*Corresponding Author:
Guy HEJ Vijgen,
Department of Surgery, Franciscus, Netherlands
E-mail: guy.vijgen@gmail.com
Abstract
Background: The aim of this study was to evaluate a cohort Lapa- roscopic Sleeve Gastrectomy’s (LSGs) converted into Laparoscopic Roux-en-Y Gastric Bypass (LRYGB). Furthermore, the effect of ei- ther additionally reducing the size of the gastric pouch or not during conversion into LRYGB was determined.
Methods: All patients who underwent revision of a LSG into a LRYGB, due to inadequate weight loss or substantial weight regain, in our center were identified in a retrospective analysis.
Results: 42 patients qualified for analysis and were included in this study. The mean follow up after revisional LRYGB was 27.7±11.2 months (range, 7.3-45.3 months). The mean BMI before LRYGB was 40.1±5.3 kg/m2. A decrease in BMI was observed at 2 and 3years of follow-up after conversion into a LRYGB; 34.2±5.9 kg/m2 and 35.1±8.0 kg/m2 respectively (P<0.05). Subgroup analysis of pa- tients with a non-reduced gastric pouch (n=25) versus patients with a reduced gastric pouch (n=17) showed no significant differences in base line characteristics or in additional weight loss between the two groups (P≥0.05).
Conclusion: Conversion of a primary LSG into a LRYGB in patients with inadequate weight loss or weight regain resulted in significant weight loss. Additional gastric pouch reduction did not further in- crease weight loss.
Keywords
Conversion; Laparoscopic sleeve gastrectomy; Laparo- scopic Roux-en-Y Gastric bypass
Introduction
Laparoscopic Sleeve Gastrectomy (LSG) is well accepted as a stand-alone bariatric procedure and currently, after Laparoscopic Roux-en-Y Gastric Bypass (LRYGB), the second-most performed bariatric procedure worldwide showing a rise in prevalence from 0% in 2003 to 37% of the world total (n=468.609) in 2013 [1]. A drawback of this procedure is that in approximately 15% of patient’s inadequate weight loss, substantial weight regains or gastroesophageal reflux fol- lowing the primary procedure is observed necessitating revisional surgery [2-5]. Several revisional procedures such as resizing the sleeve [6,7], banding of the sleeve [8], conversion of the sleeve into a gas- tric bypass [9,10], a mini gastric bypass [11], duodenal switch [12] or single anastomosis duodeno-ileal bypass with sleeve gastrectomy (SADI-S) [13] have been proposed to achieve further weight loss.
In case of revision into a LRYGB, gastric pouch creation may be performed by ‘transecting the sleeve only’ or with additional calibra- tion of the often-dilated gastric pouch in vertical direction to reduce the size of the pouch. Smaller sized pouches in LRYGB have been as- sociated with better weight loss [14]. Revision of a LSG into a LRYGB was initially not routinely performed with reduction of the gastric pouch in our institute as well as in others [9,10]. Hence, we analyzed both LRYGB revisions with and without reduction of the gastric Pouch in our center. Subgroup analysis was performed to assess the additional effect of gastric pouch reduction during conversion into a LRYGB.
Materials and Methods
Patients
From March 2008 to September 2014, 84 consecutive patients underwent conversion of a LSG into a LRYGB in our center. All patients who met the Reinhold criteria modified by Christou, defined as BMI ≥35 or <50% EWL, were considered as inadequate weight loss or substantial weight regain 1 year after primary surgery and were potential candidates for revisional surgery in our center [15,16]. Patients who underwent conversion from LSG into LRYGB due to inadequate weight loss or weight regain and with at least one year of follow up after the revisional procedure were included in the current analysis, resulting in a cohort of 42 patients. Informed consent was obtained from all patients. This retrospective study did not require medical ethical approval of the Institutional Review Board of Franciscus.
Surgical technique
All primary LSG procedures were performed in our center as described in detail before [17]. During the initial procedure in all patients received 34 French bougie used. After maximal dietician and psychological counseling, patients were discussed in a multidisciplinary bariatric meeting prior to being scheduled for revisional surgery. Conversion from LSG to LRYGB was independently performed by two surgeons using a 5-trocar technique similar to primary LRYGB as described by Leifsson et al [18]. The sleeve was transected between the first and second gastric vessel using a linear stapler Echelon 60 mm. One of the surgeons standardly reduced the diameter of the gastric pouch also stapling it in vertical direction along a 34 French bougie, whereas the other did not. Since patients were randomly assigned to a surgeon, they were also randomly allocated a reduced or non-reduced gastric pouch. Pouch volumetric was not performed. The 3 cm long linear gastro jejunostomy was created with the Echelon 60 mm gold cartridge. The biliopancreatic limb of 60 cm and the alimentary limb of 150 cm were standard like in a primary LRYGB procedure for both surgeons.
Data collection
Our prospective database of bariatric procedures contained patient records about the primary procedure (LSG). Information about the revisional procedure (LRYGB) was retrospectively retrieved from the written and electronic patient records. Outpatient and clinical data on the primary and the revisional procedure were obtained starting from the preoperative primary LSG visit up to 3 years after the revisional LRYGB procedure. The primary outcome parameters were body weight (kg), body-mass index (BMI), percentage excess BMI loss (%EBMIL) and percentage total weight loss (%TWL).
Statistical analysis
All analyses were performed using SPSS (PASW) 18.0 software (SPSS Inc., Chicago, Illinois, USA). Reported data are expressed as mean ± standard deviation (SD) for continuous variables and as percentages for categorical variables. Excess BMI Loss (EBMIL) is expressed as %EBMIL = 100 [(follow-up BMI 25/ starting BMI before LSG - 25) x 100]. Total Weight loss (TWL) is expressed as %TWL = [(starting weight before LSG final weight) / starting weight before LSG] x 100. Group parameters at different time points were compared using paired Student’s t-tests. Differences within the group were compared using unpaired Student’s t-tests. Univariate logistic regression with Student’s t-test was performed to define the effect of calibration of the pouch on weight loss; p-values below an alpha of 0.05 were considered to be statistically significant.
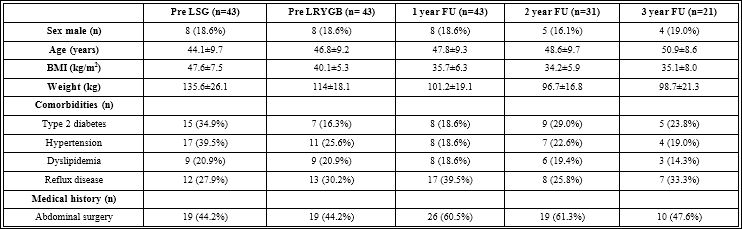
Table 1: Baseline characteristics.
Data was expressed as mean ±SD or as absolute numbers with its percentage of the subgroup. N: Number; kg/ m2: Kilograms per Square Meter; BMI: Body Mass Index.
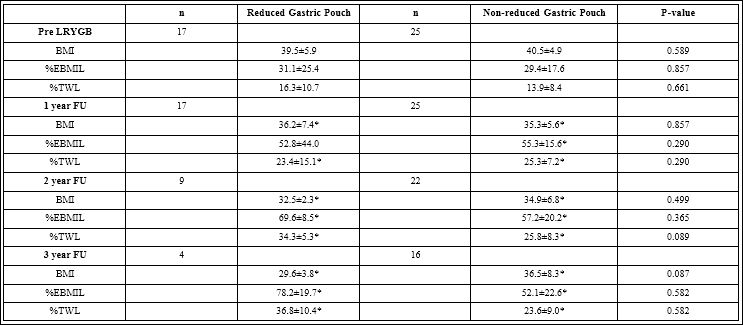
Table 2: Weight loss results.
Data was expressed as mean ±SD.
Group differences were tested using nonparametric tests.
*P<0.05 Compared to Pre-LRYGB using paired samples t-test.
Results
A total of 1343 primary LSGs were performed between Septem- ber 2006 and August 2014. Our cohort (n=42, 3.1% of the total, Table 1) represents a large part of our known group of patients converted into LRYGB after LSG (n=84, 50%). Actively contacting our patients to increase follow-up rates resulted in follow-up percentages of 100%, 73.8% and 50% for follow-up terms of respectively 1, 2 and 3 years; these rates were equally distributed over both groups.
Indications for revision were in adequate weight loss or substantial weight regain after LS Gas defined by the Reinhold criteria. [12]. The revisional procedure was performed after a mean period of 33.3±15.6 months (range, 16.1 - 63.2 months). The mean preoperative BMI was 40.1±5.3 kg/m2 (range, 30.2-58.1 kg/m2) (Table 1&2).During the re- visional procedure 17 (40.5%) patients received a LRYGB with a re- duced gastric pouch and 25 (59.2%) patients received a LRYGB with a non-reduced gastric pouch (Table 2). Mean operative time for LRYGB with or without gastric pouch reduction was 79.9±31.9 minutes (range 41-159 minutes) and 108±44.7 minutes (range, 46-215 minutes) re- spectively. Intra-operative complications did not occur and postop- erative complications during admission were not observed. The mean length of hospital stay was 2.3±1.7 days (range, 1-10 days). None of the patients passed away within the first 30 postoperative days. After revi- sion, 4 patients with an uncalibrated pouch required a 2nd revision for persistent weight loss failure. 3 of these 4 patients received a secondary calibrated pouch.
The mean follow-up period after LRYGB was 27.7±11.2 months (range, 7.3-45.3months).Although a significant decrease in mean BMI Total group was not observed at 1 year of follow-up (35.7±6.3 kg/m2, P>0.05), it was observed at 2 years (34.2±5.9 kg/m2, P<0.05), and 3 years (35.1±8.0 kg/m2, P<0.05) of follow-up (Table 2).The mean %EBMIL Total group and the mean %TWL Total group significantly increased from, respectively, 31.4% and 15.4% to 56.9% and 25.5% at 1 year of follow-up and remained stable thereafter.
Additional analyses were performed for two subgroups; patients with a reduced gastric pouch (n=17) and patients with a non-re- duced gastric pouch (n=25) (Table 2). A significant decrease in BMI (from 39.7±6.0 kg/m2 to 35.9±7.5 kg/m2) as well as increase in %EB- MIL (from 34.2±22.4% to 59.1±35.7%) and increase in %TWL (from 16.6±9.3% to 25.7±11.8%) was observed for patients with a reduced gastric pouch at 1 year of follow-up. All 3 parameters showed fur- ther improvement thereafter (P<0.05). In contrast to patients with a non-reduced gastric pouch, who also achieved a significant decrease in BMI (from 40.5±4.9 to 35.3±5.6 kg/m2) as well as an increase in %EBMIL (from 29.4±17.6 to 55.3±15.6) and %TWL (from 13.9±8.4 to 25.3±7.2) at 1 year of follow-up, but remained stable thereafter with values significantly better as compared to before revisional surgery. In conclusion, no significant differences were observed in additional weight loss in patients with a reduced gastric pouch versus patients with a non-reduced gastric pouch.
Discussion
With increasing numbers of bariatric procedures being performed globally, the number of patients who do not achieve the desired weight loss also rises, regardless of the applied procedure. Thus, an important aspect of bariatric surgery is revisional surgery. As LSG is currently the most frequent performed procedure worldwide [1], the question arises which secondary procedure would be most effective in achieving additional weight loss in case of inadequate weight loss or substantial weight regain. Consensus regarding this matter has not yet been established and inadequate weight loss and weight regain remain a concern for both the patient and the bariatric surgeon.
Reports on conversion of LSG to LRYGB are limited, discuss small numbers of converted patients and also include revisions of gastroesophageal reflux after LSG. Gautier et al. [9] reported on 18 conversions of which 9 nine were due to insufficient weight loss; an additional BMI decrease from 40.9 kg/m2 before revision to 35.8 kg/m2 was observed within FU 3.6-31.1 months. Langer et al. [10] reported on 8 revisions of LSG into LRYGB of which 5 for weight regain. After conversion, a mean weight reduction of 15.2±8 kg was achieved within FU 1-52 months. Since then, several other reports on revisional surgery after primary LSG have been published aiming to increase insight into which revisional procedure yields the best results in terms of additional weight loss [5,19-32]. This data has, currently, not yet been merged and analyzed in a meta-analysis.
This report describes 42 patients who underwent conversion from LSG into LRYGB (with or without gastric pouch reduction) due to inadequate weight loss or weight regain. A non significant decrease in BMI was observed for the total group at1 year of follow-up, whereas a significant decrease in BMI was observed at 2 and 3 years of follow-up (compared to before LRYGB). A decrease in BMI was, however, mainly observed during the first postoperative year and remained stable thereafter. Interestingly, continued weight loss was only observed in patients with a reduced gastric pouch. In conclusion, revision from LSG into LRYGB in patients with inadequate weight loss or weight regain resulted in significant additional weight loss. Additional gastric pouch reduction did not further increase weight loss.
Limitations of this study were the retrospective design, which makes the results subjective to bias and the limited follow-up. Despite these limitations we report on a large cohort of conversions due to inadequate weight loss or weight regain. Additional prospective re- search of larger cohorts with longer follow-up is required to properly assess which conversion technique is the most effective in achieving additional weight loss after primary LSG.
References
- Angrisani L, Santonicola A, Iovino P, et (2017) Bariatric Surgery and Endo- luminal Procedures: IFSO Worldwide Survey 2014. Obes Surg.
- Sjöström L, Lindroos AK, Peltonen M, et al. (2014) Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric N Engl J Med 351: 2683-2693.
- Himpens J, Dobbeleir J, Peeters G (2010) Long-term results of laparoscopic sleeve gastrectomy for obesity. Ann Surg 252: 319-324.
- Gadiot RP, Biter LU, van Mil S, et al. (2017) Long-Term Results of Lapa- roscopic Sleeve Gastrectomy for Morbid Obesity: 5 to 8-Year Results.Obes Surg 27: 59-63.
- Malinka T, Zerkowski J, Katharina I, et al. (2017) Three-Year Outcomes of Revisional Laparoscopic Gastric Bypass after Failed Laparoscopic Sleeve Gastrectomy: a Case-Matched Analysis. Obes Surg 27: 2324-2330.
- Baltasar A, Serra C, Pérez N, et al. (2006) Re-sleeve gastrectomy. Obes 16:1535-1538.
- Noel P, Nedelcu M, Nocca D, et al. (2014) Revised sleeve gastrectomy: an- other option for weight loss failure after sleeve gastrectomy. Surg Endosc. 28: 1096-1102.
- Greenstein AJ, Jacob BP (2008) Placement of a laparoscopic adjustable gas- tric band after failed sleeve gastrectomy. Surg Obes Relat Dis. 4: 556-558.
- Gautier T, Sarcher T, Contival N, et (2013) Indications and mid-term results of conversion from sleeve gastrectomy to Roux-en-Y gastric bypass. Obes Surg. 23: 212-215.
- Langer FB, Bohdjalian A, Shakeri-Leidenmühler S, et al.(2010) Conversion from sleeve gastrectomy to Roux-en-Y gastric bypass--indications and out- Obes Surg.20: 835-840.
- Moszkowicz D, Rau C, Guenzi M, et (2013) Laparoscopic omega-loop gas- tric bypass for the conversion of failed sleeve gastrectomy: early experience. J Visc Surg. 150: 373-378.
- Gumbs AA, Pomp A, Gagner M (2007) Revisional bariatric surgery for inade- quate weight loss. Obes Surg.; 17: 1137-1145.
- Sánchez-Pernaute A, Rubio Herrera MA, et al. (2007) Proximal duodenal-il- eal end-to side bypass with sleeve gastrectomy: proposed technique. Obes 17: 1614-1618.
- Roberts K, Duffy A, Kaufman J, et (2007) Size matters: gastric pouch size correlates with weight loss after laparoscopic Roux-en-Y gastric bypass. Sur- gEndosc.21: 1397-1402.
- Reinhold RB (1982) Criticalanalysis of longtermweight lossfollowing gastric Surg Gynecol Obstet. 155: 385-394.
- Christou NV, Look D, Maclean LD (2006) Weight gain after short- and long- limb gastric bypass in patients followed for longer than 10 years. Ann Surg. 244: 734-740.
- Gadiot RP, Biter LU, Zengerink HJ, et al. (2012) Laparoscopic sleeve gas- trectomy with an extensive posterior mobilization: technique and preliminary Obes Surg.22: 320-329.
- Leifsson BG, Gislason HG (2005) Laparoscopic Roux-en-Y gastric bypass with 2 meter long biliopancreatic limb for morbid obesity: technique and expe- rience with the first150 patients. Obes Surg. 15: 35-42.
- van Rutte PW, Smulders JF, de Zoete JP, et (2012) Indications and short- term outcomes of revisional surgery after failed or complicated sleeve gas- trectomy. Obes Surg. 22: 1903-1908.
- Carmeli I, Golomb I, Sadot E, et (2015) Laparoscopic conversion of sleeve gastrectomy to a biliopancreatic diversion with duodenal switch or a Roux- en-Y gastric bypass due to weight loss failure: our algorithm. Surg Obes Relat Dis. 2015; 11: 79-85.
- Homan J, Betzel B, Aarts EO, et al. (2015) Secondary surgery after sleeve gastrectomy: Roux-en-Y gastric bypass or biliopancreatic diversion with duo- denal switch. Surg Obes Relat Dis. 11: 771-777.
- Abdemur A, Han SM, Lo MenzoE, et al. (2016) Reasons and outcomes of conversion of laparoscopic sleeve gastrectomy to Roux-en-Y gastric bypass for non responders. Surg Obes Relat Dis. 12: 113-118.
- Al-Sabah S, Mulla AA, Vaz JD (2017) Revisional laparoscopic sleeve gastrec- tomy after Primary Obesity Surgery Endolumenal (POSE). Surg Obes Relat 13: 899-900.
- Casillas RA, Um SS, Zelada Getty JL, et (2016) Revision of primary sleeve gastrectomy to Roux-en-Y gastric bypass: indications and outcomes from a high-volume center. Surg Obes Relat Dis. 12: 1817-1825.
- Felsenreich DM, Langer FB, Kefurt R, et (2016) Weight loss, weight regain, and conversions to Roux-en-Y gastric bypass: 10-year results of laparoscopic sleeve gastrectomy. Surg Obes Relat Dis. 12: 1655-1662.
- Greco F (2017) Conversion of Vertical Sleeve Gastrectomy to a Functional Single Anastomosis Gastric Bypass: Technique and Preliminary Results Us- ing a Non-Adjustable Ring Instead of Stapled Division. Obes Surg. 27: 896-901.
- Iannelli A, Debs T, Martini F, et (2016) Laparoscopic conversion of sleeve as trectomy to Roux-en-Y gastric bypass: indications and preliminary results. Surg Obes Relat Dis. 12: 1533-1538.
- Poghosyan T, Lazzati A, Moszkowicz D, et al. (2016) Conversion of sleeve gastrectomy to Roux-en-Y gastric bypass: an audit of 34 Surg Obes Relat Dis.12: 1646-1651.
- Quezada N, Hernández J, Pérez G, et al. (2016) Laparoscopic sleeve gas- trectomy conversion to Roux-en-Y gastric bypass: experience in 50 patients after 1 to 3 years of follow up. SurgObesRelat Dis. 12: 1611-1615.
- El Chaar M, Stoltzfus J, Claros L, et al. (2017) Indications for Revisions Fol- lowing 630 Consecutive Laparoscopic Sleeve Gastrectomy Cases: Experi- ence in a Single Accredited Center. JG as Surg. 21: 12-16.
- Parmar CD, Mahawar KK, Boyle M, et al. (2017) Conversion of Sleeve Gas- trectomy to Roux-en-Y Gastric Bypass is Effective for Gastro-Oesophageal Reflux Disease but not for Further Weight Loss. Obes Surg. 27: 1651-1658.
- van Wezenbeek MR, van Oudheusden TR, de Zoete JP, et al. (2017) Con- version to Gastric Bypass After Either Failed Gastric Band or Failed Sleeve Obes Surg. 27: 83-89.
Citation: Vijgen GHEJ, Birbal RS, Apers JA, van Mil S, Biter LU, et al. (2018) The Importance of Gastric Pouch Reduction in Conversion of Laparoscopic Sleeve Gastrectomy into Roux-en-Y Gastric Bypass. J Obes Bod Weig 1: 001.
Copyright: © 2018 Vijgen GHEJ. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.