*Corresponding Author:
Yasser Ahmed Ghaleb,
Yemen Field Epidemiology Training Program, National Blood Transfusion and Research Centre, Sana’a, Yemen
Tel: +967- 772265039
E-mail: ysrghaleb@gmail.com
Abstract
Background: Transfusion-Transmissible Infectious (TTIs) agents such as Hepatitis B Virus (HBV), Hepatitis C Virus (HCV), Human Immunodeficiency Virus (HIV), syphilis and malaria are the greatest threats to blood safety for transfusion recipients and pose a serious public health problem in Yemen.
Aims: To determine the magnitude of Transfusion-Transmitted Infections (TTIs) among blood donors and its associated factors.
Method: A cross-sectional study was conducted on 340 blood donors at the National Blood Transfusion and Research Center during November and December 2017. Data was collected through face-to- face interviews using a predesigned questionnaire that covered socio- demographic characteristics and associated factors with TTIs. Blood samples were drawn and tested for HBV surface antigen (HBsAg), HCV antibodies, HIV I & II by using electrochemiluminescence immunoassay technique and rapid immunochromato-graphic for screened syphilis and malaria antibodies.
Result: The overall prevalence of TTIs was 8.8% where 2.5 %, 1.2%, 0.3%, 1.2%, 3.2% have HBV, HCV, HIV, syphilis and malaria respectively. HBV was significantly associated with history of jaundice and cupping. Furthermore, urethero-vaginal excretion was significantly associated with syphilis while malaria was significantly higher among donors from malaria endemic areas. Nearly three- fourth of donations were replacement donors who had significantly higher TTIs prevalence than the voluntary donors: 10.4% vs. 3.3%, OR 3.4 (CI: 1.1-11.6).
Conclusion: Although the prevalence of TTIs is low, it remains an important problem in blood transfusion. Therefore, establishment of TTIs surveillance system, improving donor recruitment procedures and increasing the proportion of regular and voluntary donation with the use of more sensitive screening methods is recommended.
Keywords
Blood donors; HIV; Malaria; Syphilis; Transfusion transmitted infections
Background
Blood Transfusion (BT) is a life-saving intervention where it saves millions of lives each year globally, however it’s associated with risks that could lead to adverse consequences. Besides BT acute and delayed complications, there is a risk of 1 to 2 per 1000 recipients, to receive contaminated blood with viral, bacterial or parasitic Transfusion Transmitted Infections (TTIs) [1,2].
The strategic framework for blood safety and availability 2016-2025 of WHO recommends an integrated strategy including availability of a well-organized and adequately funded nationally coordinated BTS, with an effective blood components programme under well-defined regulatory oversight. In addition, prioritization of blood donation from Voluntary Non-Remunerated Donors (VNRD), quality-assured testing of all donated blood, including screening for TTIs, reduction in unnecessary transfusions through appropriate clinical use and safe administration of blood and blood products; and implementation of effective quality systems in all areas of BTS were recommended [3].
TTIs are defined as any infection that is transmissible from person to person through blood transfusion of blood or blood products [4]. Among them are Hepatitis B Virus (HBV), Hepatitis C Virus (HCV), human immunodeficiency virus (HIV 1,2), syphilis and transfusion associated malaria infection [5]. According to WHO reports, the prevalence of HBV, HCV, HIV and syphilis infections among blood donors in different parts of the world varies from 0.03%-8.47%, 0.02%-1.80%, 0.003%-2.69%, and 0.05%-1.88%, respectively [6].
However, in low-income countries, such prevalence rates increase to 3.34%-8.47%, 0.67%-1.80%, 0.56%-2.69% and 0.31%-1.88% respectively [6]. Furthermore, malaria constitutes a big health problem in the general population where in 2016; there were an estimated 216 million cases in 91 countries [7]. Transfusion-transmitted malaria occurs at an estimated rate of 0.25 cases per 1 million blood units collected [8].
In Yemen, TTIs found to be an important health problem due to war consequences and conflict, as well as upsurge of casualties and injuries that may increase the possibility of TTIs among recipients through using rapid blood screening methods that have low sensitivity and specificity. Studies that were conducted in Sana’a City, Aden and Hodeidah revealed that hepatitis B and C viruses and HIV are a major issue among blood donors. The prevalence of HBV, HCV, HIV and syphilis according to those studies varies from 2.1%-5.1%, 0.79%-3%, 0.34%-0.39% and 0.34%-0.75%, respectively [9-12].
Furthermore, previous study found that 8.33% of blood donors were positive for malaria [13].
The National Blood Transfusion and Research Center (NBTRC) is the main blood transfusion center in Sana’a City, which launched in 2006 to ensure safe blood and blood products for all patients’ needs and regulate the BTS in the whole country. During 2006 to 2017, the center collected 144,458 blood units from VNRD and Family Replacement Donors (FRD).
Since its establishment, the NBTRC is focusing on blood transfusion services provision with little emphasis on research component due to limited capacities, lack of earmarked research budget and poor documentation caused by absence of computerized registration system. Therefore, there are few studies that were conducted at the NBTRC and none of them was on TTIs.
This study aims to determine the prevalence of TTIs among blood donors and its associated factors. It will help to understand the magnitude of the problem and to guide evidence-based decision making to ensure the safety of blood transfusion through better donor selection, motivation, retention and care as well as improving screening practices against TTIs.
Methods
Study population and setting
The study was conducted on blood donors at the NBTRC during November to December 2017. It is the main center for blood transfusion services in Sana’a, which provides blood transfusion services to the local, as well as for the population coming from different governorates. All healthy donors from different localities (rural and suburban population) come to donate as VNRD or for their relatives. The standard criteria for selection of blood donors was used based on NBTRC and WHO guidelines [14]. These criteria include: age of donor arranged between 18 to 55 years, body weight greater than 50 kg, hemoglobin level between 14 -18 g/dl for male and 12.5-16 g/dl for females with normal pulse rate of 60-100 per minute and blood pressure (systolic of 100-140 mmHg and diastolic of 60-90 mmHg). In addition to, the exclusion criteria were age less than 18 years or more than 55 years, body weight less than 50kg. Hemoglobin values less than 12.5 g/dl for female and 14 g/dl for male, history of jaundice, cupping, surgical operation, hypertension or current fever, recent illness or transfusion, and not giving consent.
Sampling method
The sample size calculated using Epi- info with an acceptable error fixed at three, confidence levels 99% and the prevalence of HBV was 5.1% [11]. The sample size comes to 311. We increased the sample by 10% to be 340 in order to overcome refusal of some of blood donors in the sample to participate due to their own reasons. A sampling frame was created using the blood donor register. The number of blood donations at NBTRC was an average of 1,300 per month. The sample was selected by using a simple random sampling method.
Data collection
Data were collected through face-to-face interview with blood donors by trained staff from NBTRC using a predesigned questionnaire that covers socio-demographic characteristics (e.g. age, sex, marital status), special habits (e.g. cigarette smoking, khat chewing), and past history (e.g. of jaundice, surgical operation, dental clinic visiting, cupping, hepatitis B vaccination, donate blood times, endemic area of malaria and urethro-vaginal excretion).
Laboratory test
Three to five ml whole blood samples were collected from each donor in a labeled plain and EDTA tubes with the unique identifier number. The serum was separated and screened for HBV, HCV, HIV by using a commercially available Electro-Chemi-Luminescence Immunoassay (ECLIA) Roche technique [15]. Any sample found reactive was retested for confirmation by using Bio Rad Kits ELISA. In addition, the samples were screened for syphilis and malaria antibodies by rapid immune-chromatographic assay method. Any unit found to be reactive was discarded.
Blood donors grouping and Rh factor were tested by used monoclonal antisera (serological method).
Data management and analysis
Data was entered and analyzed using Epi info 7.2 version where it was presented as frequencies and percentage. Cross-tabulation was used to identify associated factors with TTIs using the Chi-squared test (χ2) and odd ratio (OR). P-Value ≤ 0.05 is considered statistically significant.
Result
Three hundred-forty out of 2566 total blood donors recruited at the NBTRC during November and December 2017 were interviewed. Table 1 shows the blood donors according to scio- demographic information. Literate, male, and married formed the majority: 97%, 95%, and 77% respectively. Only 27% of the donors were VRCD. The most common age group was 26-35years (43%) and blood donors mostly came from Sana’a City (42%). Regarding special habits, 89% was Qat chewers and 53% was current smokers. There was no association between TTIs and gender, age groups, donation type, marital status, residence place, smoking or Khat chewing.
Table 2 O Positive (53.8%) and A Positive (29.7%) are the most encountered groups while the AB positive (0.6) is the least and there is no significant association between TTIs and blood grouping.
Table 3 shows that at 8.8% were reactive for any of TTIs tests and the most prevalent TTI marker was anti-malaria (3.2%) followed by HBsAg (2.5%). Only one donor sample had reactive results of multiple pathogens (co. infection).
Table 4 shows the significant associated factors with HBV, Malaria and syphilis. Multivariable analysis identified only past history of cupping [OR=4.8 (1.3-17.6), p<0.05], history of jaundice [OR=7.7 (2.1-27.8), p<0.01] and donating blood more than three times [OR=10.7 (1.3-85.3), p<0.01] found to be significantly associated with HBV infection.
Being from an endemic area was significantly associated with reactivity for malaria [OR=6.2 (1.6-23.8), p<0.01].
Regarding syphilis cases, urethra-vaginal excretion is significantly associated [OR=40.75 (5.08-326.8), P<0.001].

Table 1: Distribution of the blood donors by scio-demographic information and trans- fusion transmitted infections markers reactivity, National Blood Transfusion and Re- search Center, Sana’a City, 2017.
*VNRD: Voluntary Non-Remunerated Donors *FRD: Family Replacement Donors
**Khat is a plant, cultivated in Yemen, the young leaves and stems of khat are chewed for several hours for their stimulant action

Table 2: Distribution of TTIs by blood group types and Rh factors among blood do- nors at NBTRC, Sana’a city, 2017.
Discussion
TTIs remain an important cause of transfusion morbidity and mortality. Despite the advances that have been made in the testing of blood donations for infectious diseases, the risk of transmitting viral, bacterial, and parasitic diseases still exists. Thus, infectious complications of transfusion remain an important area of concern in transfusion medicine [1].

Table 3: Seroprevalence of Transfusion Transmitted Infections markers among blood donors, National Blood Transfusion and Research Center, Sana’a City, 2017.
* Only one donor had co-infection (HBV with HIV)
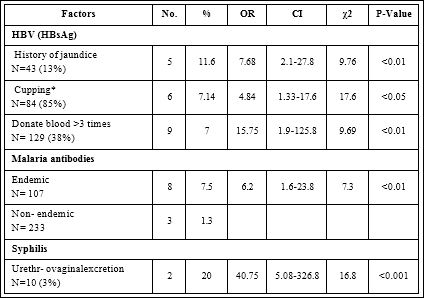
Table 4: Significant factors associated with HBV, malaria and syphilis reactivity among blood donors, National Blood Transfusion and Research Center, Sana’a City, 2017.
OR: Odd Ratio; CI: Confidence Interval; χ2: Chi-squared test
*Cupping: an operation of drawing blood from the body by scarification and cupping glass
In our study, the majority of the blood donors (95%) were males, which is mostly similar to the studies done in Yemen and Saudi Arabia [12,16]. This gender imbalance might be due to the fact that in these societies’ men are more proactive and independently make decisions. In addition, there may be misconceptions that donating blood by women may have a negative impact on their health due to their physiological repeated blood loss e.g. during pregnancy, menstruation etc. Thus, blood transfusion services authorities need to overcome such misconception through targeting women with clear health education messages on the benefits of blood donation even for women.
Thirty-four percent of donors in our study was 26-35 years, which is similar to previous studies in Yemen [9,17] as well as neighboring countries such as Ethiopia [4]. However, this differs from the figures published by the WHO that reported 45% of donors were aged 25 or less [18].This may be attributed to lack of awareness among younger age groups in the Yemeni population.
WHO advocates for developing national blood transfusion services based on VNR regular blood donation to ensure safe and adequate blood supply [19]. Our findings showed only 27% of blood donors are VNR that is similar to previous reports from Sana’a 27.4% [20] but contrasting the 100% VNR reported from Oman, Iran, and Qatar [21]. Such difference may reflects poor awareness and negative attitude among the Yemeni community regarding voluntary donation.
ABO blood distribution in this study showed that 53.8% of donors were O Rh positive that is quite similar with that reported from Ethiopia [22]. However, no significant association between ABO and TTIs was found.
In addition, our findings revealed that nearly half of the donors from Sana’a city which may be attributed to the location of NBTRC in Sana’a city. There is also no significant association between residence and TTIs.
This study showed that 29 units (8.8%) of donated blood had serological evidence of TTIs compared to 5.8% in Pakistan and 4.09% in India [23,24]. However, this increase in the prevalence of TTIs in our study may be attributed to the use of malaria antibodies in testing for malaria while the Pakistani and Indian studies used malaria antigen that usually gives lower prevalence. In addition, our findings showed nearly three-fourth of donations were replacement donors who had significantly higher TTIs prevalence than the voluntary donors which is similar to previous studies in other countries of the world [25,26].
Our study showed HBsAg prevalence of 2.5%, which is similar to previous results reported from Yemen that was ranging from 2.1% to 2.4% [9-11,17]. However, higher rates (5.1% and 6.7 %) have previously been reported among Yemeni blood donors [9,27] which may be either attributed to poor selection of donors or using fewer specific tests e.g. chromatography. Lower prevalence HBsAg rates was reported among Saudi blood donors (0.7%), Iraq (0.78) and Jordan (1.4%), respectively [28-29] that may be attributed to differences in the HBV epidemiology. Moreover, strong blood donor mobilization, selection, and retention and care systems in blood banks in those countries may play a more important role in such lower HBV prevalence.
Our study showed HCV prevalence 1.2% which is similar to previous studies in Yemen that was ranging between 0.8%-1.2% [9- 11,16]. However, our result was higher than reported from Saudi Arabia (0.4%), Iraq (0.2) and Jordon (0.9%) [28-30] which may reflects differences in HCV epidemiology.
The prevalence of HIV in our study (0.3 %) is slightly higher than reported from Hodeidah, Yemen: 0.14 % [11] and neighboring Saudi Arabia: 0.07% [28]. However, it is slightly lower than reported from Sana’a: 0.5% [17]. More research is still needed to explore reasons behind such differences.
Syphilis is a serious sexually transmitted disease that can be transmitted through blood transfusions [31]. In our finding, the prevalence of syphilis was 1.2% however, lower prevalence 0.34% was reported in Hodeidah, Yemen and from Saudi Arabia that may reflect geographical variation or in the testing methodology [11,32]. Nevertheless, much higher prevalence 6.8% was reported among Sudanese blood donors [33] that may relate to differences in behavioral risk factors. Our result revealed that past history of urethra-vaginal excretion is significantly associated with higher syphilis prevalence among blood donors (OR=40.75; 95% CI=5.08-326.8, P<0.001). Such a result is not unexpected considering that syphilis is a sexually transmitted disease that is frequently manifested by urethra-vaginal excretion.
Asymptomatic carriers of malaria are generally the source of transfusion-transmitted malaria infection. Asymptomatic infections may persist for five years especially in asymptomatic Plasmodium falciparum and vivax infections [34]. Our result showed the overall malaria antibody prevalence of 3.2%, which is higher than reported in Pakistan (0.07%) and India (0.03%)where malaria antigen tests were used [23,24]. Nevertheless, our results is lower than the overall prevalence of 7.6%, reported from Saudi Arabia [35] that could be attributed to use ELISA antibody tests while we used the rapid antibody test method. Our result showed a significant difference in malaria antibody among donors from endemic vs. non-endemic areas (7.5% vs. 1.3% respectively) which is consistent with findings from Saudi Arabia (9.1% vs. 4.8%).
This study showed that 29 units (8.8%) of donated blood had serological evidence of TTIs compared to 5.8% in Pakistan and 4.09% in India [23,24]. However, this increase in the prevalence of TTIs in our study may be attributed to the use of malaria antibodies in testing for malaria while the Pakistani and Indian studies used malaria antigen that usually gives lower prevalence.
TTIs were slightly progressively increasing with age, higher among males, married, illiterates and not employed where the differences are statistically insignificant (p>0.05). These findings are consistent with previous reports from Yemen and other countries [9,15,17].
Regarding associated factors with HBV, our finding showed HBsAg was significantly higher among blood donors who had previous history of cupping or jaundice. Similar result was previously reported among blood donors in Sana’a city [17]. Furthermore, donating blood more than three times found to be significantly associated with HBV infection, which may be an indication for possible healthcare- associated infection [36]. Furthermore, higher frequency of blood donation is related to paid donation - which is not uncommon in Yemen [37] that was found to be associated with higher rates of HBV markers [38].
We did not find any associations between HCV or HIV and any of potential factors e.g. blood transfusion. This may be due to lower prevalence of these infections in this study. Further studies with larger sample size should be considered.
Conclusions
The overall prevalence of viral infections among blood donors was drop compared with previous years and slightly increased for syphilis infections. While the prevalence of TTIs is low, it remains an important problem in blood transfusion. Therefore, establishment of TTIs surveillance system, improving donor motivation procedures and increasing the proportion of regular and voluntary donation together with using more sensitive screening methods are recommended. Increase public health awareness regarding TTIs and encouraging more research should be considered. Further studies over a longer period and with larger sample size should be also considered.
Declaration
Ethics approval and consent to participate
The study was approved by the Ethical Committee at the Ministry of Health and Population (12 February, 2018). Permission of the NBTRC was secured and verbal consent was taken from blood donors. Privacy was maintained during interviews, questionnaires kept in a lockable cabinet and data entered in a password-protected file in a computer with specific entrance code.
Consent for publication
Not applicable.
Availability of data and materials
The data presented in this paper are available from the corresponding author on request.
Competing interests
The authors declare that they have no competing interests.
Funding
This work was supported by TEPHNET, the funder had a role only in data collection.
Acknowledgment
Authors would like to acknowledge the TEPHNET for their support. They would also like to acknowledge the support of Y-FETP, EMPHNET, CDC and WHO.
References
- Manzoor I, Hashm NI, Daud S, Ajmal S, Fatima H, et (2009) Seroprev- alence of Transfusion Transmissible Infections (TTIS) in blood donors. Biomedica 25: 154-158.
- United States General Accounting Report to the Ranking Minority Member, CommiRee on Commerce, House of representative. Blood sup- ply, transfusion-associated risks. GAO/PEMD 1997: 97-102.
- Strategic framework for blood safety and availability 2016-2025. Cairo: World Health Organization Regional Office for the Eastern Mediterranean; 2017.
- Mohammed Y, Alemayehu B (2016) Seroprevalence of transfusion trans- mitted infection among blood donors at Jijiga blood bank, Eastern Ethio- pia: Retrospective 4 years BMC Res Notes 9: 129.
- Wairimu KM, Herbert K, John M (2016) Prevalence of (TTIs) among Blood Donated at Nyeri Satellite Transfusion Centre In IOSR Jour- nal of Pharmacy 6: 20-30.
- Blood safety and Fact sheet. Geneva: World Health Organiza- tion 2017.
- World malaria Geneva: World Health Organization 2017.
- Kumar A, Valecha N, Jain T, Dash AP (2007) Burden of malaria in India: Retrospective and prospective view. The American journal of tropical med- icine and hygiene 77: 69-78.
- Alodini AQ (2014) Prevalence of Hepatitis B Virus (HBV) and Hepatitis C Virus (HCV) Infections among Blood Donors at AlThawra Hospital Sana’a City Yemen. Yemeni journal for medical sciences 6: 16-20.
- Al-Waleedi A.A, Khader YS (2012) Prevalence of hepatitis B and C in- fections and associated factors among blood donors in Aden city, Eastern Mediterranean Health Journal 18: 624- 629.
- Saghir SA, Al–Hassan FM, Alsalahi OS, Abdul-Alaziz AE, Baqir HS (2012) Frequencies of HBV, HCV, HIV, and Syphilis Markers Among Blood Do- nors: A Hospital-Based Study in Hodeidah, Yemen. Tropical Journal of Pharmaceutical Research February 11: 132-136.
- Saghir SAM, Alsalahi OSA, Zabad AAM, Al-Hassan FM (2012) HIV and Syphilis among Blood Donors in Sana’a, Biohealth Science Bulletin 4: 24-27.
- Nada S, Alhweesh M, Al-harazi T, Alkadasi M, Zaid AA (2014) Diagnostic study on plasmodium in blood bags at Taiz City, Int J Curr Micro- biol App Sci 3: 635-43.
- Guidelines on Assessing Donor Suitability for Blood Donation. Geneva: World Health Organization 2012.
- Roche Diagnostics Products and solutions, 2015.
- El-Hazmi M (2004) Prevalence of HBV, HCV, HIV-1, 2 and HTLV-I/II in- fections among blood donors in a teaching hospital in the Central region of Saudi Arabia. Saudi Med J 25: 26-33.
- Amar G (2017) Prevalence of Major viral blood-borne infections among blood donors at National blood transfusion and research center in Sana’a city-Yemen. MSc Faculty of Medicine and Health Sciences, Sana’a Yemen.
- Teo KS, Saparudin MS, Zain Z, Morshidi MA, Metassan N, et al. (2011) Transfusion transmissible infections in Brunei Darussalam: A blood donor Brunei Int Med J 7: 321-327.
- Voluntary blood Geneva: World Health Organization 2010.
- Al-Zubiery, Alharazi T, Alsumairy H, Jabir AA, Muckbil MJ, et (2017) Sero-prevalence of Anti- HCV among Yemenis Blood Donors Attending National Blood Transfusion and Research Centre in Sana’a: Yemen. IBRR 7: 1-6.
- The regional status report on blood safety and availability. Cairo: World Health Organization Regional Office for the Eastern Mediterranean 2016.
- Wakjira K, Mekonnen Z, Gerbi A, Abebe G (2017) Transfusion-transmis- sible infection surveillance among blood donors in Southwest Ethiopia. Asian Pac J Trop Dis 7: 156-161.
- Arshad A, Borhany M, Anwar N, Naseer I, Ansari R, et al. (2016) Prev- alence of transfusion transmissible infections in blood donors of Paki- BMC hematology 16: 27.
- Sharma DC, Rai S, Bharat S, Iyenger S, Gupta S, et (2014) Transfusion Transmissible Infections among Blood Donors at the Blood Bank of Medi- cal College of Gwalior: A 5 Year Study 5: 236-246.
- Mujeeb SA, Mahmood T (1996) Prevalence of HBV, HCV and HIV infec- tions among family blood donors. Ann Saudi Med 16: 702-703.
- Sultan F, Mehmood T, Mahmood MT (2007) Infectious Pathogens in volunteer and replacement blood donors in Pakistan: A ten year experi- Intern J Infect Dis 11: 407-412.
- Haidar NA (2002) Prevalence of hepatitis B and hepatitis C in blood donors and high-risk groups in Hajjah, Yemen Republic. Saudi Medical Journal 23: 1090-1094.
- Elbjeirami WM, Arsheed NM, Al-Jedani HM, Elnagdy N, Hazem M, et (2015) Prevalence and Trends of HBV, HCV, and HIV Serological and NAT Markers and Profiles in Saudi Blood Donors. J Blood DisordTransfus 6: 280.
- Rasheed Hussein N, Mohamad Haj S, Amin Almizori L, Ahmed Taha A (2017) The Prevalence of Hepatitis B and C Viruses Among Blood Donors Attending Blood Bank in Duhok, Kurdistan Region, Iraq, Int J Infect 4: e39008.
- Al-Gani FA (2011) Prevalence of HBV, HCV and HIV-1, 2 infections among blood donors in Prince Rashed Ben Al-Hassan Hospital in North Region of Int. J. Biol. Med. Res 2: 912-916.
- Elyamany G, Al amro M, Pereira W, Alsuhaibani O (2016) Prevalence of Syphilis among Blood and Stem Cell Donors in Saudi Arabia. Electronic Physician 8: 2747-2751.
- Kim JK, Choi SR, Lee HJ, Kim DH, Yoon MS, et al. (2011) Conngenital syphilis presenting with a generalized bullous and pustular eruption in a premature newborn. Ann Dermatol 1: 127-30.
- Bazie EA, Ali MA, Hamza HB, Omer Saeed Magzoub OS, Salih MS, et (2015) Sero-Prevalence of HIV and Syphilis Infections among Blood Do- nors at Kosti Teaching Hospital-White Nile State-Sudan. Int J Curr Micro- biol App Sci 4: 832-837.
- Katz LM (2003) Transfusion-induced malaria. In: Brecher ME, ed. Bac- terial and parasitic contamination of blood components. Bethesda, MD: AABB Press 127-155.
- Saeed AA, Al Rasheed AM, Al Nasser I, Al Onaizi M, Al Kahtani S, et al. (2002) Malaria screening of blood donors in Saudi Arabia. Annals of Saudi medicine 22: 329-332.
- Moorman AC, Stramer SL, Schaefer MK, Collier MG, Suryaprasad A, et (2015) Incident hepatitis among repeat blood donors; A sentinel event signaling possible healthcare associated infection and need for reporting to public health authorities. Transfusion 55: 2531-2533.
- Darbandi A, Mashati P, Yami A, Gharehbaghian A, Namini MT, et al. (2017) Status of blood transfusion in World Health Organization-Eastern Mediterranean Region (WHO-EMR): Successes and Transfu- sion and Apheresis Science 56: 448-453.
- Van Der poel, CL, Seifried E, Schaasberg WP (2002) Paying for blood do- nations: Still a risk? Voxsanguinis 83: 285-293.
Citation: Ghaleb YA, Alshahari AZ, Ali MA, Al-Amad MA, Al-Serouri AA (2021) Transfusion Transmitted Infections: Prevalence and Associated Factors, National Blood Transfusion and Research Center, Sana’a Capital, Yemen. J Hematol Hemother 6: 015.
Copyright: © 2021 Ghaleb YA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and re- production in any medium, provided the original author and source are credited.