*Corresponding Author:
Rüştü Gedik,
Department of Oral Diagnosis and Radiology, Cumhuriyet University,Faculty of Dentistry, Sivas,Turkey.
Tel: +90 5357146360
Email: gedikrustu@gmail.com
Abstract
Stafne’s bone defects are asymptomatic lingual bone depressions of the lower jaw. There are two variant of Stafne’s bone defects, the common variant exists at the third molar region posterior of the mandible and the other anterior variant is relatively uncommon and is located in the premolar region anterior of the mandible. In the present study we described two cases with Stafne’s bone defects exists at the third molar region posterior of the mandible. The two cases were observed incidentally during routine radiographic examination.
Keywords
Lingual bone depressions; Stafne’s bone cavity; Stafne bone cyst; Stafne bone defect
Introduction
Stafne bone defect is known as Stafne bone cyst, also known as lingual mandibular salivary gland depression; latent bone cyst; static bone cyst; static bone defect or lingual cortical mandibular defect [1]. Edward C Stafne was the first to describe Stafne Bone Cyst in 1942 [2]. He described them as Bony Cavities in the posterior mandible [1]. These cavities are asymptomatic and are found only during routine radiography below the inferior alveolar canal, located distal to 3rd mandibular molar in the mandible and inferiorly limited by the mandibular border [3-5]. They are radiolucent and unilateral, and rarely bilateral [6].
Studies revealed that there are two variant of Stafne’s bone defects, the common variant exists at the third molar region posterior of the mandible and the other anterior variant is relatively uncommon and is located in the premolar region anterior of the mandible [7-10]. The incidence of Stafne’s bone defect ranges from 0.10% to 0.48% [2,6,7] with a male-to-female ratio of 4 to 1 [9-11]. Most of these painless lesions occur in the fifth and sixth decade of life. They are round or ovoid, and their sizes vary between 0.5 cm and 2.0 cm in diameter [3,8]. This lesion is easily diagnosed from the radiographs as they appear at a typical site & shape and clearly distinguished from its surroundings. CT scans add as important tool in confirmation of these lesions [12-17].
Cases Report
Case 1. A 42-year-old woman was referred to Cumhu riyet University, Faculty of Dentistry, Department of Dentomaxillofacial Radiology for routine dental examination and prosthetic management. Medical history and dental history were not contributory. Panoramic radiograph of the patient revealed a well-defined radiolucent area at the molar region posterior of the mandible below the mandibular canal (Figure 1). The defect shape like a saucer, which was diagnosed later as a stafne’s bone cavity The overlying mucosa of the defect was quite normal and there was not any sign of infection or fistula. The defect was unilocular , asymptomatic and no history of expansion was recorded.
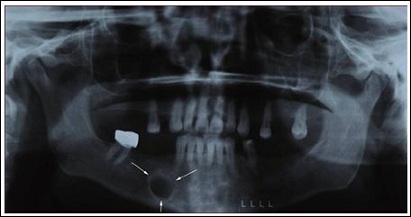
Figure 1: Case 1.A 42-year-old woman.
Case 2. A 39-year-old male patient was referred to Cumhuriyet University, Faculty of Dentistry, Department of Dentomaxillofacial Radiology in order to detect orijin of the severe pain, the panoramic radiograph revealed presence of profundd caries on the left maxillar poterior region which is underwent to surgical extraction. Also we observed radiographically the exist of a radiolucent defect on mandibular posterior region which was diagnosed later as a stafne’s bone cavity the shape of the defect was eliptic. Medical and dental history was not contributory. Palpation of the defect was not painful with no discomfort (Figure 2).
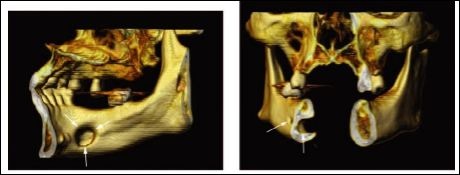
Figure 2: Case 2. A 39-year-old male patient.
Discussion
The Stafne’s defect is thought to be a normal anatomical variant, as the depression is created by ectopic salivary gland tissue associated with the submandibular gland and does not represent a pathologic lesion [2]. The differential diagnosis of Stafne’s defect is includes benign and malign jaw lesions such as odontogenic cystic lesion, Radiographically, it is a well-circumscribed, monolocular, round, radiolucent defect, 1-3 cm in size, usually between the inferior alveolar nerve and the inferior border of the posterior mandible between the molars and the angle of the jaw.[3-6]. It is one of the few radiolucent lesions that can occur below the inferior alveolar nerve ,with the exception of a portion of the submandibular gland [3-8]. The Stafne’s defect also tends to not increase in size or change in radiographic appearance over time and this can be used to help confirm the diagnosis. Also this defect is easily diagnosed from the radiographs as they appear at a typical site and shape and clearly distinguished from its surroundings [15,16]. The biopsy is not usually indicated, but if carried out, the histopathologic appearance is usually normal salivary gland tissue.
CT is more specific to bone lesions of the jaws and much less so to soft tissue have led some authors to advocate MR imaging as the primary diagnostic technique [16,17]. MR imaging should be adequate to make the diagnosis of stafne’s defect. Sialography is able to depict salivary tissue in the bony cavity and has been used to confirm the diagnosis [17,18].
In this paper, orthopantomograph is used for diagnosing the stafne’s defect (Unfortunately we hav’nt advanced non-invasive radiologic technique such CT to evaluate this position.
In conclusion, advanced non-invasive radiological assessment with CT scans is usually sufficient to achieve a final diagnosis of Stafne’s defect, and to avoid surgical interventions, which would be an unnecessary option in the management of Stafne’s defect except for symptomatic or concomitant other pathologies. In this paper, we are used only the orthopantomograph for diagnosing the stafne’s defect.
References
- Murdoch-Kinch CA (2004) Developmental disturbances of the face and jaws. In: White SC, Pharoah MJ (eds.). Oral radiology, principles and interpretation, (5thed). St. Louis, MO: Mosby-Year Book 639-657.
- Stafne EC (1942) Bone cavities situated near the angle of the Jour- nal of the American Dental Association 29: 1969-1972.
- Wray D, Stenhouse D, Lee D, Clark AJE (2003) Textbook of general and oral Edinburgh [etc.]: Churchill Livingstone. 236-237.
- Philipsen HP, Takata T, Reichart PA, Sato S, Suei Y (2002) Lingual and buccal mandibular bone depressions: a review based on 583 cases from a world- wide literature survey, including 69 new cases from Japan. Dentomaxillofac Radiol 31: 281-290.
- Burket LW, Greenberg MS, Glick M (2003). Burket’s oral medicine diagnosis & treatment (10th ) Hamilton, Ont. : BC Decker. 155.
- Soames JV, Southam JC (2003) Oral New York: Oxford University Press Inc 89.
- Grellner TJ, Frost DE, Brannon RB (1990) Lingual mandibular bone defect: report of three Journal of Oral and Maxillofacial Surgery 48: 288-296.
- Quesada-Gómez C, Valmaseda-Castellón E, Berini-Aytés L, Gay-Escoda C (2006) Stafne bone cavity: a retrospective study of 11 cases. Med Oral Patol Oral Cir Bucal 11: 277-280.
- Boyle CA, Horner K, Coulthard P, Fleming GJ (2000) Multiple Stafne bone cavities: a diagnostic Dent Update 27: 494-497.
- Prapanpoch S, Langlais RP (1994) Lingual cortical defect of the mandible: an unusual presentation and tomographic diagnosis. Dentomaxillofac Radiol 23: 234-237.
- Dereci O, Duran S (2012) Intraorally exposed anterior Stafne bone defect: a case Oral Surg Oral Med Oral Pathol Oral Radiol 113: 1-3.
- Aguiar LBV, Neves FS, Bastos LC, Crusoé-Rebello I, Ambrosano GMB, et al. (2011) Campos. Multiple Stafne bone defects: a rare entity. ISRN Dentistry 2011:
- Layne EL, Morgan AF, Morton TH (1981) Anterior lingual mandibular bone concavity: report of case. J Oral Surg 39: 599-600.
- de Courten A, Küffer R, Samson J, Lombardi T (2002) Anterior lingual man- dibular salivary gland defect (Stafne defect) presenting as a residual cyst. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 94: 460-464.
- White SC, Pharoah MJ (1981) Oral radiology principles and interpretation 5th St. Louis M: Mosby. 651-652.
- Branstetter BF, Weissman JL, Kaplan SB (1999) Imaging of a Stafne bone cavity: what MR adds and why a new name is needed. AJNR Am J Neurora- diol 20: 587-589.
- Smith MH, Brooks SL, Eldevik OP, Helman JI (2007) Anterior mandibular lingual salivary gland defect: a report of a case diagnosed with cone-beam computed tomography and magnetic resonance Oral Surg Oral Med Oral Pathol Oral Radiol Endod 103: 71-78.
- Segev Y, Puterman M, Bodner L (2006) Stafne bone cavity--magnetic reso- nance Med Oral Patol Oral Cir Bucal 11: 345-347.
Citation:Gedik TN, Gedik R, Gedik S (2017) Stafne’s Bone Cavity: Report of Two Cases. J Case Repo Imag 1: 003.
Copyright: © 2017 Gedik TN, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.


