*Corresponding Author:
Elvis Chongsi Wam,
School of Medical and Biomedical Sciences, National Polytechnic University Institute Bamenda, Cameroon
Email: elviswam@yahoo.fr
Abstract
Background: Malaria is a deadly but preventable and treatable infectious disease transmitted by infected female anopheles mosquitoes. Each year, it kills >1 million people, most of them in Sub-Saharan Africa, where malaria is the highest cause of death for children under-five. In Cameroon, the mortality rate of malaria witnessed a rise from 17% in 2012 to 22% in 2013 with 45% of deaths in children under-five. Thus, the Cameroon government under the impetus of the Ministry of Public Health, came out with a policy in June 2014, implementing free treatment of severe malaria in children under-five. This study determined the state of implementation of this policy in health facilities of the Ndop Health District from July 2014 to 2017.
Methods: A cross-sectional study was conducted in September 2017, using purposive sampling to choose 21 health facilities in the Ndop Health District. Questionnaires were used to collect data from 21 consulting health personnel and 17 parents/guardians of children under-five suffering from severe malaria, with a retrospective data collection from the 1st of July 2014 to the 30th of June 2017.
Results: A total of 85.7% consulting health personnel were trained on the management of severe malaria. All the 21 health facilities had the treatment guide for the management of severe malaria. During data collection, most health facilities used artesunate (42.8%) and artemether (38.1%) as first line treatment for severe malaria in children below-five. Syringes were found to be available in all health facilities, while 76.2% and 61.9% health facilities, had stock outs in ar- tesunate and artemether respectively, within July 2014 to June 2017. All the 21 personnel were informed about free treatment policy, while only 41% parents/guardians of children below-five were aware of the policy. No child benefitted from free treatment during data collection.
Conclusion: The free treatment of severe malaria in children under-five has not been effectively implemented in the Ndop Health District as stipulated by the policy. Drugs should be supplied for free, community sensitized and a supervisory committee established for follow-up of implementation of this policy.
Keywords
Severe malaria; Free treatment policy; Children; Ndop Health Districty
Background
Malaria is a deadly but preventable and treatable infectious disease transmitted by infected female anopheles mosquitoes that kill more than one million people each year, most of them in Sub-Saharan Africa, where malaria is the leading cause of death for children under five [1]. About half of the worlds’ population (3.2 billion) is at risk of malaria with 97 countries reported to have an ongoing malaria transmission in 2015, inflicting a tremendous burden on countries in Sub-Saharan Africa [2]. Severe malaria is a life-threatening medical emergency and requires prompt and effective treatment to prevent death. Children under five and pregnant women are the most vulnerable to malaria, suffering from serious consequences of the disease, especially in regions where transmission is intense or stable. According to the World Malaria Report (2017), in 2016, there were 216 million cases of malaria, (with 90% occurring in the African Region) and 445,000 deaths (with 91% occurring in African Regions) [3]
In 2015, malaria killed an estimated 303,000 under-fives globally, including 292,000 in the African Region. Between 2010 and 2015, the malaria mortality rate among children under 5 fell by an estimated 35%. Nevertheless, malaria remains a major killer of under-fives, claiming the life of 1 child every 2 minutes [4]. Malaria is endemic in Cameroon, where it is the leading cause of morbidity and mortality [5]. According to the National Malaria Control Programme (NMCP), malaria accounts for 50-56% of morbidity and 40% of deaths among children less than five years of age [5]. Health statistics reveal that it is responsible for 24% of total deaths in health facilities, 40% to 45% of medical consultations and 30% of hospital admissions [6]. In addition, in 2011, 52% of consultations in children under five were due to simple and severe malaria [6]. More so, actions such as the free distribution of impregnated bed nets contributed in the reduction of malaria morbidity from 41% in 2008 through 36% in 2010 to 27% in 2012 [7]. The annual mortality rate from malaria in Cameroon dropped from 29% in 2009 through 25% in 2010 to 17% in 2012. However, the mortality rate witnessed a rise from 17% in 2012 to 22% in 2013 with 45% of deaths in children under five linked to malaria [8]. Thus, malaria remains a global health problem in Cameroon, and public health efforts today are focused on controlling it.
Faced with this situation, the Cameroon government under the impetus of the Ministry of Public Health, came out with a policy in June 2014, implementing free treatment of severe malaria in children under five. This policy consists of reducing the cost of managing severe malaria by offering drugs, inputs and diagnostic tests free to children under five. Four years into its implementation, only one study has been carried out in Cameroon in the Bamenda Health District to determine the level of implementation of free treatment of severe malaria in children under five years from July 2014 to June 2015 [9]. Thus, there is an urgent need of data to inform the health system pyramid on the state of implementation of the policy in the Ndop Health District, four years into its implementation. This study sought to determine the state of implementation of free treatment of severe malaria in children less than five years in health facilities of the Ndop Health District within the period of July 2014 to 2017.
Materials and Methods
Study Site
This study was carried out in the Ndop Health District of Cameroon. The Ndop Health District covers the entire Ngoketunjia Division with Ndop as the head quarter located about 60 km on the highway from Bamenda to Kumbo. The area is a low land surrounded by hills with streams that empty into the Bamenjim dam. All the 13 villages are accessible by road and 1 out of 15 health areas Mbissa by water; across the dam. Telephone and radio networks are within reach to the general population. In 2017 the total projected population was 267,506 inhabitants [10]. The district has a total surface area of 1126 km2. The Ndop Health District is made up of 1 administrative division and 3 sub-divisions that correspond to 3 council areas. The District has 15 Health Areas and 31 functional Health facilities; 16 government, 7 confessional and 8 lay private. Malaria is a major health problem in this District with 18,557 hospitalisations due to severe malaria registered in 2016 leading to 12 deaths, 6 of which were children less than five [11].
Study Design and Period of Study
A cross-sectional descriptive survey was conducted, with study population being consulting health personnel in health facilities and parents of children under five admitted for severe malaria in the Ndop Health District. The data collection phase of this research was carried out in September 2017, with a retrospective data collection from the 1st of July 2014 to the 30th of June 2017 in 21 health facilities.
Study Population
The study involved 21 consented consulting health personnel who carry out consultation and 17 parents or guardians of children under five years admitted for severe malaria in Health facilities of the Ndop Health District.
Inclusion Criteria
Operational Health facilities in which Health personnel give monthly reports on severe malaria.
Exclusion Criteria
Non-operational Health facilities within the last 3 months or operational but give no monthly reports on severe malaria.
Sampling Method and Sample Size
Health facilities were selected through non-probability sampling technique with the use of a purposive sampling. The reason for using the purposive sampling is because it aimed at getting valid information from a particular set of health facilities from the entire population. These health facilities were purposely chosen because they were best placed to provide the information needed for the study. A total of 21/31 health facilities were enrolled in this study (Figure 1). With regards to parents or guardians of under-five suffering from severe malaria, a sample size was not calculated. This is because the number of patients to meet at the time of data collection was not known. However, a total of 17 parents/guardians of under-five suffering from severe malaria were recruited in this study.
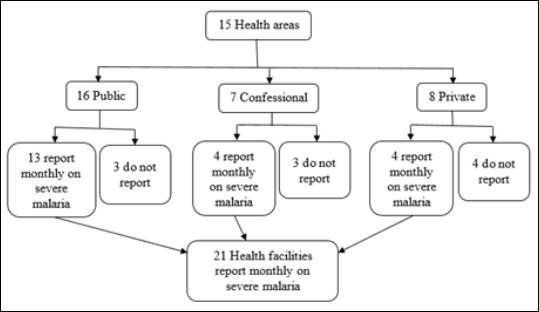
Figure 1: Sampling and sample size.
Data Collection
Two types of questionnaires were used. The first questionnaire was administered face to face to 21 consented consulting health personnel in the 21 chosen health facilities. Thereafter, a documentary review was done in the consulting register(s). Data from July 2014 to 30th of June 2017 on all suspected, confirmed and treated cases of severe malaria in children under five was collected. This first questionnaire was divided into five sections: the first having questions on the socio-demographic characteristics of participants and the other four; questions on the first three specific objectives of this study. The second questionnaire was administered face to face to 17 guardians or parents of children under five. It comprised of two sections: the first containing questions on socio-demographic characteristics and the second, questions on the fourth specific objective of this study, which sought to evaluate the degree of satisfaction of the beneficiaries (parents/guardians) of the free treatment initiative.
Data Management and Statistical Analysis
To ensure data quality, data collected with the questionnaires was double entered into two computers and analysed using Epi InfoTM version 7.2.0.1 and Excel 2013. Descriptive statistical analysis of data was also done with Epi InfoTM 7 programme. Frequency tables were used to determine the proportion of children treated with Artemether, Artesunate, Quinine injectable, and cases with laboratory diagnosis. Frequencies and medians were calculated, and rates (proportions) determined and presented in form of tables or figures depending on the variable. Ethical Considerations.
Given the fact that this research involves humans (participants, investigator), ethical consideration is mandatory. It is for this reason that we obtained a recommendation letter, from the Department of Biology of Higher Teacher Training College, Bambili, University of Bamenda, then submitted a research proposal to the North West Regional Delegation of Public Health for authorisation. Authorization was equally obtained from the Ndop District Medical Officer, as well as the general supervisors/directors/chiefs of each Health facility.
Information about this study, was explained to all the participants of this study (parents of children under 5 and health personnel), comprising of the potential risks linked to this study such as: violation of autonomy, rupture of confidentiality on the private data with regards to participants, exploitation of participants and inequality in risk/ benefit ratio and also rupture of social equilibrium in the community. Such potential risks were minimised by obtaining Informed Consents from participants before administering questionnaires, respecting the autonomy of participants. The data collection tool (questionnaire) was anonymous. Access to data was restricted only to those concerned with the research. This study is beneficial to the society as a whole in that the results we obtain will enable policy makers, stakeholders and the Cameroon Government through the National malaria control programme to provide strategies to ameliorate the implementation of such a policy. Thus, better management of severe malaria in children under 5.
Results
Socio-demographic Characteristics of Participants
This study carried out in the Ndop Health District involved 21 out of 31 health facilities and 17 parents/guardians of children under five suffering from severe malaria. All the health personnel consulting in the chosen health facilities during the data collection period were interviewed. The minimum age of health personnel was 25 years and the maximum was 50 years with age range of 25 years and median age of 32 years. Majority of the health personnel had ages greater than 32 years. There were more males (52.4%) than females (47.6%) (Table 1). A total of 17 parents/guardians of children below 5 were interviewed during the data collection period. Majority of the children were found in the age groups 13-25 months (41.2%) and 26-38 months (41.2%) with minimum and maximum ages of 8 months and 48 months respectively (Figure 2). Out of the 17 children, 64.7% of them were females while 35.3% were males. Mothers were found to be the primary care providers for their children accounting for 82.4%, while only 11.7% and 5.9% of sisters and aunts respectively were care providers for the admitted children under five years suffering from severe malaria within the period of study. Most of the parents/guardians of the children interviewed were farmers accounting for 82.4%, while 11.8% and 5.8% were students and civil servants respectively (Table 2). Also, all the interviewed parents/guardians, had attended school, majority of which ended just at the primary and secondary levels, with just one who had attended the tertiary level (Table 2).
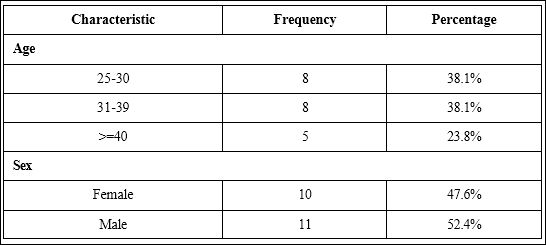
Table 1: Partition of health personnel according to age and sex.
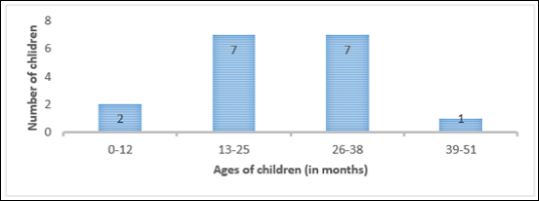
Figure 2: Partition of children under five according to age.
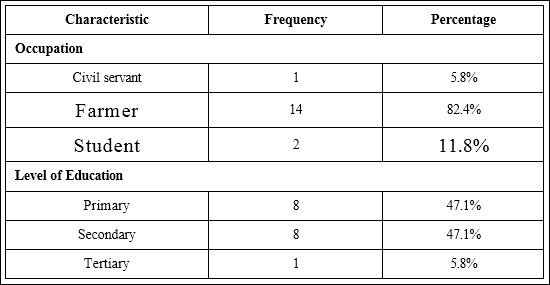
Table 2: Occupation and level of education of parents/guardians of children below-five.
Availability of Qualified Health Personnel for the Management of Severe Malaria
Highly qualified and well trained health personnel are indispensable for the proper suspicion, diagnosis, and treatment of severe malaria, and therefore ensure better management. State Registered Nurses (SRN) occupied the majority of the consulting health personnel, accounting for 33%, second by medical doctors (29%), with midwives having the least number (10%) (Figure 3). More than half (57.1%) of the consulting health personnel had from 1-5 years of working experience, with just one personnel having above 20 years of working experience (Table 3). The National Directives on the management of severe malaria in under-fives are supposed to be present in all health facilities including the price list for malaria cases in persons greater than 5 years. A total of 80.9% of the health facilities had these two documents, while only one health facility (4.8%) had none of these documents (Table 4). A total of 85.7% consulting health personnel were trained on the management of severe malaria in children below-five, the majority (47.6%) of which were trained in 2015 (Table 5). Only two health facilities (9.5%) had up to 6 health personnel trained for the management of severe malaria while 47.6% health facilities had just 1 trained health personnel, for the management of severe malaria (Figure 4).
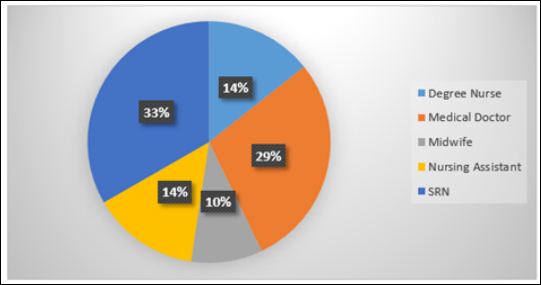
Figure 3: Qualifications of consulting health personnel
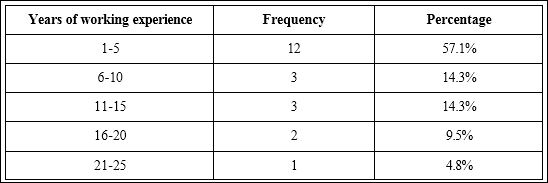
Table 3: Years of working experience of health personnel.
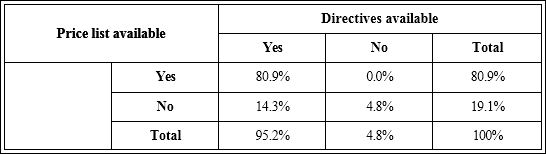
Table 4: Availability of Ministerial Directives and Price list on the free treatment Policy.
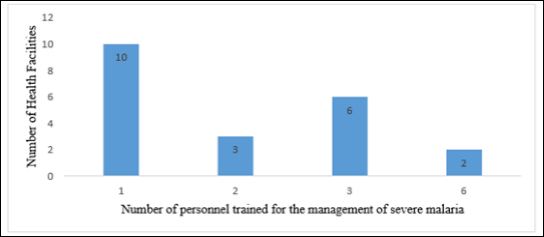
Figure 4: Number of personnel trained per health facility to manage severe malaria.
Adhesion of Health Personnel to Free Treatment Policy
All the 21 (100%) health facilities visited, had the treatment guide for the management of severe malaria in children below-five. The drug frequently administered as first line treatment for severe malaria in children below-five by most health facilities at the time of data collection was artesunate (42.8%) followed by artemether (38.1%). Quinine infusion was the least used, but the main drug used for second line treatment (80.9%) (Table 6). Quinine infusion was in all cases prescribed as first line drug due to its efficacy (100%), while artemether and artesunate were mostly prescribed as first line treatment in respect of the free treatment policy, accounting for 62.5% and 55.6% as against 37.5% and 44.4% for efficacy respectively (Table 7). According to national guidelines, all the cases of severe malaria must be confirmed with either Rapid Diagnostic Test (RDT), or microscopy before treatment. All the cases of malaria were confirmed before treatment, with the most frequent confirmatory test being RDT, accounting for 76.2%, while 23.8% cases were confirmed with microscopy. The most frequent means used in the various health facilities to sensitise the population on the free treatment policy was interpersonal communication during consultations accounting for 42.9%. The least was by community health workers (9.5%), while 28.6% health facilities did nothing towards informing the population about the policy (Table 8).
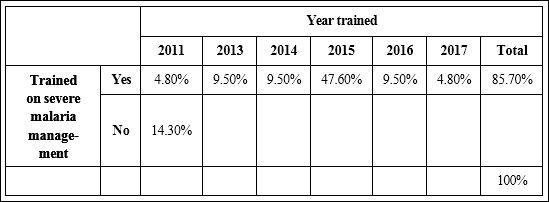
Table 5: Frequency of health personnel trained on the management of severe malaria and year trained.
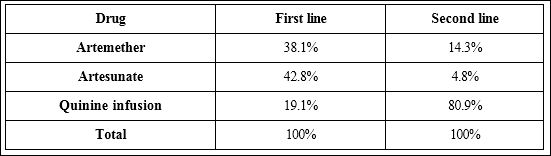
Table 6: Proportion of drugs administered for first line and second line treatment by health.
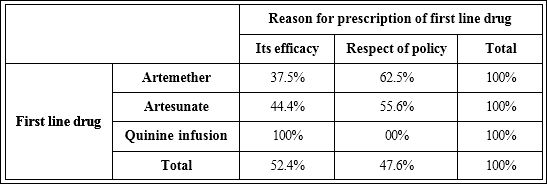
Table 7: Purpose for which drugs are prescribed as first line.
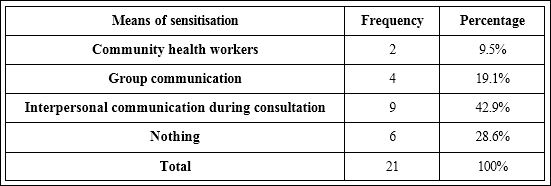
Table 8: Means of sensitising the population on free treatment policy.
Availability of Drugs and Inputs
Drugs and inputs availability play a major rule in the implementation of the free treatment policy. A total of 76.2%, 61.9%, 61.9%, and 38.1% health facilities had stock outs of artesunate, artemether, quinine, and RDT respectively. This stock out in artesunate, artemether and quinine was for more than 1 month in 9, 9, and 6 health facilities respectively. The only input that was available in all the health facilities from July 2014 to June 2017 was syringes. The majority of the health facilities had RDT (61.9%), and drip set (76.2%), available within this time frame (Table 9).
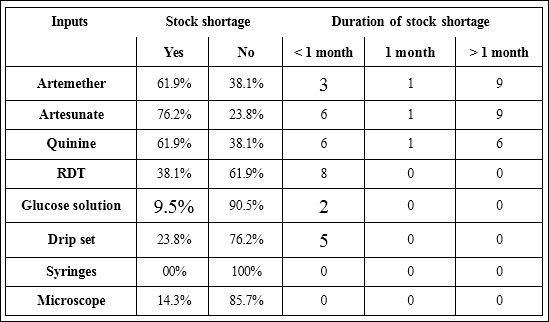
Table 9: Proportion of inputs shortage and its duration in the 21 health facilities in Ndop Health District from July 2014 to June 2017.
State of Implementation of the Free Treatment Policy
The free treatment policy was evaluated based on the number of children below-five with severe malaria, treated with injectable artesunate (60 mg) and injectable artemether (40 mg), since these drugs are supposed to be administered free of charge to treat severe malaria in children under five in Cameroon. There were more confirmed severe malaria cases in children below-five in 2016 than in 2015. Of the confirmed cases, only 16.7% and 9.0% were treated with the recommended first line drugs artemether and artesunate respectively in 2015, while the majority of cases (72.3%), were treated with quinine infusion, which is the recommended second line drug but emerged as first line treatment. In 2016, 6.7% and 14.5% of the confirmed cases were treated with artemether and artesunate respectively while 69.7% were treated with quinine infusion (Figure 5). However, during data collection, none of the 17 children we made in the various health facilities admitted for severe malaria was treated for free.
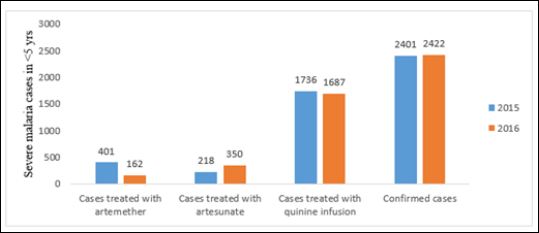
Figure 5: Evolution of the treatment of severe malaria for under-fives in 2015 and 2016 in 21 health facilities of the Ndop Health District.
Degree of Satisfaction/Awareness of Parents/Guardians of Children under Five
Of the 17 parents/guardians of children under-five interviewed in this study, 59% were not informed on free treatment policy, while 41% were informed, all of which got the information through friends. None of the children under-five, informed of the free treatment policy or not, was treated free of charge during the study period. The majority of the parents/guardians of the children below-five described the implementation of the free treatment policy in health facilities as bad, accounting for 64.7%, while 35.3% had nothing to say about the free treatment policy implementation.
Discussion
The purpose of this study was to assess the state of implementation of free treatment of severe malaria in children below-five years in health facilities of the Ndop Health District within the period of July 2014 to 2017. Of the 21 consulting health personnel interviewed, 52.4% were males and 47.6% females with the majority having ages greater than 32 years. This is contrary to findings in a study carried out in the Bamenda Health District in 2015 by Vukugah and colleagues, who found that 54.5% of the consulting health personnel were of the female gender and also that the majority of them had ages greater than 43 years [9]. The majority of parents/guardians of the children under-five interviewed were farmers (82.4%), 66.7% of which were mothers of the children. This was consistent to a study by Vukugah and colleagues, who reported that mothers were the primary care providers of children (73%) [9]. A total of 64.7% of the children under-five were females as against 35.3% males. As regards the availability of qualified health personnel, findings from this study showed that the majority of the consulting health personnel were State Registered Nurses (SRN) (33%). This is consistent with findings in a study conducted in the Bamenda Health District by Vukugah and colleagues, who found that 45% of the consulting health personnel were state registered nurses [9].
More so, a total of 85.7% consulting health personnel interviewed, were trained on the management of severe malaria in children below-five, the majority (47.6%) of which were trained in 2015. These findings are similar to a study conducted in the Bamenda Health District by Vukugah and colleagues, in which all (100%) the consulting health personnel had received training on the management of severe malaria, 86% of which did so in 2015 [9]. Similarly, Drissa in a study carried out in Bamako Health District in Mali in 2010, found that 96% of the interviewed health personnel had received training on the management of severe malaria [12]. However, other studies like that carried out in Uganda by Achan and colleagues, showed that only 22% of the health personnel were trained on the management of severe malaria [13]. This could be explained by the fact that, the study by Achan and colleagues, involved all health personnel whereas this study, that by Drissa, Vukugah and colleagues, involved only consulting health personnel.
Concerning the adhesion of health personnel to free treatment policy of severe malaria in children below-five, this study revealed that all the 21 (100%) health facilities visited, had the treatment guide for the management of severe malaria in children below-five. Similar results were obtained in Bamenda Health District and Bamako Health District, by Vukugah and colleagues and Drissa respectively, who reported that 95% and 96%, of the health facilities respectively had the management guides for malaria [9,12]. In addition, most health facilities at the time of data collection administered artesunate (42.8%) followed by artemether (38.1%), and lastly quinine infusion (19.1%) as first line treatment, but the main drug used for second line treatment was quinine infusion (80.9%). This was contrary to a study in Mazowe District, Zimbabwe, in 2014, where the treatment of severe malaria cases was done using mainly quinine injectable administered to 78.7% of cases [14]. Artesunate was not used because the health workers had not been trained on how to administer it [14]. The higher administration of artesunate as first line in this study was in line with the guidelines for the management of severe malaria in Cameroon (2017), which stipulates that injectable artesunate be used as first line treatment, and quinine injectable as second line and artemether injectable in case of contra indication of quinine.
This was also in line with the directives laid down by the Minister of public health on behalf of the Cameroon government on the free treatment of severe malaria in children under-five which stipulates that injectable artesunate and injectable artemether are drugs to be used free of charge to treat severe malaria in children under five, and that an eventual complication of treatment is an object for payment. However, a similar study carried out in the Bamenda Health District showed that 68.1% of the health facilities administered artemether as first line treatment, which was not in line with the guidelines for the management of severe malaria in Cameroon [9]. This could be explained by the fact that, at the time of this study, artesunate, which is the recommended first line drug was supplied to health facilities which was not the case in the study by Vukugah and colleagues. Parenteral artesunate is simple to administer, is safe, and reduces mortality substantially by 23% compared with quinine [15]. Quinine infusion was in all cases prescribed as first line drug due to its efficacy (100%), while artemether and artesunate were mostly prescribed as first line treatment in respect of the free treatment policy with percentages of 62.5% and 55.6% as against 37.5% and 44.4% for efficacy respectively.
This was similar to study in Mali by Drissa, who reported that 84% of consulting health personnel prescribed artemisinin-based combination therapy in respect of policy while only 12% did so for efficacy [12]. Moreover, all the 21 health facilities carry out a laboratory diagnostic test for severe malaria before treatment, with the most frequent confirmatory test being RDT (76.2%) against 23.8% for microscopy. This was in conformity with the guidelines for the management of severe malaria in Cameroon [16]. Same results were obtained in the study by Vukugah and colleagues in the Bamenda Health District [9]. However, in the study by Drissa, consulting health personnel showed a reluctance in carrying out a confirmatory test with just 32% interviewed consulting health personnel doing RDT before treatment, while in another study in Zimbabwe by Makumbe and colleagues, 97.5% of cases were diagnosed using RDT [12,14]. This high use of Rapid antigen Detection diagnostic Test (RDT) in this study could be explained by the fact that it is more widely accessible than expert microscopy, provides prompt results, is cost effective and is adequately sensitive for Plasmodium falciparum infections [17].
As concerns the availability of drugs and inputs, this study showed that 76.2%, 61.9%, 61.9%, and 38.1% health facilities had stock outs of artesunate, artemether, quinine, and RDT respectively, within July 2014 to June 2017. Vukugah and colleagues their study carried out in the Bamenda Health District documented that 36% of the health facilities had stock shortages of artemether within July 2014 to June 2015 [9]. This difference might be attributed to the fact that this study evaluated stock outs for a period of three years, whereas that of Vukugah and colleagues was just for a year. The only input that was available in all the health facilities from July 2014 to June 2017 was syringes. This was in conformity with findings by Vukugah and colleagues [9]. The evaluation of the state of implementation of the free treatment policy was done based on the number of children below-five with severe malaria, treated with injectable artesunate (60 mg) and injectable artemether (40 mg), since these drugs are supposed to be administered free of charge to treat severe malaria in children under five in Cameroon. In 2015, only 16.7% and 9.0% cases were treated with the recommended first line drugs artemether and artesunate respectively, while the majority of cases (72.3%), were treated with quinine infusion, which is the recommended second line drug but emerged as first line treatment.
In 2016, 6.7% and 14.5% of the confirmed cases were treated with artemether and artesunate respectively while 69.7% were treated with quinine infusion. Findings from a study in Bamenda Health District showed that only 32% health facilities treated severe malaria in under-five solely with artemether [9]. Although most health facilities at the time of data collection administered artesunate (42.8%) and artemether (38.1%), as first line treatment, the treatment was not for free, that is, none of the 17 children under-five years whom we made at the time of data collection, benefitted from the free treatment. This was consistent to a study in Bamenda Health District by Vukugah and colleagues, wherein no child below-five benefitted from free treatment meanwhile in a study carried out in Mali, 13.8% benefitted from free treatment [9, 12]. The lack of free treatment at the time of data collection in this study could be attributed to the fact that artesunate and artemether were not supplied for free as stipulated by the policy. More so, there were drug stock-outs and some health facilities preferred to use quinine infusion for the treatment since it is not for free. Finally, this study documented that, only 41% parents/caretakers of children below-five were aware of the free treatment all of which got informed by friends. This result is contrary to the 13% and 63.3% reported by Vukugah and colleagues and Drissa, respectively [9,12].
This difference could be due to a lack of sensitisation at community and hospital levels of the population about the free treatment policy. A total of 64.7% parents/guardians of children under-five described the implementation of the free treatment policy in health facilities as bad, while 35.3% had nothing to say. As a limit to this study, access to data was so difficult and some of the data was missing at the level of the various health facilities/district or present but not organised. Not all health facilities adequately indicated suspected cases of severe malaria in their consulting registers. The poor recording of such data in some health facilities influences the calculation confirmation rate of severe malaria. Thus, affecting the results of this study. The time frame for this study was not enough to have enough patients under five suffering from severe malaria in order to evaluate their level of satisfaction to free treatment policy of severe malaria. Thus the results from parents/guardians of under-fives cannot be generalised to the district. However, findings from this study can only be generalised to the Ndop Health District and not the North West Region nor Cameroon as a whole.
Conclusion
The free treatment of severe malaria in children under-five has not been effectively implemented in the Ndop Health District as stipulated by the policy laid down by the Minister of public health on behalf of the Cameroon government, on the 18th of June, 2014. A total of 85.7% of the consulting health personnel interviewed were properly trained on the management of severe malaria in children under-five, with at least one trained personnel in each health facility. The consulting health personnel somehow adhere to the free treatment policy, since 42.8%, and 38.1%, administered artesunate and artemether respectively, as first line treatment while 80.9% used quinine as second line drug at the time of data collection. Artesunate, artemether, quinine and other inputs, necessary for severe malaria management had stock outs at times but only syringes were available in all health facilities from July 2014 to June 2017. Drug supply has not been constantly offered free as prescribed by policy. No child below-five admitted for severe malaria was treated free of charge during the study period. A total of 59% of the parents/guardians of children under-five interviewed in this study were not informed of the free treatment policy, and 64.7% described the implementation of this policy as bad.
Recommendations
The following practices are thus recommended in the various levels of the Cameroon health system pyramid.
To Health facilities
- Step up ways to sensitise the general population on free severe malaria treatment, in order for all implicated actors to have the same definition of the said policy.
- Keep proper records and constantly give monthly reports on the management of severe malaria.
To District Health Service
- Perform a mass sensitization of the community at large on the free treatment policy and do a monthly supervision on the effective free treatment of severe malaria in under-five in health facilities.
- Improve on record keeping and ensure a proper monthly reporting by all health facilities on the treatment of severe malaria in under-fives.
North West special Fund for Health
- Supply inputs required for severe malaria management especially artemether and artesunate to both public, confessional and private health facilities on a monthly basis and on time.
- Create a supervisory committee to ensure the availability of inputs for severe malaria management in a bit to avoid stock outs.
Regional Malaria Control Unit
- Make available directives for free treatment of severe malaria in less than five and price list for treating severe malaria in persons above five years.
- Put in place a supervisory committee and elaborate a follow-up plan for the implementation of the free treatment policy in children below-five.
National Malaria Control Programme
- Perform research on the state of implementation of the free treatment policy in a large scale involving many other Health
- Estimate the financial impact on the implementation of the free treatment policy in confessional and lay private health facilities.
- Carryout research to evaluate the evolution of molecular markers of drug resistance to severe malaria four years after the implementation of the free treatment policy in Cameroon.
Contributors
ECW and MAT designed the study. ECW, LAA, ANW, JWTM and HSL administered questionnaires. LFS and HSL performed the statistical analyses. All authors participated in the write-up and approved the final version of the manuscript.
Acknowledgements
We thank the participants of this study who dedicated their time to grant us all the useful information and data for this study. Sincere thanks goes to the District Medical Officer of the Ndop Health District and his close staff for the assistance they gave which permitted us to easily get access to the various health facilities in the Ndop Health District.
Competing Interests
No conflict of interest declared.
References
- 1.Roll Back Malaria (2017a) For a malaria free world: About
- 2.Roll Back Malaria (2017b) For a malaria free world: Key
- 3.World Malaria Report (2017) Global disease burdens and 1-196.
- 4.WHO Factsheet (2016) World Malaria 1-186.
- 5.National Malaria Control Program (NMCP) (2014a) National strategic plan for malaria control. Health Ministry Cameroon report.
- 6.National Institute of Statistics (NIS) (2015) Annual statistics of Chapter 7: Health. 119-136.
- 7.Roll Back Malaria (2013) Consultation on Developing a Multi-sectoral Approach to Malaria World Health Organization, Geneva, 1-3 July 2013: Country-Brief-Cameroon, Malaria in Cameroon.
- 8.Global Fund (2014) Investing for impact against HIV, tuberculosis or ma- Global concept note Cameroon 1-48.
- 9.Vukugah AT, Zambou B, Nsalar MM, Josue WP (2018) The State of Im- plementation of Free Treatment of severe Malaria in Children Less Than Five Years in Health Facilities in the Bamenda Health District: A Cross Sectional Study. International Journal of Current Advanced Research 07: 9849-9854.
- 10.Ndop Health District Archives (2017).
- 11.Tchekountouo O, Col (2016) Rapport annuel des activités de lutte contre le paludisme dans le Nord-Ouest 1-45.
- 12.Drissa S, Alain Jourdain (2010) Evaluation du processus de mise en œu- vre du système de gratuité du traitement du paludisme chez les enfants de moins de cinq ans dans le district de Bamako.
- 13.Achan J, Tibenderana J, Kyabayinze D, Mawejje H, Mugizi R, et (2011) Case Management of Severe Malaria - A Forgotten Practice: Experiences from Health Facilities in Uganda. Plos One 6: 17053.
- 14.Makumbe B, Tshuma C, Shambira G, Mungati M, Gombe NT, et al. (2017) Evaluation of severe malaria case management in Mazowe District, Zim- babwe, 2014. Medical Journal 27: 33.
- 15.Dondorp AM, Fanello CI, Hendriksen ICE, Gomes E, Seni A, et (2010). Artesunate versus quinine in the treatment of severe falciparum malaria in African children (AQUAMAT): An open-label, randomised trial. Lancet 376: 1647-1657.
- 16.National Malaria Control Program (NMCP) (2014b) Guidelines for the management of malaria in Cameroon 74.
- 17.Bell DR, Wilson DW, Martin LB (2005) False-positive results of a Plas- modium falciparum histidine-rich protein 2-detecting malaria rapid diag- nostic test due to high sensitivity in a community with fluctuating low parasite American Journal of Tropical Medicine and Hygiene 73: 199-203.
Citation:Wam EC, Agyingi LA, Sama LF, Wam AN, Marbou J-WT, et al. (2021) Policy of Free Treatment of Severe Malaria in Children Less Than 5 Years in the Ndop Health District, North West Region of Cameroon. J Case Repo Imag 5: 044.
Copyright: © 2021 Wam EC, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.


