*Corresponding Author:
Hafiz Hafeez Ullah,
Doctor of Pharmacy the Indus Hospital Lahore, Kahna Nau, Pakistan
Tel: +923364794595
Email: hafizhafeez54@gmail.com
Abstract
The current study was being performed to evaluate the birth complications in diabetic mothers; including both maternal and fetal complications; miscarriages. The nature of study was observational cross-sectional study. The study was being taken place at different hospitals, clinical settings, and maternity homes of Lahore during September 2016 November 2016. The demographic data, family history, socio-economic history, indications, examination findings, results, lab findings etc. were recorded. Total 200 pregnant diabetic patients were evaluated for this study. The age limit for this study was 18-40 years. The patients were being analyzed for their FBS/ BSR or HbA1c findings and the type of diabetes was being recorded. Out of 200 patients, 81% had GDM while the remaining patients were being presented with pregestational diabetes (type I 5%, type II 14% patients). Most of the GDM cases were being diagnosed during 5th to 8th week of pregnancy. Out of 200 pregnancies, 20.5% (41) of these patients had normal pregnancies, and had no major fetal complications except uncontrolled sugar level in mothers. Remaining 79.5% (159) pregnancies/deliveries were associated with some major complications including respiratory distress, macrosomia, hypoglycemic babies, CVS malformations and still births/miscarriages. The ratio of normal vaginal delivery to CS was found out to be 29% to & 76%. The major indications for these CS deliveries were placental abruption (19.74%), dystocia (14.47%), uterine rupture (13.16%), breech position (6.58%), fetal distress (46.05%) and to some extent previous CS. The miscarriages were being associated with hypertension (41.5%), polyhydramnios (22%), Hughes syndrome (12.2%), and uncontrolled sugar level (24.3%). In our study population TT immunization status was good i.e. 76%. Diabetes is still a major problem of birth complications and miscarriages. Public awareness program is required to educate the people about reproductive health and to motivate them to undergo BSR/FBS during pregnancy prior to 24thgestational weeks to diagnose for GDM.
Keywords
Complications; Diabetes; Foetus; GDM; Miscarriage; Neonate; Pregnancy
Introduction
Definition
“Diabetes Mellitus (DM), commonly referred to as diabetes, is a group of metabolic diseases in which there are high blood sugar levels over a prolonged period”.
Overview
DM is a chronic disorder characterized by hyperglycemia and the late development of vascular and neuropathic complications. Regardless of its cause, the disease is associated with a common hormonal defect namely insulin deficiency that may be absolute or relative in the context of coexisting insulin resistance. The effect of insufficient insulin plays a primary role in the metabolic derangements linked to diabetes; hyperglycemia, in turn, plays an important role in disease-related complications [1].
Nomenclature and classification of diabetes
The first widely accepted classification of diabetes mellitus was published by WHO in 1980 and, in modified form, in 1985. The 1980 Expert Committee proposed two major classes of diabetes mellitus and named them, IDDM or Type 1, and NIDDM or Type 2. In the 1985 Study Group Report the terms Type 1 and Type 2 were omitted, but the classes IDDM and NIDDM were retained, and a class of Malnutrition–Related Diabetes Mellitus (MRDM) was introduced. In both the 1980 and 1985 reports other classes of diabetes included Other Types and Impaired Glucose Tolerance (IGT) as well as GDM. These were reflected in the subsequent International Nomenclature of Diseases (IND) in 1991, and the tenth revision of the International Classification of Diseases (ICD–10) in 1992. The 1985 classification was widely accepted and is used internationally [2].
The nomenclature of human DM has been revised, and this classification has been accepted throughout the medical world and literature. The major categories of diabetes are [3].
- Insulin-dependent DM, type I or IDDM
- Noninsulin-dependent DM, type II or NIDDM
- Secondary DM or type S
- Impaired glucose tolerance, IGT
- Gestational diabetes or GDM
- Previous abnormality of glucose tolerance PrevAGT
Types
The vast majority of cases of diabetes fall into two broad etiopathogenetic categories. In one category, type-1 diabetes, the cause is an absolute deficiency of insulin secretion. Individuals at increased risk of developing this type of diabetes can often be identified by serological evidence of an autoimmune pathologic process occurring in the pancreatic islets and by genetic markers. In the other, much more prevalent category, type-2 diabetes, the cause is a combination of resistance to insulin action and an inadequate compensatory insulin secretory response [4].
In a recent study the basic classification of diabetes was described as follows (Tables 1.1 & 1.2): [1].
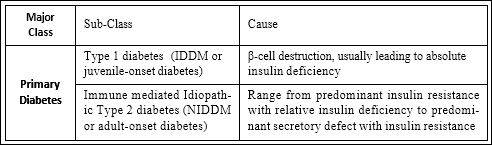
Table 1.1: Primary Diabetes and its Classification.
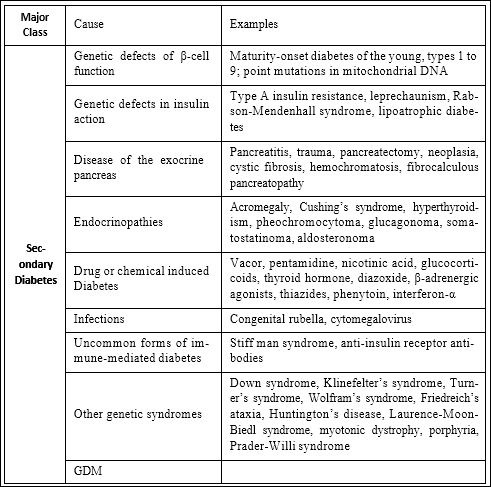
Table 1.2: Secondary Diabetes and its Classification.
Etiology
The vast majority of human diabetics show no clear etiological analogy. But certain rare cases are clearly due to primary pancreatic disease which destroys insulin production, and to other endocrine factors which induce a diabetic state. These include:
Primary pancreatic destruction
- Total surgical pancreatectomy for widespread carcinoma or hyperinsulinism
- calculus disease and chronic relapsing diabetes
- haemochromatosis (these three forms are severely insulin-deficient)
Primary disturbance of other endocrines (Table 2):
Table 2: Endocrinal disturbances during Diabetes [5].
Risk Factors
Type-1 Diabetes
The major genetic susceptibility to IDDM is determined by genes in the HLA chromosomal region. An increased relative risk for developing the disease is observed in subjects who are HLA A1, A2, B8, B18, B15, B40, CW3, Bfs, DW3, DW4, DRW3, and DRW4 positive.
There is an additive relative risk in subjects who possess two “high risk” HLA B alleles which has an important influence on the prevalence of the disease in sibships and possibly on the concordance rate in diabetic identical twins [6].
Type2 diabetes
Type II diabetes is a common disorder whose prevalence is increasing in the United States and throughout the world. Type II diabetes is also associated with several other metabolic abnormalities such as central obesity, hypertension, and dyslipidemia, which contributes to the very high rate of cardiovascular morbidity and mortality. The main pathologic defects in diabetes consist of excessive hepatic glucose production, peripheral insulin resistance, and defective beta-cell secretory function.
Treatment of type-1 and type-2 DM
Initiation of non-pharmacologic therapy should be started as soon as the diagnosis is made. Pharmacologic agents should be initiated if the glycemic goals are not met with a 3-month trial of diet and exercise. The cornerstone of therapy consists of a regular exercise routine along with a diet consisting of 40% to 50% complex carbohydrates, 10% to 20% protein, and monounsaturated fats such as canola oil and olive oil.
If non-pharmacologic therapy does not achieve adequate glycemic control, initiation of an oral anti-diabetic agent is warranted. In addition to the sulfonylureas, which work by stimulating insulin secretion, we now have metformin, which inhibits excessive hepatic glucose production; acarbose, which delays the absorption of carbohydrates in the gut; and troglitazone, which reduces insulin, resistance primarily in skeletal muscle [7].
Embryonic stem (ES) cells display the ability to differentiate in vitro into a variety of cell lineages. Using a cell-trapping system, we have obtained an insulin-secreting cell clone from undifferentiated ES cells. Clusters obtained from this clone were implanted (1x10(6) cells) in the spleen of streptozotocin-induced diabetic animals. Transplanted animals correct hyperglycemia within 1 week and restore body weight in 4 weeks. Whereas an intraperitoneal glucose tolerance test showed a slower recovery in transplanted versus control mice, blood glucose normalization was same after a challenge meal. This approach opens new possibilities for tissue transplantation in the treatment of type-1 and type-2 diabetes and offers an alternative to gene therapy [8].
Signs and symptoms of type-1 and type-2 DM
Some of the signs and symptoms commonly experienced include (Figure 1)
- Frequent urination
- Excessive thirst
- Increased hunger
- Weight loss, Tiredness
- Lack of interest and concentration
- A tingling sensation or numbness in the hands or feet
- Blurred vision
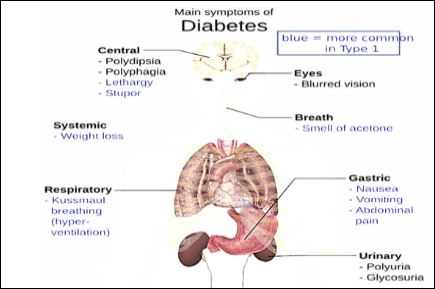
Figure 1: Main Symptoms of Diabetes.
Gestational Diabetes Mellitus (GDM)
GDM represents a heterogeneous group of metabolic disorders, which result in varying degrees of maternal hyperglycemia and pregnancy-associated risk. The frequency of GDM is rising globally and may also increase further as less-stringent criteria for diagnosis are adopted [9].
Definition
GDM is defined as “Glucose intolerance that is first detected during pregnancy”. This simple definition belies the complexity of a condition that spans a spectrum of glycaemia, pathophysiology, and clinical effects and for which there is a wide diversity of opinion regarding detection and clinical management [10] (Figure 2).
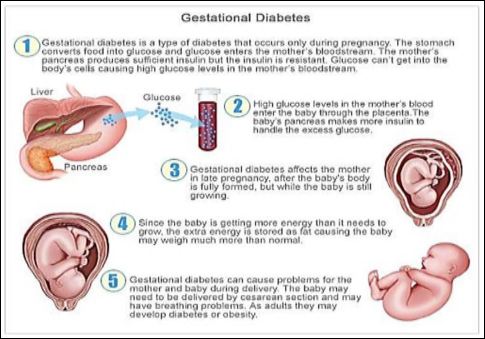
Figure 2: Main Symptoms of Diabetes.
Etiology
During pregnancy, the placenta makes hormones that can lead to a buildup of sugar in blood. Usually, pancreas can make enough insulin to handle that. If not, blood sugar levels will rise and can cause GDM. A transient physiologic insulin resistance and hyperinsulinemia are characteristic of normal pregnancy. In women with β-cells that are not capable of maintaining the high insulin production, GDM develops. A restriction of high-insulinogenic carbohydrates may help to prevent the development of GDM [11]. In pregnancy, several physiologic changes take place, the sum of which tends to reset the glucose homeostasis in the direction of diabetes. About 1-2% of all pregnant women develop an abnormal glucose tolerance in pregnancy, but most often glucose tolerance returns to normal postpartum. This condition is called GDM [12] ) (Figure 2.1).
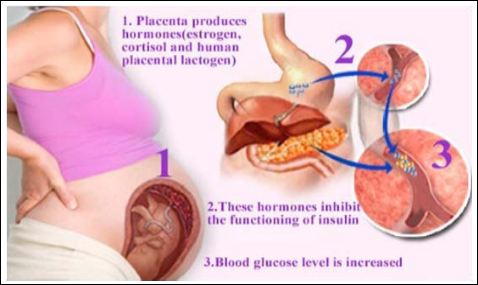
Figure 2.1: Etiology of GDM.
GDM typically does not cause any noticeable signs or symptoms. This is why screening tests are so important. Rarely, an increased thirst or increased urinary frequency may be noticed. GDM has serious, long-term consequences for both baby and mother, including a predisposition to obesity, metabolic syndrome and diabetes later in life. Early detection and intervention can greatly improve outcomes for women with this condition and their babies. Unfortunately, screening and diagnostic tests are not uniform worldwide, which could lead not only to under diagnosis but also under management of the illness [13] (Table 3) (Figure 3).
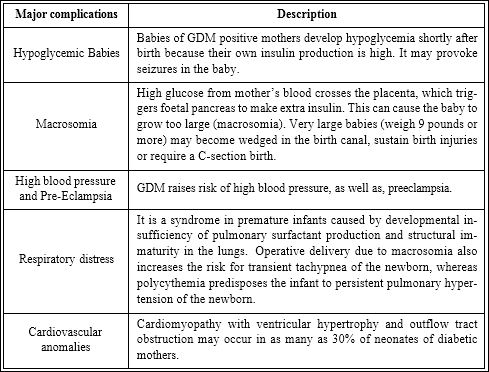
Table 3: Major complications associated with GDM.
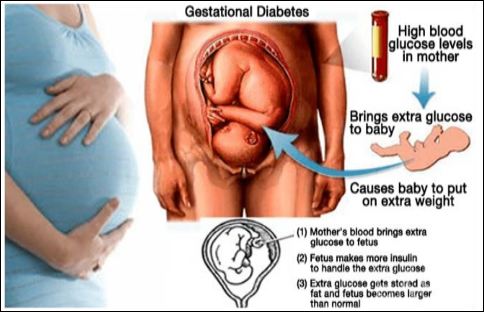
Figure 3: Cause of Macrosomia.
Objectives
- To determine birth complications in diabetic mothers
- To determine the prevalence of GDM during pregnancy
- To determine the ratio of CS and risk factors leading to CS
- To determine reproductive health of females in our community
Literature Review
The current study suggested that although the excess risk for birth defects among children of mothers with diabetes mellitus is well doc- umented, there are few data concerning the risk for specific malforma- tions. In the Atlanta Birth Defects Case-Control Study, those risks for malformations were evaluated. The population-based study included 4929 live and stillborn babies with major malformations ascertained by the Metropolitan Atlanta Congenital Defects Program in the first year of life born to residents of Metropolitan Atlanta between 1968 and 1980. The study also included 3029 non-malformed live babies who were frequency-matched to case babies by race, period of birth, and hospital of birth. The relative risk for major malformations among infants of mothers with insulin-dependent diabetes mellitus (n=28) was 7. (5% Confidence Interval [CI] 1.9, 33.5) compared with infants of non-diabetic mothers. The relative risks for major central nervous system and cardiovascular system defects were 15.5 (95% CI=3.3, 73.8) and 18.0 (95% CI=3.9, 82.5), respectively. The absolute risks for major, central nervous system, and cardiovascular system malforma- tions among infants of diabetic mothers were 18.4, 5.3, and 8.5 per 100 live births, respectively. Infants of mothers with gestational diabetes mellitus who required insulin during the third trimester of pregnancy were 20.6 (95% CI=2.5, 168.5) times more likely to have major car- diovascular system defects than infants of non-diabetic mothers. The absolute risk for infants of this group of diabetic mothers was 9.7%. No statistically significant differences were found among infants of mothers with gestational diabetes mellitus who did not require insulin during pregnancy. These results suggested a stronger association than previously reported between maternal diabetes mellitus and specific categories of major malformations and implicate gestational diabetes mellitus as a risk factor for major cardiovascular system defects [14].
In this study Neonatal morbidity was assessed in the offspring of 878 mothers with Gestational Diabetes Mellitus (GDM), 132 mothers with pre-GDM, and 380 control subjects. Compared with the con- trol group, the GDM group had a higher incidence of complications, including macrosomia, hypoglycemia, hyperbilirubinemia, hypo- calcemia, polycythemia, and major congenital anomalies (P<0.05).
Although our GDM patients were stringently managed with diet or diet plus insulin, as indicated and maintained almost euglycemic val- ues, these neonatal complications could not be eliminated. Our data may be consistent with observations published during the last decade that even subtle degrees of maternal hyperglycemia can have a det- rimental effect on perinatal outcome. Most neonatal complications readily respond to therapy if diagnosed and treated early and prompt- ly. Macrosomia can have a detrimental effect on delivery (trauma) and later long-term implications during childhood. Tight metabolic control with diet and, when indicated, insulin treatment may be ad- vantageous in reducing fetal birth weight. Criteria of how tight the metabolic control should be remain to be accurately defined [15].
This study proposed that the perinatal mortality rate of Infants of Diabetic Mothers (IDMs) has declined dramatically from 250 per 1000 live births in the 1960s to a near-normal 20 per 1000 live births in the 1980s. Five to 8% of all IDMs suffer from major congenital mal- formations, and it is the latter that are responsible for 50% of these perinatal deaths. It has been shown that tight glycemic control prior to conception and during pregnancy can prevent an excess rate of con- genital malformations, fetal macrosomia, birth trauma, and neona- tal respiratory distress syndrome. We briefly reviewed the short- and long-range complications that occur in Offspring of Diabetic Mothers (ODMs) from gestation through young adulthood. Short-term neo- natal complications, such as hypoglycemia, hypocalcemia, hypomag- nesemia, hyperbilirubinemia, and polycythemia, are related mainly to fetal hyperinsulinemia, hypoxemia, and prematurity. They are readily controllable within the setup of modern neonatal intensive care units. Long-range complications include an increased rate of childhood and adolescent obesity, impaired glucose tolerance or diabetes mellitus, and subtle neuropsychological dysfunctions. These may be related to the severity of the maternal hyperglycemia during pregnancy, the consequent fetal hyperinsulinemia, and third trimester maternal lipid metabolism disturbances. Today we have at hand the knowledge and tools to properly treat both pregestational and gestational diabetes. Increased education of the general practitioner and the target popu- lation regarding early referral of pregestational diabetic mothers and the implementation of screening programs for gestational diabetes will further reduce diabetic pregnancy-related morbidity [16].
This study proposed that intrauterine exposure to diabetes is asso- ciated with an excess of diabetes and obesity in the offspring, but the effects of intrauterine exposure are confounded by genetic factors. To determine the role of the intrauterine diabetic environment per se, the prevalence of diabetes and the mean BMI were compared in siblings born before and after their mother was recognized as having diabetes. Nuclear families in which at least one sibling was born before and one after the mother was diagnosed with type 2 diabetes were selected. Consequently, the siblings born before and after differed in their ex- posure to diabetes in utero. A total of 58 siblings from 19 families in which at least one sibling had diabetes were examined at similar ages (within 3 years). The risk of diabetes was significantly higher in sib- lings born after the mother developed diabetes than in those born be- fore the mother’s diagnosis of diabetes (odds ratio 3.7, P=0.02). In 52 families, among 183 siblings without diabetes, the mean BMI was 2.6 kg/m2 higher in offspring of diabetic than in offspring of non-diabetic pregnancies (P=0.003). In contrast, there were no significant differ- ences in risk of diabetes or BMI between offspring born before and after the father was diagnosed with diabetes. Intrauterine exposure to diabetes per se conveyed a high risk for the development of diabetes and obesity in offspring in excess of risk attributable to genetic factors alone [17].
The aim of the study was to examine the outcome of the pregnan- cy and neonatal period in women with gestational diabetes mellitus and non-diabetic pregnant women, and in women with early and late diagnosis of gestational diabetes mellitus. It included 327 wom- en with gestational diabetes mellitus and 295 non-diabetic women, who were screened with a 75 g oral glucose tolerance test because of risk factors for gestational diabetes. Women with gestational dia- betes mellitus were treated with a low-caloric diet and insulin when appropriate, while women in the control group received routine an- tenatal care. Gestational age at delivery was significantly lower in the group with gestational diabetes mellitus, both when considering all deliveries (39.1 ± 1.7 weeks versus 39.8 ± 2.0 weeks, p<0.05) and only those with spontaneous onset of labor (38.8 ± 2.0 weeks versus 40.0 ± 1.6 weeks, p<0.05). The frequency of macrosomia was in- creased, although not statistically significant (8% vs. 2%, p=0.07), and the rate of admission to the neonatal ward was significantly increased (18% vs. 9%, p<0.05) in the group with gestational diabe- tes. Women with early diagnosis of gestational diabetes mellitus had a significantly increased need for insulin treatment during pregnancy (36% vs. 9% p<0.05) and a significantly higher occurrence of diabetes mellitus at follow-up from two months until three years postpartum. This study of women with gestational diabetes mellitus and non-dia- betic pregnant women showed that gestational diabetes mellitus was associated with a significantly lower gestational age at delivery and an increased rate of admission to the neonatal ward. Women diagnosed with GDM before 20 weeks of gestation had an increased need for in- sulin treatment during pregnancy and a high risk of subsequent overt DM, compared with women diagnosed with GDM later in pregnancy [18].
This study suggested that Dietary vitamin D supplementation is as- sociated with reduced risk of type 1 diabetes in animals. Our aim was to ascertain whether or not vitamin D supplementation or deficiency in infancy could affect development of type 1 diabetes. A birth-cohort study was done, in which all pregnant women (n=12 055) in Oulu and Lapland, northern Finland, who were due to give birth in 1966 were enrolled. Data was collected in the first year of life about frequency and dose of vitamin D supplementation and presence of suspected rickets. Our primary outcome measure was diagnosis of type 1 diabetes by the end of December, 1997. 12,058 out of 12,231 represented live births, and 10,821 (91% of those alive) children were followed-up at age 1 year. Of the 10,366 children included in analyses, 81 were diagnosed with diabetes during the study. Vitamin D supplementation was asso- ciated with a decreased frequency of type 1 diabetes when adjusted for neonatal, anthropometric, and social characteristics (Rate Ratio [RR] for regular VS no supplementation 0·12, 95% CI=0·03–0·51, and irreg- ular VS no supplementation 0·16, 0·04-0·74. Children who regularly took the recommended dose of vitamin D (2000 IU daily) had a RR of 0·22 (0·05-0·89) compared with those who regularly received less than the recommended amount. Children suspected of having rickets during the first year of life had a RR of 3·0 (1·0-9·0) compared with those without such a suspicion. Dietary vitamin D supplementation is associated with reduced risk of type 1 diabetes. Ensuring adequate vitamin D supplementation for infants could help to reverse the in- creasing trend in the incidence of type 1 diabetes [19].
The objective of the current study was to investigate maternal, perinatal, and neonatal outcomes of pregnancies in women with type 1 diabetes in the Netherlands. The study design was nationwide prospective cohort study. It was performed in 118 hospitals in the Netherlands. Participants include 323 women with type 1 diabetes who became pregnant between 1 April 1999 and 1 April 2000. Main outcome measures were Maternal, perinatal, and neonatal outcomes of pregnancy. Results showed that 84% (n=271) of the pregnancies were planned. Glycaemic control early in pregnancy was good in most women (HbA1c 7.0% in 75% (n=212) of the population), and folic acid supplementation was adequate in 70% (n=226). 314 pregnancies that went beyond 24 weeks’ gestation resulted in 324 infants. The rates of pre-eclampsia (40; 12.7%), preterm delivery (101; 32.2%), caesare- an section (139; 44.3%), maternal mortality (2; 0.6%), congenital mal- formations (29; 8.8%), perinatal mortality (9; 2.8%), and macrosomia (146; 45.1%) were considerably higher than in the general population. Neonatal morbidity (one or more complications) was extremely high (260; 80.2%). The incidence of major congenital malformations was significantly lower in planned pregnancies than in unplanned preg- nancies (4.2% (n=11) v 12.2% (n=6); relative risk 0.34, 95% confi- dence interval 0.13 to 0.88). This study concluded that despite a high frequency of planned pregnancies, resulting in overall good glycae- mic control (early) in pregnancy and a high rate of adequate use of folic acid, maternal and perinatal complications were still increased in women with type 1 diabetes. Neonatal morbidity, especially hypo- glycaemia, was also extremely high. Near optimal maternal glycaemic control (HbA1c 7.0%) apparently is not good enough [20].
The aim of this study was to investigate that a transient physiologic insulin resistance and hyperinsulinemia are characteristic of normal pregnancy. This insulin action has evolved during a period of human evolution that was characterized by a very low-carbohydrate nutri- tion. The development of gestational diabetes mellitus (GDM) is pro- posed to result from a collision of this evolutionary inheritance with our “modern” nutrition: The “Western” high-insulinogenic nutrition increases the postprandial demand for insulin significantly during the insulin resistant state of late pregnancy. In women with β-cells that are not capable of maintaining the high insulin production, GDM de- velops. A restriction of high-insulinogenic carbohydrates may help to prevent the development of GDM [11].
This study proposed that Pregnancies of women with type 1 dia- betes mellitus are associated with maternal and perinatal complica- tions. These complication rates remain elevated despite achievement of the treatment goals described in the widely used guidelines of the American Diabetes Association (i.e. HbA1c level ≤ 7.0%). Against this background, we sought to answer two questions: (1) are HbA1c levels within 1% above normal appropriate in pregnant women with type 1 diabetes or should treatment be aimed at normal HbA1c levels; and (2) how many Self-Monitored Blood Glucose (SMBG) levels are needed per day to obtain an adequate image of glycaemic control in pregnant women with type 1 diabetes? We asked 43 pregnant women with type 1 diabetes to use the Continuous Glucose Monitoring System (CGMS) once in each trimester of pregnancy, while continuing their SMBG measurements. Glucose levels measured with the CGMS were com- pared between patients with HbA1c levels of 4.0-6.0%, 6.0-7.0% and >7.0%. Self-monitored glucose levels and those measured with CGMS were compared between patients with four or five, six to nine and ten or more SMBG determinations daily. In patients with HbA1c levels ≤6.0%, the glucose levels obtained by CGMS were significantly better than in patients with HbA1c levels>6.0%. In women with HbA1c lev- els 6.0-7.0% and>7.0%, these levels did not differ. The detection rate of hyper- and hypoglycemic episodes was significantly higher in patients with ten or more SMBG determinations daily than in patients with fewer than ten. Treatment of diabetes in pregnant women should be aimed at achieving HbA1c levels within the normal range, i.e. ≤ 6.0%.
A minimum of ten SMBG determinations daily is necessary to obtain adequate information of all daily glucose fluctuations [21].
The current study was conducted to determine the range of com- plications occurring in Infants of Diabetic Mothers (IDMs). An obser- vational cross-sectional study was performed in Federal Government Services Hospital, Islamabad and National Institute of Child Health, Karachi, from August 1999 to January 2000. All IDMs born during the study period were immediately admitted to the neonatal intensive care unit after delivery. Maternal history was obtained and a detailed phys- ical examination was performed to detect congenital abnormalities. Babies were screened for hypoglycemia, hypocalcaemia, hyperbiliru- binemia, birth asphyxia, Respiratory Distress Syndrome (RDS) and birth trauma. Outcome of IDMs and relative frequencies of various complications were evaluated. Results were analyzed using Statistical Package for Social Sciences (SPSS) version 11. A total number of 40 babies with IDM were included in the study. Out of diabetic mothers, only 19 (47.5%) were taking insulin albeit irregularly. No mother was taking oral hypoglycemic agents, 5 (12.5%) were following only dietary advice while 16 (40%) were not following any advice for control of di- abetes. Twenty-two (55%) mothers were delivered by C-section and 18 (45%) had vaginal delivery. Seven (17.5%) mothers experienced birth injuries all of them were delivered vaginally and majority of them were large babies. Fifteen percent IDMs suffered from birth asphyxia. Most (82.5%) were delivered vaginally. Congenital anomalies were found in 10 (25%) babies. Eighteen (45%) were macrosomic, 20 (50%) were Appropriate for Gestational Age (AGA) and 02 (5%) were Small for Gestational Age (SGA) or growth retarded. Hypoglycemia was noted in 35% and hypocalcaemia in 15%. Hyperbilirubinemia was observed in 12 (30%) newborns. Mortality was 7.5%. The results of this study showed high frequency complications in IDMs. The diabetic mothers should have regular antenatal follow-up and maintain good glycemic control throughout pregnancy. Cesarean sections may be allowed more liberally, especially with clinical evidence of macrosomic babies, to avoid birth injury and asphyxia. All deliveries of diabetic mother should be attended by a pediatrician to minimize complications [22].
The current study proposed that Carbohydrate intolerance is the most common metabolic complication of pregnancy. Gestational Di- abetes Mellitus (GDM) poses numerous problems for both mother and fetus. The objectives of this study were to find out the incidence of gestational diabetes mellitus in pregnant women and their preg- nancy outcomes. It was also to discover the risk factors for the ad- mission of neonates to the Neonatal Intensive Care Unit (NICU). A hospital-based prospective study performed at King Khalid University Hospital (KKUH), where 685 pregnant women who were diagnosed with gestational diabetes mellitus, out of 8000 pregnant women regis- tered during January 2000 - December 2001, were followed and their outcomes studied. The incidence of gestational diabetes mellitus was found to be 8.6% (95% CI=8.1, 9.3). There were 511 (74.6%) spon- taneous vertex deliveries, and 148 (21.6%) were delivered by lower segment cesarean section. Maternal morbidity in these women was 1.2%. A total of 697 babies were delivered by these 685 women, out of whom 675 were singleton pregnancies, 9 sets of twins and one set of quadruplets. Six-hundred-eighty-seven babies were born alive, 7 ba- bies died in utero and 3 died in the neonatal period. The incidence of neonatal intensive care admission was 4.9%. The mean length of stay in the NICU was 16 days. The commonest cause of neonatal NICU admission was hyperbilirubinemia (41.2%). The risk factors for NICU admission were delivery by non SVD procedure (RR: 4.6, 95% CI= 2.8, 7.7), preterm deliveries, (RR: 4.6, 95% CI=2.7, 7.7), and induc- tion of labor (RR: 2.5, 95% CI=1.4, 4.5). The observation and quanti- fication of maternal outcomes with gestational diabetes mellitus were necessary, so that proper measures could be taken to reduce complica- tions during delivery and the neonatal period and thereby, minimize particularly NICU admission rate [23].
The current study proposed that Metformin is a logical treatment for women with gestational diabetes mellitus, but randomized trials to assess the efficacy and safety of its use for this condition are lacking. This study randomly assigned 751 women with gestational diabetes mellitus at 20 to 33 weeks of gestation to open treatment with met- formin (with supplemental insulin if required) or insulin. The prima- ry outcome was a composite of neonatal hypoglycemia, respiratory distress, need for phototherapy, birth trauma, 5-minute Apgar score less than 7, or prematurity. The trial was designed to rule out a 33% increase (from 30% to 40%) in this composite outcome in infants of women treated with metformin as compared with those treated with insulin. Secondary outcomes included neonatal anthropometric mea- surements, maternal glycemic control, maternal hypertensive compli- cations, postpartum glucose tolerance, and acceptability of treatment. Of the 363 women assigned to metformin, 92.6% continued to receive metformin until delivery and 46.3% received supplemental insulin. The rate of the primary composite outcome was 32.0% in the group assigned to metformin and 32.2% in the insulin group (relative risk, 1.00; 95% confidence interval, 0.90 to 1.10). More women in the met- formin group than in the insulin group stated that they would choose to receive their assigned treatment again (76.6% vs. 27.2%, P<0.001). The rates of other secondary outcomes did not differ significantly be- tween the groups. There were no serious adverse events associated with the use of metformin. In women with gestational diabetes melli- tus, metformin (alone or with supplemental insulin) is not associated with increased perinatal complications as compared with insulin. The women preferred metformin to insulin treatment [24].
The main objective of this study was to determine the role of in- trauterine hyperglycemia and future risk of type 2 diabetes in human offspring is debated. It studied glucose tolerance in adult offspring of women with either Gestational Diabetes Mellitus (GDM) or type-1 di- abetes, taking the impact of both intrauterine hyperglycemia and ge- netic predisposition to type-2 diabetes into account. The glucose toler- ance status following a 2-h 75-g Oral Glucose Tolerance Test (OGTT) was evaluated in 597 subjects, primarily Caucasians, aged 18-27 years. They were subdivided into four groups according to maternal glucose metabolism during pregnancy and genetic predisposition to type 2 di- abetes: 1) offspring of women with diet-treated GDM (O-GDM), 2) offspring of genetically predisposed women with a normal OGTT (O-No GDM), 3) offspring of women with type 1 diabetes (O-type 1), and 4) offspring of women from the background population (O- BP).The prevalence of type 2 diabetes and pre-diabetes (impaired glucose tolerance or impaired fasting glucose) in the four groups was 21, 12, 11, and 4%, respectively. In multiple logistic regression analy- sis, the adjusted Odds Ratios (ORs) for type 2 diabetes/pre-diabetes were 7.76 (95% CI=2.58-23.39) in O-GDM and 4.02 (1.31-12.33) in O-type 1 compared with O-BP. In O-type 1, the risk of type 2 dia- betes/pre-diabetes was significantly associated with elevated maternal blood glucose in late pregnancy: OR 1.41 (1.04-1.91) per mmol/l. A hyperglycemic intrauterine environment appears to be involved in the pathogenesis of type-2 diabetes/pre-diabetes in adult offspring of primarily Caucasian women with either diet-treated GDM or type-1 diabetes during pregnancy [25].
The purpose of this study was to assess changes in the prevalence of preexisting diabetes (diabetes antedating pregnancy) and gesta- tional diabetes mellitus (GDM) from 1999 through 2005. In this ret- rospective study of 175, 249 women aged 13-58 years with 209,287 singleton deliveries of ≥ 20 weeks’ gestation from 1999 through 2005 in all Kaiser Permanente hospitals in southern California, information from clinical databases and birth certificates was used to estimate the prevalence of preexisting diabetes and GDM. Preexisting diabetes was identified in 2,784 (1.3%) of all pregnancies, rising from an age- and race/ethnicity-adjusted prevalence of 0.81 per 100 in 1999 to 1.82 per 100 in 2005 (Ptrend=0.001). Significant increases were observed in all age-groups and all racial/ethnic groups. After women with preexisting diabetes were excluded, GDM was identified in 15,121 (7.6%) of 199,298 screened pregnancies. The age- and race/ethnicity-adjusted GDM prevalence remained constant at 7.5 per 100 in 1999 to 7.4 per 100 in 2005 (Ptrend=0.07). Among all deliveries to women with either form of diabetes, 10% were due to preexisting diabetes in 1999, rising to 21% in 2005, with GDM accounting for the remainder. The stable prevalence of GDM and increase in the prevalence of preexisting diabetes were independent of changes in the age and race/ethnicity of the population. The increase in preexisting diabetes, particularly among younger women early in their reproductive years, is of concern [26].
This current study proposed that Gestational diabetes mellitus is a substantial and growing health concern in many parts of the world. Certain populations are especially vulnerable to developing this con- dition because of genetic, social, and environmental factors. Gesta- tional diabetes has serious, long-term consequences for both baby and mother, including a predisposition to obesity, metabolic syndrome, and diabetes later in life. Early detection and intervention can greatly improve outcomes for women with this condition and their babies. Unfortunately, screening and diagnostic tests are not uniform world- wide, which could lead not only to under diagnosis but also under management of the illness. Here this study reported the controversies surrounding the causes, screening, diagnosis, management, and pre- vention of gestational diabetes, and gave specific recommendations for research studies to address the major issues of this medical condi- tion [13].
This study suggested that Gestational diabetes mellitus is a sub- stantial and growing health concern in many parts of the world. Cer- tain populations are especially vulnerable to developing this condition because of genetic, social, and environmental factors. Gestational dia- betes has serious, long-term consequences for both baby and mother, including a predisposition to obesity, metabolic syndrome, and diabe- tes later in life. Early detection and intervention can greatly improve outcomes for women with this condition and their babies. Unfor- tunately, screening and diagnostic tests are not uniform worldwide, which could lead not only to under diagnosis but also under man- agement of the illness. Here, we report the controversies surround- ing the causes, screening, diagnosis, management, and prevention of gestational diabetes, and give specific recommendations for research studies to address the major issues of this medical condition [13].
This study proposed that Pregestational (PGDM) and gestational (GDM) diabetes may be associated with a variety of fetal effects includ- ing increased rate of spontaneous abortions, intrauterine fetal death, congenital anomalies, neurodevelopmental problems and increased risk of perinatal complications. Additional problems of concern are fetal growth disturbances causing increased or decreased birth weight. Optimal control of maternal blood glucose is known to reduce these changes. Among the long lasting effects of these phenomena are a high rate of overweight and obesity at childhood and a high tendency to develop the “metabolic syndrome” characterized by hypertension, cardio-vascular complications and type-2 diabetes. Similarly, mater- nal overweight and obesity during pregnancy or excessive weight gain are also associated with increased obesity and complications in the offspring. Although there are different causes for fetal growth restric- tion (FGR) or for fetal excessive growth (Macrosomia), paradoxically both are associated with the “metabolic syndrome” and its long term consequences. The exact mechanism(s) underlying these long term effects on growth are not fully elucidated, but they involve insulin re- sistance, fetal hyperleptinemia, hypothalamic changes and most prob- ably epigenetic changes. Preventive measures to avoid the metabolic syndrome and its complications seem to be a tight dietary control and physical activity in the children born to obese or diabetic mothers or who had antenatal growth disturbances for other known or unknown reasons [27].
The current study proposed that Gestational Diabetes Mellitus (GDM) represents a heterogeneous group of metabolic disorders, which result in varying degrees of maternal hyperglycemia and preg- nancy-associated risk. The frequency of GDM is rising globally and may also increase further as less-stringent criteria for the diagnosis are potentially adopted. The additional burden placed on the health care system by increasing cases of GDM requires consideration of di- agnostic approaches and currently used treatment strategies. Debate continues to surround both the diagnosis and treatment of GDM despite several recent large-scale studies addressing these controver- sial issues. As many now have come to reassess their approach to the management of GDM, we provided information in this review to help guide this process. The goal for each health care practitioner should continue to be to provide optimum care for women discovered to have carbohydrate intolerance during pregnancy [9].
The aim of current study was to investigate the Gestational diabe- tes mellitus. It is defined as diabetes diagnosed during pregnancy that is not clearly overt diabetes, and is becoming more common as the epidemic of obesity and type-2 diabetes continues. Newly proposed diagnostic criteria will, if adopted universally, further increase the prevalence of this condition. Much controversy surrounds the diag- nosis and management of gestational diabetes. This review provided information regarding various approaches to the diagnosis of gesta- tional diabetes and the recommendations of a number of professional organizations. The implications of gestational diabetes for both the mother and the offspring were described. Approaches to self-moni- toring of blood glucose concentrations and treatment with diet, oral medications, and insulin injections were covered. Management of glucose metabolism during labor and the postpartum period were discussed, and an approach to determining the timing of delivery and the mode of delivery was outlined. This review provided an overview of current controversies as well as current recommendations for ges- tational diabetes care [28].
The current study was done to investigate life transitions associat- ed with high levels of stress affecting health behaviors among people with Type 1 diabetes. It suggested that Transition to motherhood is a major transition with potential complications accelerated by preg- nancy with risks of adverse childbirth outcomes and added anxiety and worries about pregnancy outcomes. Further, preparing and go- ing through pregnancy requires vigilant attention to a diabetes man- agement regimen and detailed planning of everyday activities with added stress on women. Psychological and social well-being during and after pregnancy are integral for good pregnancy outcomes for both mother and baby. The aim of this study was to establish the face and content validity of two novel measures assessing the well-being of women with type 1 diabetes in their transition to motherhood, 1) during pregnancy and 2) during the postnatal period. The approach to the development of the Pregnancy and Postnatal Well-being in T1DM Transition questionnaires was based on a four-stage pre-testing pro- cess; systematic overview of literature, items development, piloting testing of questionnaire and refinement of questionnaire. The ques- tionnaire was reviewed at every stage by expert clinicians, researchers and representatives from consumer groups. The cognitive debriefing approach confirmed relevance of issues and identified additional items. The literature review and interviews identified three main ar- eas impacting on the Women’s postnatal self-management; (1) psy- chological well-being; (2) social environment, (3) physical (maternal and fetal) well-being. The cognitive debriefing in pilot testing of the questionnaire identified that immediate postnatal period was difficult, particularly when the women were breastfeeding and felt depressed. The questionnaires fill an important gap by systematically assessing the psychosocial needs of women with type 1 diabetes during preg- nancy and in the immediate postnatal period. The questionnaires can be used in larger data collection to establish psychometric properties. The questionnaires potentially play a key role in prospective research to determine the self-management and psychological needs of wom- en with type 1 diabetes transitioning to motherhood and to evaluate health education interventions [29].
The current study suggested that Macrosomia is defined as birth- weight over 4,000 g irrespective of gestational age and affects 3-15% of all pregnancies. The present study aimed to determine the relation- ship between mother’s characteristics and macrosomic births and also compare macrosomic and normal newborns regarding the maternal and offspring complications of diabetes during pregnancy. In this case control study, among the 420 consecutive births occurring in public and private hospitals of Shiraz, Iran from October 2006 to March 2007, the data of 32 macrosomic and 128 normal newborns were an- alyzed using t-test and chi square in bivariate and logistic regression in multivariate model. The mean (SD) of neonate weight, height, and head size was 3323.4 (709), 48.95 (3.2), and 34.9 (1.8), respectively. Re- gression analysis showed that gestational diabetes (Odds Ratio (OR): 11.9, Confidence Interval CI=4.6-30.3), preeclampsia in the pregnan- cy period due to diabetes (OR: 3.81, CI=1.1-13.2), and macrosomic birth history (OR: 3.3, CI=1.04-10.4) were the main predictors of macrosomia. Moreover, macrosomia increased neonate hypoglycemia (OR: 4.7, CI=1.4-15.8) and section delivery (OR: 4.1, CI=1.27-13.1). Gestational diabetes, preeclampsia due to diabetes, and history of macrosomic birth were the main predictors of macrosomia. More- over, macrosomia increased some delivery complications for both mothers and newborns [30].
The current study suggested that women with Gestational Di- abetes Mellitus (GDM) and their offsprings are at increased risk of future type 2 diabetes and metabolic abnormalities. Early diagnosis and proper management of GDM, as well as, postpartum follow-up and preventive care is expected to reduce this risk. However, no large scale prospective studies have been done particularly from the devel- oping world on this aspect. The objective of this study was to identify and follow a cohort of pregnant women with and without GDM and their offspring to identify determinants and risk factors for GDM, for various pregnancy outcomes, as well as, for the development of fu- ture diabetes and metabolic abnormalities. This was a prospective co-
hort study involving pregnant women attending prenatal clinics from urban, semi-urban and rural areas in the greater Chennai region in South India. Around 9850 pregnant women was screened for GDM. Socio-economic status, demographic data, obstetric history, delivery and birth outcomes, perinatal and postnatal complications, neonatal morbidity, maternal postpartum and offsprings follow-up data will be collected. Those diagnosed with GDM were initially advised routine care. Those unable to reach glycaemic control with diet alone were advised to take insulin. Postpartum screening for glucose abnormal- ities were performed at months 3 and 6 and then every year for 10 years. The offsprings followed up every year for anthropometric mea- surements and growth velocity, as well as, plasma glucose, insulin and lipid profile. In addition, qualitative research carried out to identify barriers and facilitators for early GDM screening, treatment compli- ance and postpartum follow-up and testing, as well as, for continued adherence to lifestyle modifications. The study demonstrated whether measures to improve diagnosis and care of GDM mothers followed by preventive postpartum care are possible in the routine care setting. It also mapped out the barriers and facilitators for such initiatives and provided new evidence on the determinants and risk factors for both GDM development and occurrence of adverse pregnancy outcomes and development of future diabetes and metabolic abnormalities in the GDM mother and her offspring [31].
Materials and Methods
Study design
The design of the current study was observational cross-sectional study. A questionnaire with the variables related to birth complications in diabetic mothers was designed with consensus of gynecologists/patients for the study. The demographic data, family history, previous medical history, reproductive history as well as the Tetanus Toxoid Vaccination status and drug profile was included in the questionnaire. This study was conducted in different Hospitals, Clinical settings, Maternity homes in Lahore, Punjab Pakistan.
Data collection
The questionnaire was designed to collect information regarding various parameters associated with birth complications due to diabetes, directly by patient counseling. Records of patients having IDDM, NIDDM or GDM were evaluated for fetal status. The pathology reports like Hb A1C were reviewed to determine the glucose control during previous months. The type of diabetes in patients, presenting signs and symptoms, family history of diabetes, other related pathological conditions, diabetes associated risk factors in mother and child, birth complications, treatment strategies, risk of diabetes in newborn, were evaluated.
Inclusion criteria
In this study, we included all those female patients who gave informed consent to be a part of this study, with positive diagnostic tests for diabetes like BSR or FBS or whose HbA1c value indicated hyperglycemia during pregnancy in the time period of September 2016November 2016. In this study, those female patients were also added with the age limit between 18-40 years.
Exclusion criteria
In this study those female patients were not included who refused to give informed consent to be a part of this study and those who left against medical advice after provisional diagnosis were made. In this study, those female patients were also excluded with the age less than 16 years or more than 45 years.
Data analysis
Information was compiled on the pre-designed questionnaire. Data was analyzed on MS Excel, 2010.
Results
During the above mentioned period of September 2016November 2016, a total of 200 patients were included in this study out of which 162 women were being identified to have GDM. Among the screened GDM positive women, the majority of the women were in 5TH TO 8TH gestational week (2nd month of pregnancy) i.e. 65 cases as shown in (Figure 4.1). Then 34 cases were within 9th to 12th week, 28 cases were in1st to 4th week and19 cases were in17th to 20thgestational week. The least number of cases i.e. only 15 were being diagnosed during 17th to 20th week (Table 4.1).
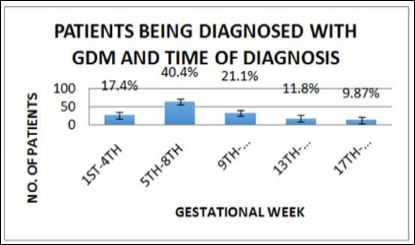
Figure 4.1: The percentage of patients being diagnosed with GDM and the time of diagnosis.
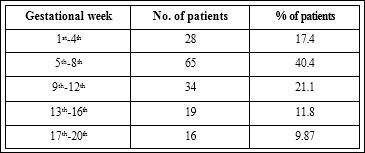
Table 4.1: The percentage of patients being diagnosed with GDM and the time of diagnosis.
In the current study we compared the prevalence of gestational and pregestational diabetes in pregnant women. Out of 200 patients, the majority of the cases were of GDM i.e. 162 (81%). The remaining cases (19%) were of pregestational diabetes i.e. type I or type II DM. 28 (5%) cases were being presented with Type I DM while 10 (14%) patients with Type II DM as shown in (Table 4.2) (Figure 4.2).
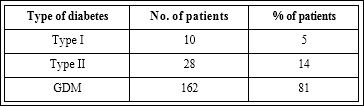
Table 4.2: Comparison of pre-gestational (type I, type II) and gestational diabetes.
In our study population 159 patients had foetal/neonatal complications while the remaining pregnancies were normal and controlled. The major complications found were macrosomia, hyperglycemia, CVS malformations, respiratory distress and stillbirth. Out of these, the most frequently occurring complication was hypoglycemic babies i.e.52%. Then at second number was respiratory distress 23%, at third number was macrosomia 16%, at fourth number was CVS malformations 7% and the least prevailing complication was still birth/miscarriage i.e. 2% as shown in (Table 4.3) (Figure 4.3).
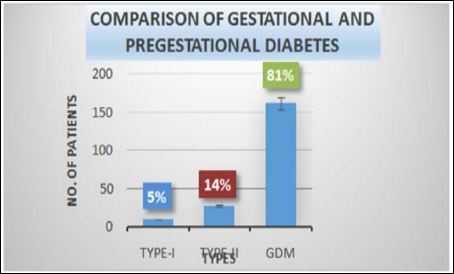
Figure 4.2: Comparison of gestational and pregestational (Type-I & Type-II) diabetes.
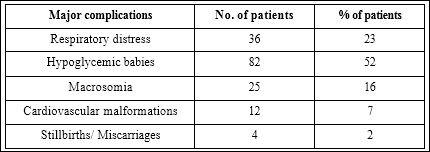
Table 4.3: Major feotal complicatioins in diabetic mothers.
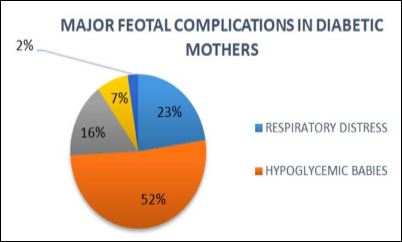
Figure 4.3: Majorfoetal complications in diabetic mothers.
Out of 200 patients 41 patients had miscarriage due to one of the following reasons. The major reason of miscarriage in diabetic mothers was found to be hypertension and out of 41 cases there were 17 (41.5%) cases of miscarriage due to hypertension. There were 10 (24.3%) cases of miscarriage due extreme sugar level, 9 (22%) cases of miscarriage due to polyhydramnios and 5 (12.2%) cases of miscarriage due to Hughes syndrome as shown in (Table 4.4) (Figure 4.4).
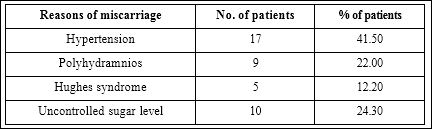
Table 4.4: Reasons of miscarriages in diabetic mothers.
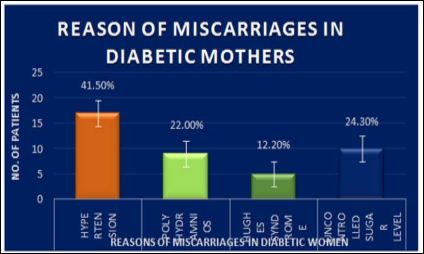
Figure 4.4: Reasons of miscarriages in diabetic mothers.
In our study population, the ratio of the normal and CS delivery was being determined. Out of 200 patients who were included in this study, 105 were being delivered during our study period.28% (29) cases were of normal delivery whereas 72% (76) cases were of C-section as shown in (Table 4.5) (Figure 4.5).
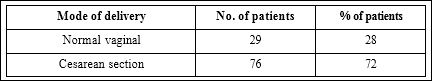
Table 4.5: Normal delivery VS C-section delivery.
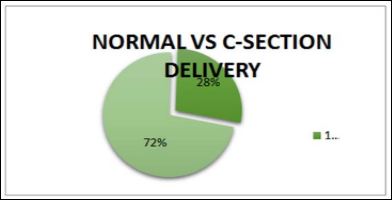
Figure 4.5: Normal delivery VS C-section delivery.
Out of 105 patients who were being delivered during our study period, there were 76 cases of CS. The major reasons of CS found out were as shown in the following figure. The major reason of CS was fetal distress and we found 35 (46.05%) such cases. Then at second place was the placental abruption with 15 (14.47%) cases, third major reason was dystocia with 11 (19.74%) cases and the fourth major reason was uterine rupture with 10 (13.16%) cases. The least reason of CS was breech position and we found only 5 (6.58%) such cases as shown in (Table 4.6) (Figure 4.6).
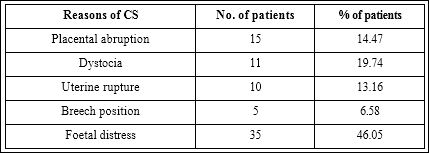
Table 4.6: Reasons for C-section delivery.
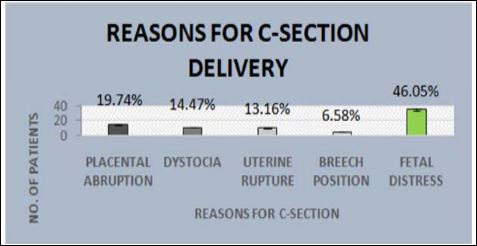
Figure 4.6: Reasons for C-section delivery.
Our study population of 200 patients was also being analyzed to check their TT status. So 76% (153) of the pregnant ladies were found to be vaccinated for tetanus while 24% (47) of the pregnant women were not being vaccinated as shown in (Table 4.7) (Figure.4.7).
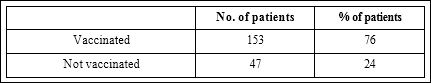
Table 4.7: Tetanus toxoid vaccination status analysis.
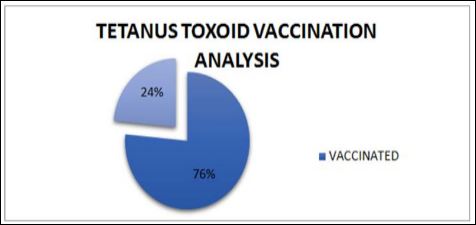
Figure 4.7: Tetanus toxoid vaccination status analysis.
Discussion
This study was conducted to determine the occurrence of GDM and the birth complications in diabetic mothers. In the estimation of the prevalence of GDM during different gestational weeks, it was found out that although GDM manifests in all trimesters of pregnancy, but in majority of the cases GDM occurs in early gestational weeks. Screening for GDM is usually performed around 24-28 weeks of gestational age. In a recent study a total of 4151 consecutive pregnant women irrespective of gestational weeks attending antenatal health posts across Chennai city underwent a 75 g OGTT (oral glucose tolerance test) recommended by WHO and diagnosed GDM if 2hr PG value ≥ 140 mg/dl. Observation in this study was that 38.7% women developed GDM even prior to 24th week of gestation [32]. Our results are very much similar to this study. So the OGTT must be performed in pregnant women prior to 24 weeks of gestation for better hyperglycemic control and to reduce the risk of birth complications.
During pregnancy, out of all types of diabetes most prevailing type is GDM. In the current study, 162 (81% of the total cases) wom- en were presented with GDM, while with type I only 5% and with type II 14%. So the risk of GDM is more in Pakistan. A recent study analyzed 1,729,225 Canadian women and found that the prevalence of gestational and pregestational diabetes in 1996 was 2.7% and 0.4%, respectively [33]. In another study, rates of gestational diabetes (Class A1 combined with Class A2) and pregestational diabetes were 2.0% and 0.3%, respectively [34]. Our results were similar to these studies in a sense that the ratio of gestational diabetes is more as compared to pregestational diabetes among pregnant women in Pakistan. The maternal diabetes is associated with a large number of complications in foetus and neonate. Patients who cannot control their diabetes with diet and exercise only, require insulin, which leads to state of hyperinsulinemia in the foetus of such mothers. This and many other reasons lead to the foetal complications. Postnatal hypoglycemia, respiratory distress, macrosomia, CVS malformations and stillbirths are major complications in the babies born to the diabetic mothers. The current study has shown that these complications are frequently occurring in the neonates and foetus of diabetic mothers. In recent years a study was performed to determine the range of complications occurring in infants of diabetic mothers. A total number of 40 babies were included in this study.35% new borns presented respiratory distress and8% were having CVS malformations. Hypoglycemia was noted in 50% [22]. Another study was being performed to compare the prevalence at live birth and the spectrum of cardiovascular malformations in infants born to diabetic mothers with that in infants of non-diabetic mothers. This study concluded that maternal diabetes is associated with a fivefold increase in risk of cardiovascular malformations. Transposition of the great arteries, truncus arteriosus, and tricuspid atresia are overrepresented to produce a substantial excess of these malformations [35]. All these previous studies strongly support our results.
Pregnancy affects both the maternal and fetal metabolism and even in nondiabetic women exerts a diabetogenic effect. Pregnancy loss is significantly higher among women with diabetes compared to the nondiabetic population. Neonatal mortality is also higher among infants of diabetic mothers in approximately 15-fold when compared to the general population [36]. Recently, a population-based cohort study conducted in the UK has shown that women with type 1 diabetes have a higher risk of late fetal loss, presenting a fourto five-fold increase in perinatal death, and a fourto six-fold in stillbirth [37]. The major reasons of miscarriages in diabetic women include hypertension, Hughes syndrome, polyhydramnios and uncontrolled sugar level; hypertension and pre-eclampsia being the root cause.
The prevalence of births worldwide complicated by DM is increasing. In the UK, for example, <25% of diabetic women have a non-instrumental vaginal delivery. Strikingly, more than half the CS in these patients was non-elective, but the reasons for this are not understood. This recent study tested the hypothesis that poor myometrial contractility as a consequence of the disease contributes to this high CS rate. There was significantly decreased contraction amplitude and duration in uteri from diabetic compared with control patients. There is poorer contractility even in the presence of oxytocin. The underlying mechanism is related to reduced Calcium channel expression and intracellular calcium signals and a decrease in muscle mass. This study concluded that these factors significantly contribute to the increased emergency CS rate in diabetic patients. It showed a high induction of labor rate (39%) and a high C-section rate (67%) in women with type I and type II DM as compared to 21% of the general maternal pop- ulation [38]. These results strongly support our current study which showed that 72% of the total deliveries were through CS.
The rise in the rate of cesarean sections in diabetic mothers is due to widening of the relative indications, such as dystocia, previous cesarean, fetal distress and breech presentation. In a recent study increase in the cesarean rate of 6.2% points was partitioned according to five complications of delivery including previous cesarean delivery, breech presentation, dystocia, fetal distress, and all other complications. Nearly half (48%) of the increase was associated with previous cesarean delivery, 29 per cent with dystocia, 16 per cent with fetal distress, 5 per cent with breech presentation, and 2 per cent with all other complications [39]. In the current study we examined the recorded indications of the CS and most common of them were fetal distress, placental abruption, dystocia, uterine rupture and breech position respectively. Previous CS was also a reason of CS in index deliveries.
Tetanus is an acute, often fatal, disease caused by an exotoxin produced by Clostridium tetani. It occurs in newborn infants born to mothers, who do not have sufficient circulating antibodies to protect the infant passively, by transplacental transfer. Prevention may be possible by the vaccination of pregnant or non-pregnant women, or both, with tetanus toxoid, and the provision of clean delivery services. Tetanus toxoid consists of a formaldehyde-treated toxin which stimulates the production of antitoxin. Recently a study was conducted to determine the TT vaccination status for pregnant women, and to examine the effects of various factors on TT vaccination coverage during pregnancy in reproductive-age women in Turkey. Four-hundred and ninety-three postpartum women who had live births at a hospital in Ankara were interviewed and information was collected on the mothers’ sociodemographic characteristics, TT vaccination history, and prenatal care during the pregnancy studied. The rates for no vaccination, one-dose vaccination, and two-dose vaccination were 53.3%, 18.9%, and 27.8%, respectively [40]. While in the current study, 76% of the screened women were being vaccinated with tetanus toxoid. This fact shows that maternal vaccination status is much better in Pakistan, but still more public awareness is required to boost up the rate of maternal vaccination in our country.
Conclusion
Diabetes is still a major problem of birth complications and miscarriages in Pakistan. In the current study we concluded that during pregnancy GDM is the most prevailing type of diabetes and it is associated with major birth complications including respiratory distress, hypoglycemic babies, macrosomia, CVS malformations and even miscarriages. Most of our patients were being diagnosed with GDM before 24th week of gestation. So a public awareness program is required to educate the people about reproductive health and to motivate them to undergo BSR/FBS during pregnancy prior to 24th gestational weeks to diagnose for GDM. This will lead to better glycemic control during pregnancy and decreased incidence of birth complications and miscarriages as according to our current study the major reason of miscarriages in diabetic mothers are hypertension and uncontrolled sugar level. From the current study we also concluded that the women being vaccinated with TT, are still at risk of GDM.
References
- Inzucchi SE, Sherwin RS (2011) Type 1 diabetes Cecil Medicine. 24th ed. Philadelphia, Pa: Saunders Elsevier.
- Assal J, Groop L (1999) Definition, diagnosis and classification of diabetes mellitus and its complications. World Health Organization 1-65.
- Stogdale L (1986) Definition of diabetes The Cornell veter- inarian 76: 156-174.
- Association AD (2010) Diagnosis and classification of diabetes mel- Diabetes care 33: S62-S69.
- Lawrence R (1951) Types of human diabetes. British medical jour- nal 1: 373.
- Cudworth A (1978) Type I diabetes Diabetologia 14: 281-291.
- Edelman SV (1997) Type II diabetes mellitus. Advances in internal medicine 43: 449-500.
- Soria B, Roche E, Berna G, León-Quinto T, Reig JA, et al. (2000) Insulin-secreting cells derived from embryonic stem cells normal- ize glycemia in streptozotocin-induced diabetic mice. Diabetes 49: 157-162.
- Landon MB, Gabbe SG (2011) Gestational diabetes mellitus. Ob- stetrics & Gynecology 118: 1379-1393.
- Kjos SL, Buchanan TA (1999) Gestational diabetes mellitus. New England journal of medicine 341: 1749-1756.
- Kopp W (2005) Role of high-insulinogenic nutrition in the etiology of gestational diabetes mellitus. Medical hypotheses 64: 101-103.
- Kühl C, Hornnes PJ, Andersen O (1985) Review: Etiology and pathophysiology of gestational diabetes mellitus. Diabetes 34: 66-
- Reece EA, Leguizamón G, Wiznitzer A (2009) Gestational diabetes: The need for a common ground. The Lancet 373: 1789-1797.
- Becerra JE, Khoury MJ, Cordero JF, Erickson JD (1990) ‘Diabetes mellitus during pregnancy and the risks for specific birth defects: A population-based case-control study’. Pediatrics 85: 1-9.
- Hod M, Merlob P, Friedman S, Schoenfeld A, Ovadia J (1991) Ges- tational diabetes mellitus: A survey of perinatal complications in the Diabetes 40: 74-78.
- Weintrob N, Karp M, Hod M (1996) Short-and long-range compli- cations in offspring of diabetic Journal of Diabetes and its Complications 10: 294-301.
- Dabelea D, Hanson RL, Lindsay RS, Pettitt DJ, Imperatore G, et (2000), Intrauterine exposure to diabetes conveys risks for type 2 diabetes and obesity: A study of discordant sibships. Diabetes 49: 2208-2211.
- Svare JA, Hansen BB, Mølsted-Pedersen L (2001) Perinatal com- plications in women with gestational diabetes mellitus. Acta obste- tricia et gynecologica Scandinavica 80: 899-904.
- Hyppönen E, Läärä E, Reunanen A, Järvelin MR, Virtanen SM (2001) Intake of vitamin D and risk of type 1 diabetes: A birth-cohort The Lancet 358: 1500-1503.
- Evers IM, De Valk HW, Visser GH (2004) Risk of complications of pregnancy in women with type 1 diabetes: nationwide prospective study in the Netherlands. Bmj 328: 915.
- Kerssen A, De Valk HW, Visser GHA (2006) Do HbA1c levels and the self-monitoring of blood glucose levels adequately reflect gly- caemic control during pregnancy in women with type 1 diabetes mellitus?. Diabetologia 49: 25-28.
- Alam M, Raza SJ, Sherali A, Akhtar A (2006) Neonatal complica- tions in infants born to diabetic mothers. Journal of the College of Physicians and Surgeons--Pakistan 16: 212-215.
- Al-Hakeem MM (2006) Pregnancy outcome of gestational diabetic mothers: Experience in a tertiary center. Journal of Family & Com- munity Medicine 13: 55-59.
- Rowan JA, Hague WM, Gao W, Battin MR, Moore MP (2008) Met- formin versus insulin for the treatment of gestational New England Journal of Medicine 358: 2003-2015.
- Clausen TD, Mathiesen ER, Hansen T, Pedersen O, Jensen DM, et (2008) High prevalence of type 2 diabetes and pre-diabetes in adult offspring of women with gestational diabetes mellitus or type 1 diabetes the role of intrauterine hyperglycemia. Diabetes care 31: 340-346.
- Lawrence JM, Contreras R, Chen W, Sacks DA (2008) Trends in the prevalence of preexisting diabetes and gestational diabetes mellitus among a racially/ethnically diverse population of pregnant women, 1999–2005. Diabetes carec31: 899-904.
- Ornoy A (2011) Prenatal origin of obesity and their complications: Gestational diabetes, maternal overweight and the paradoxical ef- fects of fetal growth restriction and macrosomia. Reproductive tox- icology 32: 205-212.
- Coustan DR (2013) Gestational Diabetes Clinical Chemis- try 59: 1310-1321.
- Rasmussen B, Dunning T, Hendrieckx C, Botti M, Speight J (2013) Transition to motherhood in type 1 diabetes: Design of the preg- nancy and postnatal well-being in transition questionnaires. BMC Pregnancy and Childbirth 13:
- Mohammadbeigi A, Farhadifar F, Soufi Zadeh N, Mohammadsalehi N, Rezaiee M, et (2013) Fetal Macrosomia: Risk Factors, Mater- nal, and Perinatal Outcome. Ann Med Health Sci Res 3: 546-50.
- Balaji V, Balaji MS, Datta M, Rajendran R, Nielsen KK, et (2014) A cohort study of gestational diabetes mellitus and complimentary qualitative research:Background, aims and design. BMC Pregnan- cy and Childbirth 14: 378.
- Seshiah V, Balaji V, Balaji MS, Paneerselvam A, Arthi T, et (2007) Gestational diabetes mellitus manifests in all trimesters of pregnan- cy. Diabetes Research and Clinical Practice 77: 482-484.
- Wen SW, Liu S, Kramer MS, Joseph K, Levitt C, et (2000) Impact of prenatal glucose screening on the diagnosis of gestational diabe- tes and on pregnancy outcomes. American journal of epidemiology, 152: 1009-1014.
- Sheffield JS, Butler-Koster EL, Casey BM, Mcintire DD, Leveno KJ (2002) Maternal diabetes mellitus and infant Obstet- rics & Gynecology 100: 925-930.
- Wren C, Birrell G, Hawthorne G (2003) Cardiovascular malforma- tions in infants of diabetic mothers. Heart 89: 1217-1220.
- Hawthorne G, Robson S, Ryall E, Sen D, Roberts S, et al. (1997) Prospective population based survey of outcome of pregnancy in diabetic women: Results of the Northern Diabetic Pregnancy Bmj 315: 279-281.
- Casson I, Clarke C, Howard C, Mckendrick O, Pennycook S, et al. (1997) Outcomes of pregnancy in insulin dependent diabetic wom- en: Results of a five year population cohort study. Bmj 315: 275-
- Al-Qahtani S, Heath A, Quenby S, Dawood F, Floyd R, et (2012) Diabetes is associated with impairment of uterine contractility and high Caesarean section rate. Diabetologia 55: 489-498.
- Taffel SM, Placek PJ, Liss T (1987) Trends in the United States cesarean section rate and reasons for the 1980-85 rise. American journal of public health 77: 955-959.
Citation: Ullah HH, Ullah HFK, Saleem HGM, Ullah W (2020) Study of Birth Com- plications in Diabetic Mothers, Dietary Supplements and their Associated Risks. J Diab Meta Syndro 3: 008
Copyright: © 2020 Ullah HH, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.