*Corresponding Author:
Afaf Felemban,
Department of Obstetrics & Gynecology, King Abdullah International Medical Research Center/King Saud bin Abdul-Aziz University for Health Sciences, Saudi Arabia.
Tel: +966555441287
Email: fillimbana@ngha.med.sa
Abstract
Objective: Report a case of a difficult Robotic myomectomy after a failed uterine artery embolization (UAE).
Setting: King Abdul-Aziz medical city, Riyadh, KSA.
Case: A 48-year-old woman with menorrhagia secondary to an intramural fibroid (10x7 cm) underwent UFE 6 years prior to presentation Therefore, recurrence of symptomatic fibroid post UFE is not uncommon, to our knowledge only two cases reported in the literature with mention of Surgery details.
Intervention: Underwent da Vinci robotic-assisted laparoscopy resection of leiomyoma to our knowledge, this is the first report of robotic myomectomy performed after failure of UAE.
Result: Total robotic procedure was 145 minutes and estimated blood loss was 600 cc. due to degeneration of the fibroid and formation of alot of collateral vessels from previous UAE make the myomectomy very difficult and also increased in blood loss. As patient desires to preserve reproductive organs Myomectomy was done rather Hysterectomy. Patient was discharged uneventfully on the day 1postoperatively. Pathology result showed 270 grams leiomyoma of uterus and Patient present to 2 weeks’ post-operative visit with no more complaint of vaginal bleeding.
Conclusion: Myomectomy after UAE may be unusually difficult and increasing bleeding rate due to the degenerative changes and formation of collateral blood vessels that occur within the leiomyoma and degeneration so we recommend surgery to be done by expect and Robotic myomectomy would be very good choice if feasible.
Keywords
Myomectomy; Uterine Fibroid; Leiomyoma; Surgery, Uterine Artery Embolization (UAE)
Case Presentation
A 48 years old, presented with menorrhagia due to intramural fibroid, with History of uterine artery embolization bilaterally done using Embozene of same site uterine fibroid (Figure 1) 6 years prior to presentation. The uterine fibroid increased in size measures 10.4 x 7.2 x 10.0cm. Persistent fibroid was noticed in ultrasound 4 years after UFE but patient was asymptomatic at that time.
So patient Underwent robotic myomectomy as she was keen to preserve the uterus, intraoperative it was difficult myomectomy which easily bleeds more that expected for myoma and it has degeneration parts, Embolization materials were seen at the uterine artery level (Figure 2). Successfully whole myoma was removed weighing 270 grams Histopathology result came as Leiomyoma with degenerative changes with no atypia or malignancy.
Discussion
To our knowledge there are only two cases reported In literature as myomectomy post UFE with mentioning of Operative details , first case laparoscopy, a 7-cm peduculated myoma was growing from the serosa of the fallopian tube. It failed to respond to UAE and was removed by laparoscopic myomectomy [1]. Second one is a case of enlarging 18to 20-week-size fibroid uterus, underwent a difficult myomectomy after failed UAE. The myomectomy was only partially completed due to the difficult dissection of the myomas [2].
Surgery is well known treatment for symptomatic Fibroid as medical therapy did not prove its effectiveness yet. Furthermore, Fibroid Uterine artery embolization is well established option and it is known safe alternative especially for patient not considering future fertility [3].
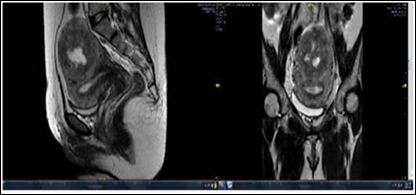
Figure 1: Fundal fibroid arising from the superior and posterior aspects. There is cen- tral cystic degeneration (about 10% necrosis).

Figure 2: Myomectomy showing emboshere materials..
Though FIBROID registry published 2008 reported that higher percentage of patients reporting improved symptoms, 92% in patient had UFE (33/36), verses 90% (26/29) in patient underwent Myomectomy (P =.78) [4]. However 10 percent of patient underwent UFE required further management either surgical intervention or repeated UFE in 3 years follow up. Broder MS et all reported higher rate of re-intervention when they Followed around 80 patient either underwent myomectomy or UFE, With variable follow-up period, embolization patients had higher percentage of requiring intervention (29% versus 3%) (P =.004) [5].
Higher percentage also proved by Cochrane review included Seven RCTs with 793 patients, reported that increased number of cases requiring reintervention in UFE group in comparison to surgical group .If we assume that 7% of women will require further surgery within two years of hysterectomy or myomectomy, between 15% and 32% will require further surgery within two years of UAE [6].
Thus although UAE is a safe, minimally invasive alternative to surgery, patient selection and counseling are essential to avoid requiring further surgical intervention [6]. For our case the approach was via Robotic -assisted laparoscopy which permits a surgeon sitting at a nearby console to control the laparoscopic arms with the use of a 3-dimensional camera [8]. Natural hand motions are replicated, eliminating the fulcrum effect seen with conventional laparoscopy in which ports serve as a fixed point around which force is applied [7].
There was a meta analysis done 2016 recruiting total, 2,027 patients comparing between the robotic myomectomy and the open one. Robotic approach showed superiority in estimated blood loss [92.78 ml/operation (95 % CI 47.26-138.29)], the need for transfusion [981 patients; odd ratio (OR) 0.20; 95 % CI 0.09-0.43], total complications (1101 patients; OR 0.31; 95 % CI 0.11-0.87) and in the length of hospital stay [1.84 days/patient (95 % CI 1.40-2.29)] over the open myomectomy [8]. Furthermore some have reported surgeon preference for robotic myomectomy in the case of ≥ 10 myomas ≤7 cm or obesity [9]. Retrospective review of 93 conventional laparoscopic and 89 robotic-assisted laparoscopic myomectomies noted that significantly more broad ligament and corporeal myomas were removed in the robotic cases, suggesting that robotic approaches may be best suited for the completion of more complex surgeries although this may reflect a selection bias [10]. This Study highlighted easier maneuverability with the use of robotic instruments, which was reported to aid in dissection and suturing [10]. Furthermore, The meta-analysis included 20 studies involving 2852 patients, Compared with Laparoscopy Myomectomy and Abdominal Myomectomy, Robotic Assisted Laparoscopic Myomectomy is associated with significantly fewer complications, significantly lower EBL, significantly fewer conversions than both Laparoscopy Myomectomy and Abdominal Myomectomy, and significantly less bleeding than Laparoscopy Myomectomy [11] .
Conclusion
Recurrence of fibroid after UFE is rare and might happen after years of successful procedure , and the case required surgical intervention surgery might be difficult due of collateral and fibriod degeneration so we recommend surgery to be done by expert and Robotic myomectomy might be good choice if feasible.
References
- Nelson HS, April DeW, Julie P, Anoosha G, Marjorie E, et al (2001) 1-Laparoscopic Myomectomy after Failure of Uterine Artery Embo- The Journal of the American Association of Gynecologic Laparoscopists 8: 583-586.
- Floyd SE, Proctor JA, Couchman G (2005) Abdominal myomecto- my after failed uterine artery embolization. Fertility and Sterility 83:
- Spies JB (2013) 3-Current Evidence on Uterine Embolization for Seminars in Interventional Radiology 30: 340-346.
- Scott CG, James BS, Robert WK, Eric P, Gaylene P (2008) Uter- ine Artery Embolization for Treatment of Leiomyomata: Long-Term Outcomes From the FIBROID Registry. Obstetrics & Gynecology 111: 22-23.
- Broder MS, Goodwin S, Chen G, Tang LJ, Costantino MM., et al. (2002) Comparison of long-term outcomes of myomectomy and uterine artery Obstetrical & Gynecology 100: 864-868.
- Gupta JK, Sinha A, Lumsden MA, Hickey M (2014) Uterine artery embolization for symptomatic uterine fibroids. Cochrane Database of Systematic Reviews.
- Advincula AP, Xu X, Goudeau S, Ransom SB (2007) Robot-assist- ed laparoscopic myomectomy versus abdominal myomectomy: A comparison of short-term surgical outcomes and immediate costs. Journal of Minimally Invasive Gynecology 14: 698-705.
- Iavazzo C, Mamais I, Gkegkes ID (2016) Robotic assisted vs lap- aroscopic and/or open myomectomy: Systematic review and me- ta-analysis of the clinical evidence. Archives of Gynecology and Obstetrics 294: 5-17.
- Vargas MV, Moawad GN, Sievers C, Opoku-Anane J, Marfori CQ, et al. (2017) Feasibility, Safety, and Prediction of Complications for Minimally Invasive Myomectomy in Women With Large and Numer- ous Myomata. Journal of Minimally Invasive Gynecology 24: 315-
- Barakat EE, Bedaiwy MA, Zimberg S, Nutter B, Nosseir M,, et al. (2017) Robotic-assisted, laparoscopic, and abdominal myomecto- my: a comparison of surgical outcomes. Obstetrics & Gynecology 117: 256-266.
- Wang T, Tang H, Xie Z, Deng (2018) Robotic-assisted vs. laparo- scopic and abdominal myomectomy for treatment of uterine fibroids: a meta-analysis. Minimally Invasive Therapy & Allied Technologies 27: 249-264.
Citation:Afaf F, Jawaher A, Reem A, Hanan A, Asem A, et al. (2019) Robotic myo- mectomy after failed uterine artery embolization. J Case Repo Imag 3: 008.
Copyright: © 2019 Afaf F, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.


