*Corresponding Author:
Nasibova EM,
Azerbaijan Medical University, Baku, Azerbaijan
Email: doc.nasibova.esmira@gmail.com
Abstract
The problem of premedication becomes especially significant in pediatric anesthesiology, since the change of environment associated with placing the child in a hospital, the absence of parents, unfamiliar faces all this leads to a sharp arousal of the child, accompanied by significant changes in the activity of vital organs and systems.
The aim of the study: optimization of anesthetic benefits in one-day surgery in children by incorporating midazolam into premedication.
Material and research methods: Midazolam at a dose of 0.4 mg/kg per os or 0.3 mg/kg intramuscularly 20 minutes before anesthesia was used as a sedative drug for sedation. The necessity of prescribing a sedative drug in premedication was determined individually and was guided by the obtained data of the Kerdo vegetative index.
The results of the study: Analysis of the depth of sedation showed that 5 minutes after sedation in 7 children (8.4%), the degree of sedation was at the RO level, and in 67 children (80.7%) at the RI level, in 9 children (10.8%) at R2 level. After 10 minutes, 72.3% of the children began to experience drowsiness, but at the same time they were in contact, performed simple commands, opened their eyes to treatment, which corresponded to the R3 degree of sedation. The remaining 27.7% of the children did not experience drowsiness, while they were calm and contact (sedation degree R2). At the 20th minute of the study, 84.3% of the children reached R3 sedation. And 15.7% of children at the time of separation from their parents corresponded to degree R2.
Thus, in the light of the above information, each anesthetist should carefully plan all aspects of the preoperative introduction of each individual child, including premedication means in this plan, if there is a clear need for them. The point of view of some doctors “applying” standard premedication is extremely erroneous, since there are no two identical patients. It is necessary to choose the method of sedation that is optimal and ideal for the child.
Keywords
Midazolam; One-day surgery; Sevoflurane
Introduction
The problem of premedication becomes especially significant in pediatric anesthesiology, since the change of environment associated with placing the child in a hospital, the absence of parents, unfamiliar faces all this leads to a sharp arousal of the child, accompanied by significant changes in the activity of vital organs and systems. By premedication is understood the medical preparation of the patient for general anesthesia, aimed at eliminating the fear and anxiety associated with the upcoming operation. Premedication is necessary to solve the following problems: reducing emotional arousal, neuro-vegetative stabilization, reducing reactions to external stimuli, creating optimal conditions for analgesics, preventing allergic reactions to drugs used in anesthesia, reducing the secretion of glands, reducing the volume of gastric juice and increasing its pH, antiemetic effect, reduced need for anesthetics, easier induction. The basis of premedication is reliable protection of the patient from preoperative emotional stress, the inevitable consequence of which is a complex of soma to vegetative disorders called “cerebrovisceral syndrome of emotional stress”: activation of the sympathetic-adrenal and hypothalamic-pituitary-adrenal systems, hyper dynamic reactions of the blood circulation, activation of respiration and respiratory and especially carbohydrate [1-6].
Features of “one-day surgery”, hospitalization on the day of surgery, educational programs with parents and game therapy with children can also reduce emotional stress before anesthesia and surgery. Despite the success of these methods of preparation for surgery, medications are often prescribed for premedication. Recently, the need for drug premedication has often been called into question [7,8]. However, according to Kain et al. [9], about 70% of children experience stress and excitement before surgery. Sedative sedation is most appropriate for young patients with whom it is difficult to find contact, especially in children aged 1-3 years [8]. Also, sedation is often required for patients who have conscious experience of painful manipulation. The development of distress during induction significantly increases the risk of arousal and anxiety upon awakening, as well as nightly fears [10]. According to Kain and other researchers, the cry, crying and anxiety of children before surgery contributes to the development of postoperative complications such as arousal syndrome after waking up, inappropriate behavior and increased postoperative pain [10-12]. Also, some researchers note that an increased level of preoperative anxiety activates the pathophysiological reactions of the body in response to stress, leading to an increase in glucocortocoid levels and increased susceptibility to postoperative infections [9,13]. Children older than 3 years who are in good contact with the anesthesiologist after a detailed explanatory conversation with him are not given sedative sedation. This is especially true if one of the parents is possible during induction, which is increasingly practiced in medical centers. It is also suggested that sedative sedation may be more effective in eliminating anxiety during anesthesia than the presence of parents. However, not all children need premedication.
There are three groups of children for who premedication is strictly required:
- 1.Children with an unfavorable prognosis of
- 2.Children with a satisfactory prognosis of behavior, but in whom, despite carrying out the whole complex of measures to reduce reactive anxiety, a pronounced negative attitude towards intervention
- 3.Children with impaired mental development, organic lesions of the nervous system, mental illness.
Drug premedication should be performed in children only after a comprehensive and careful assessment of all sides of the patient and the upcoming operation. There are no standards for child sedation. When deciding on the appointment of such drugs, it is necessary to remember not only the initial and positive effect, but also the possibility of a subsequent side effect, which negates their advantages. Nausea and vomiting, itching and, in rare cases, respiratory depression following the administration of narcotic analgesics are a good example of this premedication effect [11]. Despite this, opioids are very suitable for children who need preoperative analgesia, eliminating pain and anxiety and providing sedation.
The methodology for premedication should also be carefully provided. Routes of administration of drugs in children are one of the priority problems of sedation. The following routes of drug administration are widely used: 1) intravenous; 2) intramuscular; 3) oral; 4) rectal; 5) intranasal; 6) sublingual; 7) intradermal.
Intravenous administration for sedation is justified only in cases when a catheter is pre-installed in a vein. In other cases, this is the inevitable stressful state of the child and the consolidation of an unpleasant episode in his mind, which is extremely unfavorable for subsequent procedures. The second serious reason for limiting venous access to sedation is the possible side effect of certain drugs (opiates, ketamine, propofol) in the form of respiratory depression, which requires mandatory monitoring of respiration or, more efficiently, the use of pulse oximetry to determine the level of oxygen saturation (SpO2). Intramuscular administration is also negatively perceived by children. When taking drugs orally, the following points should be considered: 1) avoid bitter and concentrated solutions; 2) do not prescribe the drug by mouth after eating the drug dissolves in the gastric contents and is absorbed much more slowly, and a gag reflex is possible immediate and delayed. The child will not take a bitter preparation a second time in his mouth; therefore the best way is to dilute the calculated dose in 5% fruit syrup. A concentrated solution can cause not only vomiting, but also diarrhea (with high osmolarity of the solution). Many anesthetists are still opposed to oral medication for sedation, believing that getting the drug into the stomach causes immediate secretion of gastric juice, which can become dangerous due to possible regurgitation and aspiration of the contents. But numerous literatures shows that in recent years this has been treated with less concern, especially in cases where the patient needs only sedation during one of the types of regional anesthesia, and not anesthesia with the introduction of muscle relaxants and endotracheal intubation [913].
With the rectal administration of drugs, two important conditions should be observed: 1) add enveloping substances to a solution that has an irritating effect (for example, chloral hydrate); 2) do not enter through the catheter metabolized in the liver, too deep above the level of the rectum in order to avoid getting the drug into the portal system and its rapid elimination. We know that in the rectum, venous outflow is carried out in two main ways: i.v.haemorrhoidalis superiors flow into the portal vein, and therefore drugs are sent to the liver, where they are metabolized. By i.v.haemorrhoidalis inferior, which flow directly into the inferior vena cava, drugs enter the systemic circulation and thereby achieve a higher concentration in the central nervous system. Water-soluble forms of drugs for rectal administration are also recommended. The advantages of rectal administration of drugs for sedation include the following qualities: 1) the route of administration of drugs is painless; 2) upon the occurrence of sleeping pills, it is easy to pick up the child from the parents; 3) in a sleeping child, it is easier to carry out inhalation anesthesia through a mask; 4) independent rectal anesthesia or sedation is a non-polluting method [11,13].
The intranasal route of administration of sedation drugs, especially in young children, has an advantage over the oral route according to two criteria: 1) the child may flatly refuse oral administration of the drug; 2) the dose for oral administration is higher, since the drug enters the liver, where it is metabolized. The disadvantage of intranasal administration of drugs, in particular midazolam, is irritation of the nasal mucosa.
There are different options for sedation. A lot of research has been done on the use of different options for sedation. For example, in the treatment of teeth in 356 adult patients, ketamine was used intramuscularly for sedation and a positive assessment of its effect by patients and doctors was noted [8,9]. The administration of benzodiazepines in combination with the intravenous administration of ketamine to 60 patients during their transcutaneous renal biopsy provided deep sedation [5,7,8]. As a sedation, 40 children with dental treatment were prescribed either midazolam per os (0.5 mg/kg) or ketamine (5 mg/ kg) on an outpatient basis, and in all of them sedation occurred after 20 minutes, but the patients were discharged earlier treated with ketamine [10]. Surgical interventions lasting more than 30 minutes on an outpatient basis for 120 children (with pre-sedation with ketamine per os (3 mg/kg) or combined use of both drugs showed that in the latter case sedation occurred in 90% of patients with midazolam in 70%, and with ketamine in 51% of patients [10,11,13]. The study showed that in conditions of one-day surgery, 68 children from the age of 4 months up to 17 years, 350 diagnostic procedures were performed (lumbar puncture, puncture and taking a bone marrow biopsy), radiation therapy, etc., while sedation was carried out by intravenous administration of midazolam then ketamine in a dose of 1-2 mg/kg. At the same time, good sedation was noted, but in 1.1% of cases, a decrease in Hb oxygen saturation was observed (18). According to some studies, if the tone of the parasympathetic nervous system prevails in patients (92 patients) in a one-day hospital, then they should be prescribed atropine (0.015 mg/kg), relanium (0.1-0.15 mg/ kg) and ketamine (1 -2 mg/kg), with hyper sympathicotonia atropine (0.015 mg/kg) and relanium (0.1-0.15 mg/kg), and with normal sympathicotonia atropine (0.01 mg/kg) and relanium (0.1 mg/kg) [11]. Therefore, when prescribing premedication, VIC should be taken into account, which allows one to assess the prevalence of paraor sympathicotonia in the patient [1,5,7-9,13].
In recent years, the sedative drug of choice for premedication is midazolam (dormicum) [11-13]. Midazolam (dormicum, flormidal) is a short-acting benzodiazepine with high lipophilicity at physiological pH, which leads to its rapid onset of action [10]. This drug is ideal for “one-day surgery”, where it is necessary to quickly achieve anxiolytic action, a sense of comfort. It is not completely perfect, but the speed and breadth of its action indicate that this drug is better than most others currently available. It can be taken orally, administered intranasally, intravenously, intramuscularly and administered rectally. Its advantages are as follows:
- Rapid onset of action (elimination of anxiety, the onset of sedation and anterograde amnesia);
- Complete absorption and high bioavailability (> 90%);
- A minimum of side effects from the cardiovascular system and respiration;
- Short duration of
When using midazolam, separation from parents is easier, anesthesia becomes less traumatic and emotional and behavioral disorders of the postoperative period are weakened, especially with ketamine anesthesia. Oral administration of the drug is less traumatic than the intranasal route of administration, especially in many infants and children. At the same time, the bitter taste of midazolam can be masked with cherry syrup. The dose of midazolam 0.4-0.5 mg/kg orally usually leads to effective sedation and eliminates agitation for 20-30 minutes, after which this effect is reduced. Studies have shown that ingestion of the drug has a negligible effect on the volume and acidity of the stomach [10].
Children who are unable to take midazolam orally can receive it intravenously or rectally. A dose of 0.1 mg/kg intravenously provides rapid sedation and eliminates agitation. With this type of drug administration, it is necessary to provide for the possibility of prescribing oxygen and artificial ventilation in case of development of excessive sedation and respiratory depression. With rectal administration, a dose of 3 mg/kg is diluted in 5 ml of saline, which provides sedation for 20-30 minutes [11].
According to some reports, midazolam reduces the likelihood of postoperative nausea and vomiting, as well as the frequency of negative changes in behavior in young children in the first week after surgery [11,13]. According to some authors, midazolam does not lengthen the recovery time after anesthesia [10,11,13].
Background
Optimization of an esthetic benefits in one-day surgery in children by including midazolam in the sedation.
Methods
Midazolam at a dose of 0.4 mg/kg per os or 0.3 mg/kg intramuscularly 20 minutes before anesthesia was used as a sedative drug for sedation. The necessity of prescribing a sedative drug in premedication was determined individually and was guided by the obtained data of the Kerdo vegetative index. The criteria for prescribing midazolam were as follows:
- a negative reaction when trying to separate from parents of children older than 6 months (since it is difficult to find contact with children of this age, ensure a quiet separation from parents and induction into anesthesia);
- children with negative experience with medical personnel;
- An increased level of anxiety in the preoperative
To assess the degree of sedation in the preoperative period when using midosolam in premedication, the Ramsay sedation rating scale was used. Assessment of the degree of sedation was carried out 5, 10 and 20 minutes after sedation (Table 1).
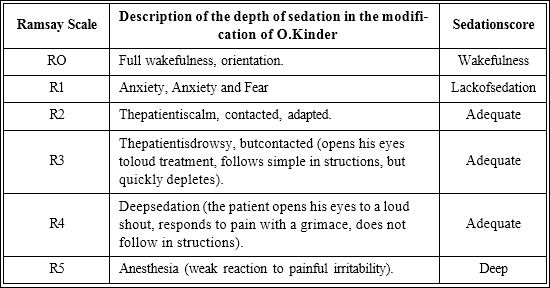
Table 1: Determining the degree of sedation on the Ramsay scale.
Sedative sedation at a dose of 0.4 mg/kg was orally performed in 83 children. 30 of them (36.1%) from 6 months to 3 years old, the remaining 53 (63.9%) were between the ages of 3 to 7 years.
Results
Analysis of the depth of sedation showed that 5 minutes after sedation in 7 children (8.4%), the degree of sedation was at the RO level, and in 67 children (80.7%) at the RI level, in 9 children (10.8%) at R2 level. After 10 minutes, 72.3% of the children began to experience drowsiness, but at the same time they were in contact, performed simple commands, opened their eyes to treatment, which corresponded to the R3 degree of sedation. The remaining 27.7% of the children did not experience drowsiness, while they were calm and contact (sedation degree R2).At the 20th minute of the study, 84.3% of the children reached R3 sedation. And 15.7% of children at the time of separation from their parents corresponded to degree R2. When using midazolam, there were no cases of deep sedation. All patients maintained a response to loud treatment. By the 20th minute, none of the studied patients receiving midazolam experienced anxiety anxiety and fear when parting with their parents. The degree of sedation R2 and R3 was regarded as adequate sedation. In 5 children (6%), hiccups that started 10-15 minutes after taking the drug, which stopped after induction in anesthesia, were noted as side effects. Other side effects associated with the use of midazolam were not observed. Thus, the effect of premedication reached its maximum effect by the 20th minute. At the same time, all patients receiving midazolam did not experience anxiety, were calm when they parted with their parents, which met the requirements of the anesthesiologist and relieved psychological stress and the patient. Consequently, the premedication provided by the administration of midazolam at a dose of 0.4 mg/kg orally made it possible to achieve a sedative effect, making children more contacted, while allowing them to remain conscious without inhibiting reflexes from the respiratory tract. Midazolam is one of the modern representatives of the benzodiazepine group, which has solubility in water. However, its hydrophilic properties change to lipotropic when it enters the body, which leads to rapid binding to GABAergic and benzodiazepine receptors. As a result, 10 minutes after ingestion, not only the psychomotor inhibition of the patient develops, but also a quick return to normal activity at the end of the use of the drug. It should be noted pronounced anxiolytic, anticonvulsant and sedative effects, low allergenicity, as well as anterograde amnesia inherent in midazolam.
Induction of sevoflurane in groups where premedication was carried out by midazolam proceeded smoothly. During induction of anesthesia, anxiety was not observed, as well as significant excitement characteristic of sevoflurane induction in children. Children calmly reacted to the supply of a high concentration of sevoflurane. No tachycardia was observed in children of the studied groups at the stages of their admission to the operating room and during the induction of anesthesia. When assessing mean arterial pressure, a significant difference was revealed at the stages of admission to the surgical induction into anesthesia. In the groups where midazolam was premedicated, the average blood pressure was significantly lower at these stages, which indicated a decrease in psycho emotional stress after sedation. In children who did not receive sedative sedation, an increase in during induction into anesthesia in children without the use of midazolam in premedication, an increase in respiratory rate was associated with their excitation during sevoflurane induction and was transient in nature. At the stages of admission to the operating room and induction into anesthesia in groups where sedation was administered with midazolam, the respiratory rate was lower than in groups without sedative premedication heart rate and an increase in blood pressure were noted.
In children who were not premedicated by midazolam separation from their parents, as well as the initial stages of induction, they were accompanied by a sharp psycho-emotional reaction in the form of crying. This caused hyper salivation, which led to the accumulation of saliva and mucus in the upper respiratory tract. Analysis of the time of awakening of children showed that the greatest duration of post-narcotic sleep was observed in groups where sedation premedication with midazolam was used. However, to assess the effect of sedative sedation on the duration of post-anesthesia sleep, it is important to compare the duration of sleep between groups with the same type of analgesia. So, when comparing the time of post-anesthetic sleep between patients who were anesthetized by regional methods, while some patients were premedicated, while others did not, no significant difference was obtained. It is also worth noting that in the groups receiving midazolam in premedication, there was a more comfortable waking up of children and the absence of post-narcotic arousal, which was usually found in children less than 5 years of age. While in children not receiving premedication, post-narcotic excitement was noted. This complication is extremely unpleasant, negatively perceived by parents and can cause physical damage in the area of the surgical wound. Smoother awakening in groups of children with midazolam premedication is associated, firstly, with the fact that a longer post-narcotic sleep contributed to a decrease in the concentration of anesthetic in the blood at the time of their awakening. Secondly, the ability of midazolam to cause anterograde amnesia could also relieve children of stress upon awakening, providing calm and elimination of unpleasant memories.
Thus, in the light of the above information, each anesthetist should carefully plan all aspects of the preoperative introduction of each individual child, including premedication means in this plan, if there is a clear need for them. The point of view of some doctors “applying” standard premedication is extremely erroneous, since there are no two identical patients. It is necessary to choose the method of sedation that is optimal and ideal for the child.
Discussion
The ideal premedication for children should meet several requirements: the preparations for it should be available, easy to use, allowed in pediatric practice, safe, not have unwanted side effects, and not require intensive monitoring. Midazolam is the optimal drug for sedation in one-day surgery in children.
References
- Nivoche Y, Lucas M, Dahmani S, Brasher C, Wodey E, et (2011) French current practice for ambulatory anesthesia in children: A survey among the French-speaking Pediatric Anesthesiologists Association (ADARPEF). Paediatr Anaesth 21: 379-384.
- Dosani FZ, Flaitz CM, Whitmire HC, Vance BJ, Hill JR (2014) Postdischarge events occurring after pediatric sedation for Pediatr Dent 36: 411-416.
- Musani IE, Chandan NV (2015) A comparison of the sedative effect of oral versus nasal midazolam combined with nitrous oxide in uncooperative children. Eur Arch Paediatr Dent 16: 417-424.
- Narendra PL, Naphade RW, Nallamilli S, Mohd S (2015) A comparison of intranasal ketamine and intranasal midazolam for pediatric Anesth Essays Res 9: 213-218.
- Olkkola KT, Ahonen J (2008) Midazolam and other benzodiaze- Handb Exp Pharmacol 182: 335-360.
- Ozcan A, Kaya AG, Ozcan N, Karaaslan GM, Er E, et al. (2014) Effects of ketamine and midazolam on emergence agitation after sevoflurane anaesthesia in children receiving caudal block: A randomized trial. Bras Anestesiol 64: 377-381.
- Pambianco DJ, Borkett KM, Riff DS, Winkle PJ, Schwartz HI, et (2016) A phase IIb study comparing the safety and efficacy of remimazolam and midazolam in patients undergoing colonoscopy. Gastrointest Endosc 83: 984-992.
- Polaner DM, Drescher J (2011) Pediatric regional anesthesia: What is the current safety record? Paediatr Anaesth 21: 737-742.
- Tavassoli-Hojjati S, Mehran M, Haghgoo R, Tohid-Rahbari M, Ahmadi R (2014) Comparison of oral and buccal midazolam for pediatric dental sedation: A randomized, cross-over, clinical trial for efficacy, acceptance and safety. Iran J Pediatr 24: 198-206.
- Welte JF, Desgranges FP, De Queiroz SM, Chassard D, Bouvet L (2017) Medication errors in paediatric anaesthesia: The hidden part of the iceberg. Br J Anaesth 118:. 797-798.
- Verma RK, Paswan A, De A, Gupta S (2012) Premedication with midazolam nasal spray: An alternative to oralmidazolam in Anesth Pain Med 1: 248-251.
- Wiltshire HR, Kilpatrick G, Tilbrook GS, Borkett K (2012) A Placeboand Midazolam-Controlled Phase I Single Ascending-Dose Study Evaluating the Safety, Pharmacokinetics, and Pharmacodynamics of Remimazolam (CNS 7056). Anesth Analg 115: 284-296.
- Trevor S, Upadya M, Sinha C, Kaur M (2012) A comparison of midazolam and clonidine as an oral premedication in pediatric Saudi J Anaesth 6: 8-11.
Citation: : Nasibova EM (2020) The Benefits of Premedication for Small Surgical Interventions in One-Day Surgery in Children. J Anes Perio Manag 4: 007.
Copyright: © 2020 Nasibova EM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.