an implantable electrode contact array, mi- croprocessor and an added separate antenna receiver mated with the stimulator that is powered by an external transmitter (Figures 1 & 2). The implanted stimulator is 100% passive and has no internal pow- er source. The external transmitter, the power generator, (Figure 3) is worn by the patient over a single layer of clothing or within clothing and wirelessly powers the implanted stimulator.

Figure 1: Neuro-stimulator electrode, MRI compatible, for both 1.5 and 3 Tesla.
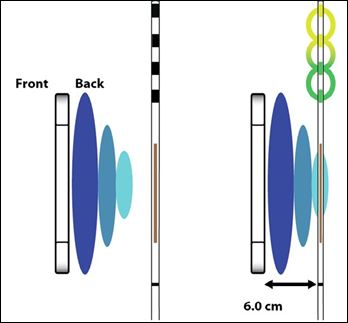
Figure 2: Neurostimulator receiver.
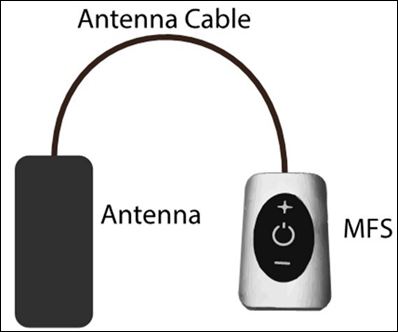
Figure 3: External pulse generator.
The external generator sends the desired stimulation parame- ters through an RF transmitting antenna to the implanted stimulator through a wireless receiver [13]. The system uses radiofrequency en- ergy at 915 MHz to transfer power and selected parameters. Wave- lengths and product specifications have been designed to decrease risks related to the wireless transmission of energy and to transfer the clinician’s desired stimulation parameters reliably to the implant [13]. The following spectrum of stimulation parameters is possible with the system for clinical applications: Amplitude: 1to 24 mA, pulse width: 10 to 1000 microseconds, pulse rate: 5 to 20,000 Hz. The transmitter lasts 24 hours.
Procedure
Under strict aseptic precautions, the skin and subcutaneous tissues were infiltrated with local anesthetic (1% lignocaine). A small skin incision was made for a 14-gauge Tuohy needle insertion, which was shaped by hand to match the body contour to achieve appropriate device placement. Stimulator was inserted through the Tuohy needle and placed epidurally for SCS or targeted at the traversing and exiting nerves for DRG target. Antero-posterior, lateral and oblique fluoro- scopic images obtained during the procedure guided the placement of the electrode up to the final positioning in real time (Figure 4). The stimulator system was subsequently activated wirelessly to confirm electrode positioning with the patient reporting comfortable pares- thesia along the distribution of the targeted nerve, after retraction of the needle tip exposing electrode contacts. The device was anchored via a sub-dermal suture located at the skin entry point. Distal tubing was cut at the insertion site and buried subcutaneously. The skin entry site was approximated.

Evaluations
Patients were monitored for ongoing pain relief and adverse events at 4 weeks post-implant and for 3 months follow up. Subjects were asked to describe their pain relief using the Visual Analog Scale (VAS). An Oswestry Disability Index (ODI), EQ-5D-5L Quality of Life Questionnaire (QLQ) and Patient Global Impression scale (PGIC) were also administered at 4, 8, 12 weeks months post-implantation.
Patient population included 28 FBSS cases for epidural SCS and18 patients with DRG placement for FBSS. Stimulation was deliv- ered at both Low Frequency (LF) and High Frequency (HF) as per the patient requirement and study protocol (Table 1). The implantation, as described above has been tolerated very well because of its sim- plicity. There have been no adverse events reported or any complica- tions related to surgery or stimulation. One patient had to get the lead replaced at DRG due to ineffective stimulation related to migration. Procedures have been performed on out-patient basis.

Results
There were 28 patients with SCS and 18 with DRGS implantations; 22 had LF stimulation and 24 received high frequency stimulation (Table 1) for relief of chronic back pain following back surgery. Sustained pain relief resulted following stimulation protocol in all patients (N=46). The pain scores and functionality as well as disability have improved during the short term follow up. Significant reduction in pain medication was observed during the review period. The stimulation protocol was effective at low as well high frequency stimulations. Additionally, the technology was utilized for stimulation at different levels for DRGS, an area of further scientific research. No wound infection, hemorrhage or other serious complications were observed during the procedure as well as the follow up period.
Discussion
Spinal cord stimulation as a preferred method of therapeutic approaches for chronic pain management has come a long way and is now an established standard of care. In FBSS, chronic benign pain and regional pain syndromes the efficacy and cost effectiveness of SCS is evidence based at present [6,14,15]. However, the present day technology of SCS and DRG is bulky with lengthy connection cables and implantable power generator. Thus it carries the burden of all the complications associated with implanted components [11,12,16-18]. In the Austrian nationwide study device dislocation occurred in 13% of implantations and electrode fractures in 5% with infections in 6% of the cases analyzed [19]. Implanted Pulse Generator (IPG) related complications were reported in 27% cases by Hamm-Faber et al and repositioning of the IPG due to pain caused by tilting of the battery in 27%. They also had problems with connecting pieces between lead and the extension cable in 1 patient (9%) [20]. IPG complications were reported in 3 out of every 7 cases (42.8%) in a series reported by Buiten et al., where a conventional PNS/SCS implant system was utilized for control of refractory angina [21].
Wireless neuromodulation, on the other hand, mitigates these complications related to the conventional SCS/PNS devices and shows promise while expanding the number of indications for the treatment of chronic pain conditions [22]. There is a significant reduction in hardware components. A simple percutaneous placement of the electrode without the need to tunnel and attach an implanted pulse generator can be advantageous to the patient and the surgeon in reducing costs, procedure time, postoperative pain and adverse events while achieving the desired pain control.
In a pilot study we have earlier reported our experience in 11 patients receiving DRGS for low back pain persisting after back surgery. All these FBSS patients improved with sustained pain relief at the end of the trial period [23]. Migration in unanchored group of patients was reported in DRGS trial without any correlation to pain relief by Weiner et al., even at 8.8mm (mean) distance [23].
This experience improved our approach to minimize migration in DRG placements. The above results in 35 additional cases, illustrate the safety and feasibility of the wireless neuromodulation system, emphasizing the fact that this modality is completely devoid of IPG related complications [24]. The surgical procedure is percutaneous, minimally invasive, requires only a small incision to place the electrode. No further incisions or implants are required for the therapy and thus, the technology provides the comfort, the cosmetic result apart from minimizing the procedural costs, operating time, postoperative pain, minimizing adverse events while desired pain control is attained [22,25]. Both low and high frequency stimulation were effective as required by the patient condition. The transmitter lasts 24 hours and battery gets recharged. The wireless therapy has carryover effects for 8-24 hours and thus most patients do not require round the clock stimulation and during night time. In those few cases that need additional duration of stimulation, a desk top transmitting unit is available (since the antenna is fabric). In addition, the technology is beneficial to the “compromised host” with immune suppression, retroviral infections, fragile skin conditions that prohibit long tunneling and multiple incisions and in patients with limited life expectancy including those with terminal illness like cancer.
Summary
A novel wireless neuromodulation is utilized in 46 patients with chronic intractable back pain for relief. The technique is minimally invasive and required percutaneous placement of electrode array only, thus avoiding implantation of long extension coils and implantable power generator. The procedure was tolerated well by all the patients at low as well as high frequency stimulation at the patient requirement. No untoward effects and adverse events were reported. Short term relief of pain could be obtained in all the patients and requirement for pain medication had come down significantly. However, multicenter, prospective studies in larger population are required for this promising technology. This innovative neuromodulation is expected to expand the indications for pain intervention in wider spectrum of patients.
References
- Centers for Disease Control and Prevention (2014) Health, United States. Centers for Disease Control and Prevention, Atlanta, GA,
- Jensen MC, Brant-Zawadzki MN, Obuchowski N, Modic MT, Malkasian D, et al. (1994) Magnetic Resonance Imaging of the Lumbar Spine in People Without Back Pain. N Engl J Med 331: 69-116.
- Taylor RS (2006) Epidemiology of refractory neuropathic Pain Practice 6: 22-26.
- North RB, Kidd DH, Zahurak M, James CS, Long DM (1993) Spinal cord stimulation for chronic, intractable pain: experience over two decades. Neurosurgery 32: 384-394.
- Thomson S (2013) Failed back surgery syndrome definition, epidemiology and demographics. Br J Pain 7: 56-59.
- North RB, Kidd DH, Farrokhi F, Piantadosi SA (2005) Spinal cord stimulation versus repeated lumbosacral spine surgery for chronic pain: a randomized, controlled Neurosurgery 56: 98-106.
- Kumar K, Taylor RS, Jacques L, Eldabe S, Meglio M, et al. (2008) The effects of spinal cord stimulation in neuropathic pain are sustained: a 24-month follow-up of the prospective randomized controlled multicenter trial of the effectiveness of spinal cord Neurosurgery 63: 762-770.
- Simpson EL, Duenas A, Holmes MW, Papaioannou D, Chilcott J (2009) Spinal cord stimulation for chronic pain of neuropathic or ischaemic origin: systematic review and economic Health Technol Assess 13: 1-154.
- Taylor RS, Ryan J, O’Donnell R, Eldabe S, Kumar K, et al. (2010) The cost-effectiveness of spinal cord stimulation in the treatment of failed back surgery Clin J Pain 26: 463-469.
- National Institute for Health and Care Excellence (2008) Spinal cord stimulation for chronic pain of neuropathic or ischaemic origin. National Institute for Health and Care Excellence, London, United Kingdom.
- Cameron T (2004) Safety and efficacy of spinal cord stimulation for the treatment of chronic pain: a 20-year literature review. J Neurosurg 100: 254-267.
- Kim DD, Vakharyia R, Kroll HR, Shuster A (2011) Rates of lead migration and stimulation loss in spinal cord stimulation: a retrospective comparison of laminotomy versus percutaneous Pain Physician 14: 513-524.
- Tyler PL, Larson P, Glaser J (2016). Tissue depth study for a fully implantable, remotely powered and programmable wireless neural stimulator. Int J Nano Stud Technol 2: 1-6.
- Kemler MA, de Vet HC, Barendse GA, van den Wildenberg FA, van Kleef M (2008) Effect of spinal cord stimulation for chronic complex regional pain syndrome Type I: five-year final follow-up of patients in a randomized controlled J Neurosurg 108: 292-298.
- Kumar K, Hunter G, Demeria D (2006) Spinal cord stimulation in treatment of chronic benign pain: challenges in treatment planning and present status, a 22-year Neurosurgery 58: 481-496.
- Taylor RS, Van Buyten JP, Buchser E (2005) Spinal cord stimulation for chronic back and leg pain and failed back surgery syndrome: a systematic review and analysis of prognostic Spine 30: 152-160.
- Slavin KV (2011) Technical aspects of peripheral nerve stimulation: hardware and Prog Neurol Surg 24: 189-202.
- Slavin KV, Vannemreddy PS (2011) Repositioning of supraorbital nerve stimulation electrode using retrograde needle insertion: a technical note. Neuro- modulation 14: 160-163.
- Sator-Katzenschlager S, Fiala K, Kress HG, Kofler A, Neuhold J, et (2010) Subcutaneous target stimulation (STS) in chronic noncancer pain: a nation- wide retrospective study. Pain Pract 10: 279-286.
- Hamm-Faber TE, Aukes H, van Gorp EJ, Gültuna I (2015) Subcutaneous Stimulation as an Additional Therapy to Spinal Cord Stimulation For the Treatment of Low Back Pain and Leg Pain in Failed Back Surgery Syndrome: Four-Year Follow-Up. Neuromodulation 18: 618-622.
- Buiten MS, DeJongste MJ, Beese U, Kliphuis C, Durenkamp A, et al. (2011) Subcutaneous Electrical Nerve Stimulation: A Feasible and New method for the Treatment of Patients With Refractory Neuromodulation 14: 258- 265.
- Yearwood TL, Perryman LT (2015) Peripheral Neurostimulation with a Microsize Wireless Prog Neurol Surg 29: 168-191.
- Weiner RL, Yeung A, Montes Garcia C, Tyler Perryman L, Speck B (2016) Treatment of FBSS low back pain with a novel percutaneous DRG wireless stimulator: Pilot and feasibility Pain Medicine 17: 1911-1916.
- Klieber J-C, Marlier B, Bannwarth M, Theret E, Peruzzi P, et al. (2016) Is spinal cord stimulation safe? A review of 13 years of implantations and com Rev neurol 171: 689-695.
- Perryman LT, Speck B, Weiner RL (2017) A novel wireless minimally invasive neuromodulation device for the treatment of chronic intractable occipital neuralgia: case J Neurol Stroke 6: 00213.
Citation: Perryman LT (2018) Wireless Neuromodulation in the Management of Chronic Refractory FBSS Back Pain: Preliminary Prospective Experience with Different Stimulation Targets and Waveforms. J Anes Perio Manag 2: 003.
Copyright: © 2018 Perryman LT. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.