*Corresponding Author:
Alvaro Hoyos,
Department of Pediatrics, Clínica Universitaria Bolivariana, Universidad Pontificia Bolivariana, Medellín, Carrera 72A No 78B50, Colombia, South America
Tel: 574 4455900
Fax: +574 4455762
Email: alvaromicro@hotmail.com
Abstract
Early-onset sepsis due to Streptococcus pneumoniae is a rare event. We present the case of a full-term baby delivered to a teen- age mother, who presented in the first hours of life with severe and rapid clinical deterioration. Steptococcus pneumoniae, serotype 19F, was isolated in both blood cultures.
Keywords
Early-onset; Neonatal sepsis; Serotype; Streptococcus pneumoniae
Introduction
Invasive disease in neonates due to S. pneumoniae is a rare event, both in well-developed and developing countries (<5% vs. 11.5%, respectively) [1,2]. Mortality is high, especially in early-onset sepsis cases (50%) and its clinical presentation is similar to cases of sepsis due to other microorganisms, like S. agalactiae and Escherichia coli [1,3-5]. The serotypes involved in neonatal infection do not appear to differ from those reported in older children and are recognized for their virulence, with some of them being included in the pneumococcal conjugate vaccines available in national vaccination programs [2,3,6,7]. We present the case of a newborn with a very early-onset pneumococcal pneumonia presenting with septic shock due to S. pneumoniae serotype 19F, leading to a fatal outcome.
Case Report
Full-term (38 weeks + 5 days) baby girl was born to a previously healthy, HIV-negative, first pregnancy, 16-year-old mother. Group B Streptococcus culture at 36 weeks of pregnancy was negative. She presented to the hospital in labor with premature rupture of membranes and clear amniotic fluid 9 hours prior to uncomplicated vaginal delivery. The baby weighed 2450 g, measured 50 cm long, had a head circumference of 35 cm and had Apgar scores of 9 and 10 at 1 and five minutes, respectively. At 2 hours of life, she developed progressive respiratory distress with expiratory grunting and low oxygen saturation without supplementary oxygen. She was transferred to the neonatal Intensive Care Unit, intubated, started on mechanical ventilation and underwent umbilical catheterization and resuscitation with intravenous fluid and inotropic support. Due to suspicion of early-onset neonatal sepsis, blood cultures were drawn and empirical antibiotic therapy was initiated with ampicillin and amikacin, according to the institutional protocol. Chest X-rays showed abundant alveolar infiltrates in both lungs with air bronchograms, suggesting surfactant consumption (Figure 1). The patient suffered progressive deterioration with refractory shock and multiple organ failure, and expired at 8 hours of life despite aggressive medical therapy. Blood cultures (automated BacT/Alert 3DTM, Biomérieux) taken 12 hours earlier grew Gram-positive cocci, which were finally identified as S. pneumoniae. The microbiological characteristics of this isolate are shown in the table 1. Other laboratory and microbiological studies (such as vaginal culture to search for S. pneumoniae in the mother-) could not be carried out due to the rapidity of the events.
Discussion
Streptococcus pneumoniae is an infrequent, but well recognized agent, causing neonatal sepsis (1-11%), and is usually associated with high morbidity and mortality [1,7]. In a recent review by Hoffman and colleagues of pneumococcal infections in pediatric hospitals in the United States, only 21 (0.5%) of 4428 episodes were in neonates, leading to a mortality of 14.3%; of these, 3 were early-onset sepsis (first 72 hours of life) and one of them occurred in the first 24 hours [3,5]. To our knowledge, this is the first reported case of neonatal early-onset sepsis due to S. pneumoniae in Colombia.
Early-onset invasive disease due to S. pneumoniae causes sepsis, meningitis and pneumonia. This last presentation is less common than in late-onset sepsis, but usually has a worst outcome, especially when it takes place in the first 48 hours of life [2].
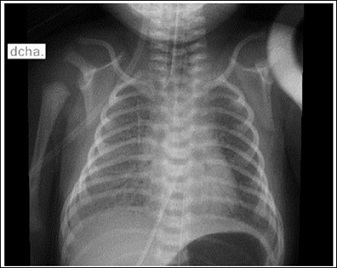
Figure 1: Chest X-rays at 5 hours of life in which mixed bilateral opacities and ground-glass appearance, suggestive of pneumonia caused by surfactant consumption, can be appreciated.
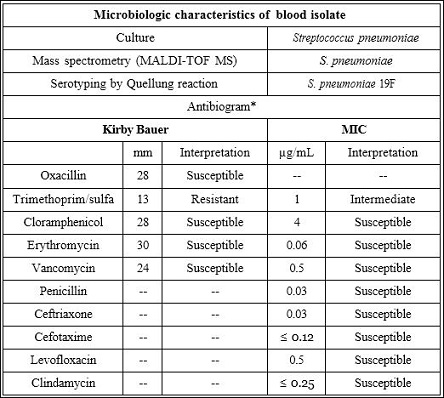
Table 1: Microbiological characteristics of S. pneumoniae isolated from blood cultures.
Abbreviations: MIC: Minimum Inhibitory Concentration; mm: millimeters; MALDI-TOF MS: Matrix-Assisted Laser Desorption Ionization-Time-Of-Flight Mass Spectrometry. *Clinical and Laboratory Standars Institute, 26th ed, 2016.
Clinical manifestations of pneumococcal sepsis in neonates do not differ from those found in sepsis due to S. agalactiae, E. coli and other bacteria [4,5]. Sepsis due to S. pneumoniae may have a very early (as in this case), early, or late-onset [8].
Passage through a colonized vaginal canal is considered the most important source of infection in cases of early-onset sepsis caused by pneumoniae [7]. Streptococcus pneumoniae has been isolated from maternal vaginal flora, although it is rare -0.03-0.75% [4,9,10]. Nevertheless, in early-onset cases, other potential sources of infection have been reported, including: transplacental infection through hematogenous spread in mothers with invasive pneumococcal disease and bacteremia; or also by ascending route in the female genitourinary tract [2,7]. In the postpartum period, infection can occur through contact with respiratory secretions in mothers or caregivers who are nasopharyngeal carriers of pneumococcus [1]. In this case, the absence of signs and symptoms of maternal infection, along with the normal appearance of amniotic fluid, suggests that infection in the newborn may have occurred through contact with the maternal genital tract during birth or, less probably, ascending through the ruptured membranes. It is possible that changes in sexual practices during pregnancy and the improvement of isolation and identification techniques for alpha-hemolytic Streptococcus explain an increase in the report of invasive infections secondary to pneumococcus in newborns [6,9]. Risk factors for early neonatal sepsis, such as duration of membranes rupture, gestational age and birth weight do not seem to be associated with S. pneumoniae sepsis in some reports [2,4,6,7]. Nevertheless, for other authors, besides the risk factors aforementioned, the severity of maternal disease with invasive pneumococcal infection could be associated with early neonatal sepsis [4,1,7]. Low pneumococcal antibody titers have been demonstrated in mothers of affected neonates, and it’s believed that there would be a higher risk of recurrent infection in subsequent babies [11].
Gómez and colleagues reviewed 119 cases of neonatal infection with S. pneumoniae and in 36 of those cases in which maternal cultures were positive (from the vaginal canal or another site) all neonates had early-onset sepsis [6]. This last observation suggests that there is a stronger relationship between invasive neonatal disease and maternal colonization with S. pneumoniae than with group B Streptococcus, since S. pneumoniae is rarely isolated from the female genital tract (≤0.75%), but has been reported in as many as 1-11% of neonatal sepsis cases [5].
Before the implementation of routinevaccination against pneumococcus with the heptavalent conjugated vaccine (2000, United States), the most frequent serotypes associated with invasive disease were: 4, 6B, 9V, 14, 18C, 19F y el 23F [12]. In neonatal invasive disease reports, the serotype involved was not always specified. Gómez and colleagues found that serotypes/serogroups: 1, 2, 3, 4, 6, 7, 8, 9, 10, 11, 18, 19, 28, 31 and 39 were implicated in 31 events of neonatal sepsis [6]. On the other hand, Hoffmann and colleagues stated that, in neonates with invasive disease, the most common serogroups/serotypes were: 19, 9, 3, 18, 14, 6, 1, 5 and 12 [3]. In both studies, the most frequent serotypes/
serogroups identified were: 19, 3, 9 and 14. Nonetheless, Fothy and colleagues, in a recent description of early neonatal pneumococcal sepsis and meningitis, found that the implicated serotype was 7A, a serotype included in the 13-valent conjugate pneumococcal vaccine [2]. Similar to this case, McAdams and colleagues notified the isolation of S. pneumoniae serotype 19F in an event of early-onset sepsis in a preterm, low-birth weight neonate [5]. In Colombia, vaccination against pneumococcus started 8 years ago with the heptavalent vaccine and later with the 10-valent vaccine, the latter being included in the current national immunization program. Both conjugate vaccines protect against serotype 19F. In the present case, given the maternal age, there was no previous history of pneumococcal immunization and, thus, a likely absence of immunity against serotype 19F.
Presently, there are no established protocols for the prevention of invasive pneumococcal disease in newborn children whose mothers’ genital tracts are colonized by S. pneumoniae or for mothers with a prior newborn who developed neonatal sepsis caused by pneumococcus. It might be reasonable to propose immunization against pneumococcus in expectant mothers fitting either profile, or the use of peripartum prophylactic antibiotics; however, to date, there are neither data nor recommendations to support either practice [2,9,10]. Given the low prevalence of pneumococcal colonization of the female genital tract, there is no indication for systematic screening in pregnant women [4].
Clarification
- Medical management was conducted promptly by intensivist due to the patient`s Blood culture was drawn and processed leaving them for incubation and after 12 hours they were positive, yet the baby had already passed away.
- At the time of bacteria identification the baby`s mother was al- ready
- We don`t have any additional available results from the newborn, except for blood cultures since they were not drawn.
Conclusion
In severe, early-onset neonatal sepsis events in children born to mothers with negative screening for Group B Streptococcus and with- out maternal antipneumococcal vaccination, S. pneumoniae should be considered as a possible etiologic agent in those whose preliminary blood cultures report Gram-positive cocci.
Acknowledgement
We wish to thank Adriana González, microbiologist at the Labora- torio Departamental de Salud Pública de Antioquia, for her technical support.
Declaration of Interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Singh J, Dick J, Santosham M (2000) Colonization of the female urogenital tract with Streptococcus pneumoniae and implications for neonatal disease. Pediatr Infect Dis J 19: 260-262.
- Fothy JF, Vetter S, Iñigo A, Gil J, Pérez JL, et al. Early-onset Streptococcus pneumoniae neonatal sepsis and meningitis in the 13-valent vaccine Pe- diatr Infect Dis J 32: 1299-1300.
- Hoffman JA, Mason EO, Schutze GE, Tan TQ, Barson WJ, et Streptococ- cus pneumoniae infections in the neonate. Pediatrics 112: 1095-1092.
- Barcos-Muñoz F, Moliner-Calderón E, Morales-Prieto R, Carrara-Scialpini L (2014) Neonatal sepsis and meningitis due to Streptococcus pneumoniae. Enferm Infecc Microbiol Clin 32: 58-59.
- McAdams RM, Garza-Cox S, Yoder BA (2005) Early-onset neonatal pneumo- coccal sepsis syndrome (2005). Pediatr Crit Care Med 6: 595-597.
- Gomez M, Alter S, Kumar ML, Murphy S, Rathore MH (1999) Neonatal Strep- tococcus pneumoniae infection: case reports and review of the Pe- diatr Infect Dis J 18: 1014-1018.
- Malhotra A, Hunt RW, Doherty RR (2012) Streptococcus pneumoniae sepsis in the newborn. J Paediatr Child Health 48: 79-83.
- Hermoso Torregrosa C, Carrasco Zalvide M, Ferrer Castillo MT (2012) Strep- tococcus pneumoniae: an unusual pathogen in neonatal sepsis of vertical Arch Bronconeumo l48: 425-426.
- Rodriguez BF, Mascaraque LR, Fraile LR, Perez IC, Kuder K (2015) Strep- tococcus pneumoniae: the forgotten microorganism in neonatal Fetal Pediatr Pathol 34: 201-205.
- Eperon I, Liberek C, Irion O, Martinez De Tejada B (2013) Neonatal pneu- mococcal sepsis associated with maternal tubo-ovarian abscess. J Obstet Gynaecol 33: 416-417.
- Khan A, Coughtrey H, Leroi MJ (2009) Streptococcus pneumoniae: uncom- mon cause of fatal neonatal sepsis. J Paediatr Child Health 45: 686-687.
- American Academy of Pediatrics (2015) Pneumococcal infections. In: Kim- berlin DW, Brady MT, Jackson MA, Long SS (eds.). Red Book: 2015 Report of the Committee on Infectious Diseases (30th edn). American Academy of Pediatrics (2015) Elk Grove Village, Illinois, USA Pg no: 626-638.
Citation:Hoyos A, Lambertino J, Vélez N, Trujillo M, Marín E, et al. (2017) Severe Early-Onset Neonatal Sepsis Due to Streptococcus pneumoniae Serotype 19F. A Case Report. J Perina Ped 1: 005.
Copyright: © 2017 Hoyos A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.