*Corresponding Author:
Janez Mohar,
Department of Spine Surgery, Valdoltra Orthopedic Hospital, Ankaran, Slovenia
Tel: +386 056696262
Email: janez.mohar@ob-valdoltra.si
Abstract
A sacral agenesia with insufficient bone stalk can pose a surgical problem of implant positioning when performing a spinal stabilization procedure. Additive Manufacturing Technology (AMT) has been increasingly used in the recent decade in spine surgery in complex spinal pathology.
A case of an adult female with a Currarino Syndrome (CS) is presented in which an instrumented lumbosacral fusion with sacroiliac (SI) fixation was indicated. The technical challenge of placing pedicle screws in an anomalous sacrum and iliac screws in a disproportionate pelvis was overcome by using a personalized guide for cannulating the bone, produced with the use of AMT. The patient’s Computed Tomography (CT) images of sacrum and pelvis were transferred to segmentation and preoperative planning software. The optimal position and dimension of screws were virtually planned in a three dimensional (3D) environment. The planned screw’s entry point and trajectory formed a basis for guide design and its final production with the use of selective laser sintering. During the operation, safe, accurate, and fast placement of sacral pedicle screws and iliac screws of optimum diameter and length was performed with an excellent clinical and radiological result.
The use of AMT or 3D printing in a patient with sacral agenesia has never been previously described.
Keywords
Additive manufacturing technology; Congenital anomaly; Iliac screws; Pedicle screws; Sacral agenesia; Spinal canal stenosis
Abbreviations
AMT: Additive Manufacturing Technology CS: Currarino Syndrome
SI: Sacroiliac
CT: Computed Tomography 3D: Three-dimensional
PSNG: Patient-specific Navigational Guides
S2AI: S2-alar-iliac
Introduction
CS is a form of caudal regression syndrome, characterized by a triad of anorectal malformation, sacral osseous defect, and presacral mass (ASP-association) that results from the abnormal separation of the neuroectoderm from the endoderm during embryological development. First described in 1981, it is caused by loss-of-function intragenic mutations and deletions of motor neuron and pancreas homeobox 1 gene MNX1 (previously named HLXB9), located at 7q36 and encodes a nuclear protein, homeodomain-containing transcription factor [1,2]. CS has an autosomal dominant pattern of inheritance with sporadic cases occurring in 30% and a variable phenotypic expression with the incomplete form being diagnosed predominantly in adults [3].
AMT or 3D printing has been used in the last decade in spine surgery for a better presentation of the pathology with anatomical models, for personalized implants and for safer, faster and cheaper implant placement in complex cases such as congenital deformities, severe thoracic scoliosis, and revisions of previously instrumented bone fusion mass with Patient-Specific Navigational Guides (PSNG) [4,5].
Case Report
A 39-year-old female with an incomplete form of CS was scheduled for an elective spinal canal decompression and fusion procedure due to her progressive symptoms of lumbar stenosis. Previously, she had an appendicovesicostomy (Mitrofanoff procedure) performed as a teenager and a left subtalar arthrodesis two years before admission. She complained of 10-year duration of a progressive left lower limb pain, worsening on sitting and walking. Her neurogenic intermittent claudication distance was assessed at 400 meters, and she had progressive paresthesias of the lower limbs. Upon examination, she had atrophies of both calves, cavovarus right foot deformity, a positive bilateral straight leg raise test at 60°, and her lower limb sensory function, muscle strength, and myotatic reflexes were otherwise healthy. Previous radiological workup revealed a central and lateral spinal canal stenosis from the third lumbar to the first sacral vertebra, intervertebral chondrosis at the L5-S1 segment, and a Type III sacral agenesis-subtotal sacral agenesis or sacral hypo development with S1 vertebra present (Figure 1) [6,7].
The preoperative plan consisted of a SI fixation in order to provide a strong basis for the lumbosacral instrumented construct due to the patient’s obesity, a possibility of a too weak fixation to the insufficient sacral bone and signs of lumbar instability of the L4-L5 segment on functional x-rays (range of motion was over 20°). The technical difficulty of having just one intraoperative possibility of cannulating S1 pedicles was acknowledged, and a decision was made to perform bilateral S1 pedicle screw fixation with the use of PSNG, produced by AMT. A possible second and further tries of S1 pedicle screw cannulation with the use of fluoroscopic guidance, as is a standard in our institution, would further decrease the already insufficient bone stalk and further lower the chances of a solid bone anchor purchase by a pedicle screw. Furthermore, the patient’s pelvis was narrow with decreased pubic arch, almost male-like, and placing optimum diameter and length of iliac screws for SI fixation with a free-hand technique was deemed somewhat cumbersome. Therefore, we opted for bilateral iliac wing cannulation by again using PSNG. The patient’s low-dose CT images of the lumbosacral spine combined with pelvis were transferred to segmentation and preoperative planning software (EBS, Ekliptik, Slovenia). After reconstructing a 3D bone model of the sacrum and pelvis, the optimum position of both S1 pedicle screws was planned in a virtual software environment by maximizing the diameter and length. The same procedure was used for both iliac screws’ position planning. The single PSNG model was designed for guiding both S1 pedicle screws’ and both iliac screws’ bone cannulation by virtually fitting four hollow cylinder bodies to a central geometric body. The latter had the surface layout inverse to the posterior sacral surface to tightly fit-and-lock to the bone when pressed down.
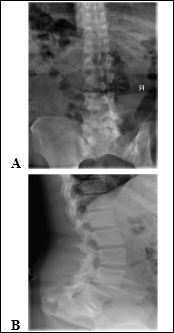
Figure 1: Preoperative anteroposterior (A) and lateral (B) x-ray images of the patent-note the sacral agenesia.
The position of the cylinder bodies on the central geometric body represented an extension of the S1 pedicle screws’ trajectories outside the sacrum and iliac screws’ trajectories outside the ilium. That way, drilling to a designated depth through hollow cylinders and into the bone, the S1 pedicle screws’ and iliac screws’ channels would be accurately and thus safely prepared (Figure 2). The PSNG was manufactured with the use of AMT, specifically from biocompatible polyamide (PA 2200, EOS, Germany) using selective laser sintering 3D printer (EOSINT P 396, EOS, Germany).
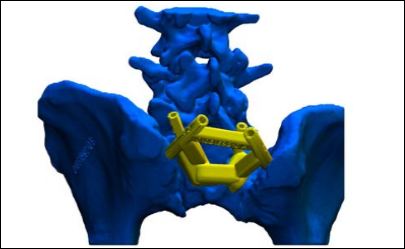
Figure 2: The virtual 3D model of the lumbar spine and pelvic girdle (blue) with the PSNG (green).
Intraoperatively, a standard midline approach from level L3 to sacrum was performed, followed by a meticulous soft tissue removal on the posterior elements of the sacrum and posterior superior iliac spines. The PSNG was fitted on the posterior sacral surface like lockand-key and was multi-directionally stabile. First, iliac screws’ cannulation was performed by drilling with a 4.5 mm drill bits that were left in place to further stabilize the PSNG (Figure 3). Next, a 3.2 mm drill bit was used to prepare the holes for bicortical S1 pedicle screw fixation. After checking the position of the drill bits on the fluoroscopy, the final tapping and screw placement followed. The dimensions of the S1 pedicle screws and iliac screws were 7.5×55 mm and 8.5×90 mm, respectively (CD Horizon Solera System, Medtronic, USA).
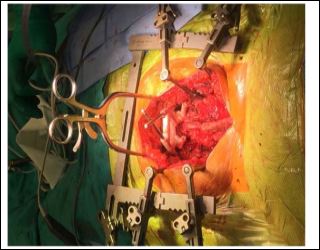
Figure 3: Intraoperative image of the PSNG fitted to the sacral osseous defect with iliac drill bits in place.
The operation concluded in a typical fashion with bilateral L3, L4 and L5 pedicle screw placement, extensive spinal canal decompression (which was absent at the level of the sacrum), L5-S1 discectomy and transforaminal implantation of the intervertebral polyether-ether-ketone cage (OPAL Cage System, DePuy Synthes, USA), and completion of the instrumentation construct by fixing double cobalt-chrome alloy rods to the pedicle screws’ heads and iliac screws’ heads through connectors (Figure 4).
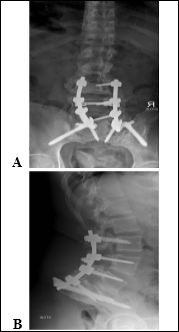
Figure 4: Postoperative anteroposterior (A) and lateral (B) x-ray images of the patent.
Discussion
Different types of mutations and variable expressivity of the MNX1 gene result in three main phenotypical subtypes found in CS; complete triad, mild form with a sacral anomaly, and either anorectal malformation or presacral mass, and minimal form with sacral anom- aly only [8]. Anorectal malformations are usually rectoperineal fis- tula, anorectal stenosis, anorectal atresia, or Hirschsprung’s disease, causing chronic constipation. A sacral osseous defect is ether type III (in 26.7%) or type IV-pathognomonic hemisacrum or “scimitar sign” (in 66.7%), according to Pang’s classification, causing neurogenic bladder, recurrent urinary tract infections or incontinence. Presacral mass is usually an anterior meningocele, epidermoid cyst, or teratoma with an estimated malignant incidence of 1 % [2,6-8]. 7q deletions cause a more severe clinical picture than intragenic mutations with possible intellectual disability, growth delay, facial dysmorphism, and associated terminal spinal cord malformations and urogenital malfor- mations [2].
Performing a stabile spinopelvic fixation is indicated in any form of sacral agenesis, representing an analogy of sacral insufficiency after sacral tumor resections. Modern sacroiliac augmentation of S1 pedicle screw fixation consists of either stabilizing the instrumenta- tion construct with iliac screws or S2-alar-iliac (S2AI) screws. A re- cent meta-analysis comparing the two techniques showed that S2AI screw fixation in adults has a significantly lower mechanical failure and complication rate than iliac screw fixation [9]. It is the standard at our institution to perform SI fixation with iliac screws in primary cas- es and reserve S2AI screw fixation for revision cases. The latter tech- nique may cause chronic pain by violating the sacroiliac joint while at the same time providing increased construct stiffness compared to iliac screw fixation [10].
PSNG have been shown to reduce the operation time, the risk of screw misplacement, and its consequent complications in the setting of severe congenital deformity pedicle screw instrumentation [11]. Since sacral agenesia of any type is regarded as a form of failure of formation, the analogy of AMT use in congenital deformity surgery has been drawn in the early stages of our patient’s treatment planning and has been proven successful.
Conclusion
Performing a SI fixation in a setting of a CS-associated sacral osseous defect can pose a technical challenge of placing anchoring implants in a correct position by using standard surgical techniques due to anomalous anatomy and altered anatomical proportions. In order to avoid possible complications from erroneously positioned pedicle or iliac screws, accurate guidance systems are indicated, such as an AMT-produced PSNG, as was in our case. Safe by being accurate, cheap by being a personalized 3D printed navigational guide and fast to work with intraoperatively, this technology is here to stay. To the best of the author’s knowledge, this is the first description of a spinopelvic fixation with the use of AMT in a patient with any form of sacral agenesia and the first description of a spinopelvic fixation in a patient with CS.
References
- Currarino G, Coln D, Votteler T (1981) Triad of anorectal, sacral, and presacral anomalies. AJR Am J Roentgenol 137: 395-398.
- Cuturilo G, Hodge JC, Runke CK, Thorland EC, Al-Owain MA, et (2016) Phenotype analysis impacts testing strategy in patients with Currarino syndrome. Clin Genet 89: 109-114.
- Köchling J, Pistor G, Märzhäuser Brands S, Nasir R (1996) The Currarino syndrome--hereditary transmitted syndrome of anorectal, sacral and presacral Case report and review of the literature. Eur J Pediatr Surg 6: 114-119.
- Wilcox B, Mobbs RJ, Wu AM, Phan K (2017) Systematic review of 3D printing in spinal surgery: The current state of J Spine Surg 3: 433-443.
- Cho W, Job AV, Chen J, Baek JH (2018) A review of current clinical applications of three-dimensional printing in spine Asian Spine J 12: 171-177.
- Pang D, Hoffman HJ (1980) Sacral agenesis with progressive neurological deficit. Neurosurgery 7: 118-126.
- Martucciello G, Torre M, Belloni E, Lerone M, Pini Prato A, et al. (2004) Currarino syndrome: Proposal of a diagnostic and therapeutic protocol. J Pediatr Surg 39: 1305-1311.
- Costanzo S, Spaccini L, Pio L, Mattioli G, Virgone C, et al. (2017) Currarino syndrome: Does the presence of a genetic anomaly correlate with a more severe phenotype? A multicentre J Pediatr Surg 52: 1591-1596.
- De la Garza Ramos R, Nakhla J, Sciubba DM, Yassari R (2018) Iliac screw versus S2 alar-iliac screw fixation in adults: A meta-analysis. J Neurosurg Spine 30: 253-258.
- Hoernschemeyer DG, Pashuck TD, Pfeiffer FM (2017) Analysis of the s2 Alar-Iliac Screw as Compared With the traditional iliac screw: Does it increase stability with sacroiliac fixation of the spine? Spine J 17: 875-879.
- Wu ZX, Huang LY, Sang HX, Ma ZS, Wan SY, et al. (2011) Accuracy and safety assessment of pedicle screw placement using the rapid prototyping technique in severe congenital scoliosis. J Spinal Disord Tech 24: 444-450.
Citation:Mohar J (2020) Sacroiliac Fixation with the Aid of a Personalized Navigational Guide in a Patient with Currarino Syndrome: Case Report. J Case Repo Imag 4: 013.
Copyright: © © 2020 Mohar J. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.


