*Corresponding Author:
Mohamed Attia Ali Ahmed,
Ophthalmology Department, Faculty of Medicine, Minia University, Minia, Egypt
E-mail: mohamedattia27@gmail.com
Abstract
Purpose
To quantitatively assess vascular changes in retinal plexuses and choriocapillaries in patients with uveitis using Optical Coherence To- mography Angiography (OCTA).
Patients and Methods
Patients with confirmed diagnosis of uveitis and age-matched healthy controls were imaged by a commercial 70-kHz spectral do- main OCT system (RTVue-XR, Optovue). Macular 3x3 and 6x6mm2 scans with accepted quality were exported for customized process- ing that includes projection artifact removal, semi-auto segmentation of retinal layers, bulk motion subtraction and shadow artifact. Vessel densities were computed on Superficial Vascular Complex (SVC), Intermediate Capillary Plexus (ICP), Deep Capillary Plexus (DCP), and choriocapillaries compared between both groups using Mann– Whitney U test.
Results
Forty-seven eyes from 47 uveitic patients and 30 eyes from 30 age and gender-matched controls (43.90 ± 11.10, 52.28 ± 12.76 years) were studied. Parafoveal and perifoveal vessel density values were significantly lower in patients compared to controls (P=0.03 & 0.01) respectively. Both vessel and capillary densities were signifi- cantly reduced in patients compared to controls in all segmented retinal slabs; in both 3x3 and 6x6 mm2 macular scans; but the chorio- capillaries capillary density reduction was not statistically significant.
Conclusion
OCTA proved to be a promising non-invasive diagnostic tool for disease confirmation and monitoring in uveitic patients. Patients with uveitis have reduced macular and choriocapillaris vessel density compared to normal controls.
Keywords
Deep capillary plexus; Intermediate capillary plexus; Op- tical coherence tomography angiography; Superficial vascular com- plex; Uveitis; Vessel density
Abbreviations
OCTA: Optical Coherence Tomography Angiography;
SVC: Superficial Vascular Complex;
ICP: Intermediate Capillary Plexus;
DCP: Deep Capillary Plexus;
VD: Vessel Density;
CC: Choriocapillaries Complex;
SD: Standard Deviation;
n: Number;
%: Percentage.
Introduction
Uveitis is associated with macular pathological changes as the in- flammatory mediators play a key role in the disruption of the reti- nal microvasculature, leading to visually debilitating findings such as macular edema, retinal ischemia, and neovascularization (NV) [1-4].
Fluorescein Angiography (FA) is considered a cornerstone in eval- uating patients with uveitis, it may show dye leakage, vascular occlu- sion, or capillary dropout areas [4]. Visualizing retinal vasculature using FA was firstly reported in 1930 by Kikai. However, limitations of FA became obvious soon as it can visualize only the large superficial retinal vessels located within the nerve fiber and ganglion cell layers while perfusion of deeper retinal vasculature was not visible. Being an invasive imaging technique, most patients experience nausea and vomiting but still life-threatening complications such as anaphylaxis and cardiac arrest could be encountered in minority of patients; also, it could be contraindicated in patients with severe renal impairment [5,6].
Ultra-widefield FA has been considered to identify areas of retinal ischemia, leakage, and vasculitis which are not easily visible using the conventional FA imaging modality [7,8]. Comparing both modalities, the ultra-widefield FA quantitative studies were confounded by the relatively low-resolution images, distorted peripheral anatomy by im- aging artifacts, lid artifacts, and a limited time window for optimal imaging during the FA transit phase.
Moreover, and importantly, the captured wide-field images gener- ally do not provide high-resolution detailed images of the foveal cap- illaries where vision-threatening macular pathological changes most often occurs [8].
The relatively recent imaging modality Optical Coherence Tomog- raphy Angiography (OCTA) was demonstrated by Spaide et al. could image all layers of the retinal vasculature, including the deep layers, in contrast to FA imaging [9]. OCTA allows simultaneous visualiza- tion of the retinal vasculature and microstructure in a three- dimen- sional, depth-resolved fashion without need for dye injection and give high-resolution volumetric angiograms allowing the superficial and deep capillary plexuses to be studied separately [10].
OCT angiography utilizes motion contrast and back-scattered light of the moving RBCs to determine blood flow velocity in blood vessels. The recently developed SSADA (Split-Spectrum Amplitude Decorrelation Angiography) algorithm allows analysis of rapidly per- formed scans for variations in reflectivity, phase shift and variation to construct microvascular flow maps which constitute OCT angiog- raphy. Moreover, it can quantify retinal and choroidal blood flow via calculating the vessel density and blood flow index [11].
OCTA provides a quantitative estimate of retinal blood flow that is not possible using the largely qualitative fluorescein angiography modality. Also, it requires less time than fluorescein angiography, and does not confer the risks and side effects associated with fluorescein injection as it does not require dye injection.
In the current study, OCTA used to quantitatively assess the mi- crovascular changes in parafoveal and perifoveal retinal capillaries in patients with uveitis comparing them to healthy controls. We demon- strated the utility of OCT angiography in quantifying the macular, and choriocapillaris blood flow changes in a series of patients with uveitis.
Materials and Methods
Study design: Observational case-control comparative study.
Study population
The current study is an observational case series comparative study; included 47 eyes of 47 patients with confirmed diagnosis of uveitis (SLE, Behcet’s disease, sarcoidosis, multiple sclerosis associated with intermediate uveitis, idiopathic intermediate uveitis, and posterior uveitis) and 30 eyes of 30 healthy age and gender-matched controls. Patients of both genders were included. Exclusion criteria were those with opaque ocular media, refractive error ≥ 5 diopters, co-existent Age-related Macular Degeneration (AMD), macular scarring, cases with history of anti-VEGF injection and previous laser photocoagulation to the macula, retinal vascular occlusion or previous ocular surgery. Patients’ demographics are listed in (Table 1).
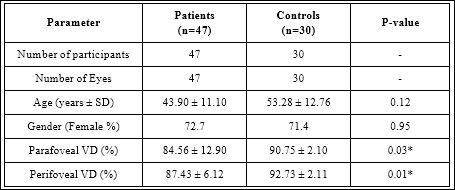
Table 1: Demographic criteria of study participants.
SD: Standard deviation, %: Percentage, VD: Vessel density, n: number, *: Statistically significant
Methods
All study participants were subjected to comprehensive history taking, ophthalmic examination including best corrected visual acuity, slit-lamp examination, intraocular pressure measurement, dilated fundus examination, and fundus fluorescein angiography (FAA).
OCTAscan capturing done using the commercial spectral-domain AngioVue OCTATM system (RTVue-XR Avanti, Optovue, Inc., Fremont, CA, USA) which is a 70-kHz spectral domain-OCT machine using an 840-nm wavelength scanning beam with an 70,000 A-scans/second acquisition and 5μm in-vivo axial resolution.
The built-in angio-analytic software automatically detect microvascular changes in both superficial and deep retinal vascular plexuses (SVP and DVP respectively) separately. The SVP was identified to be 3-15 µ below the Inner Limiting Membrane (ILM) and below the Inner Plexiform Layer (IPL) respectively, while DVP to be between 15 µ below the IPL and 71 µ below the IPL layer. Scans with accepted quality (signal strength ≥ 7) were exported for customized processing that included projection artifact removal, semi-automated segmentation of retinal layers, bulk motion subtraction and shadow artifact removal.
Semi-automated retinal segmentation was employed to define the anatomical boundaries of retinal vascular plexuses individually into Superficial Vascular Complex (SVC), Deep Vascular Complex (DVC) that is further included the Intermediate and Deep Capillary Plexuses (ICP and DCP) and Choriocapillaries Complex (CC). Vessel Density (VD) was calculated as the percentage of vascular pixels in en-face projections of the SVC, ICP and DCP within the effective analytic area at a time point.
Statistical Analysis
The Statistical Package of Social Sciences (IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp.) was adopted for tabulation and analysis the obtained data. Quantitative data were presented as mean ± standard deviation while qualitative data were expressed as number (n) and percentage (%). KolmogorovSmirnov for normality test was used to differentiate between parametric data and non-parametric data.
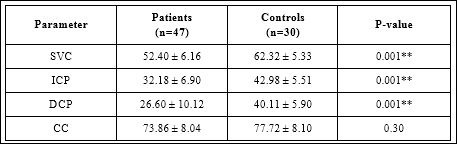
Table 2: Comparing vessel densities in segmented retinal and choriocapillaries layers in 3x3mm2 macular scans between patients and controls.
SVC: Superficial vascular complex, ICP: Intermediate capillary plexus, DCP: Deep capillary plexus, CC: Choriocapillaries complex, **: Statistically highly significant
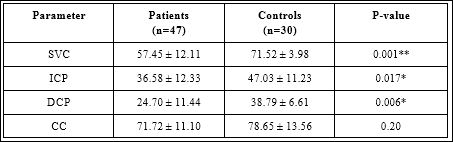
Table 3: Comparing vessel densities in segmented retinal and choriocapillaries layers in 6x6mm2 macular scans between patients and controls.
SVC: Superficial vascular complex, ICP: Intermediate capillary plexus, DCP: Deep capillary plexus, CC: Choriocapillaries complex, *: Statistically significant, **: Statis- tically highly significant
Independent sample t-test was adopted for analysis of quantitative data; Chi square test and Fisher Exact test were adopted for the analysis of the qualitative data. Vessel density values were computed in different retinal layers and compared between patients and controls using the non-parametric comparison Mann Whitney U test; P value < 0.05 is considered significant and < 0.001 is high significant.
Results
Forty-seven eyes of 47 patients with confirmed diagnosis of intermediate & posterior uveitis were compared to 30 eyes of 30 normal age and gender-matched controls were studied. Macular vessel density values were significantly lower in uveitic patients compared to controls in the three segmented retinal slabs in both 3x3 and 6x6 mm2. Capillary density in choriocapillaries also was found to be lower in patients but not statistically significant. Tables 2 and 3 shows vessel density values in segmented retinal layers and choriocapillaries in macula 3x3 and 6x6 mm2 scans respectively.
Positive correlation was found between parafoveal, and perifoveal vessel density values which showed to be only statistically significant in patients (Table 4).
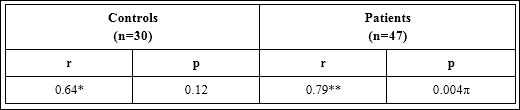
Table 4: Correlation between parafoveal and perifoveal vessel densities among controls and patients.
r: Correlation coefficient, *: Moderate correlation, **: Strong correlation, π : Statistically highly significant
Discussion
This study demonstrates presence of significant quantitative changes in the parafoveal capillary density in patients diagnosed with uveitis that can be reliably detected using OCTA imaging modality.
In a previous study of eyes with intermediate uveitis, with or without associated vasculitis and in the presence or absence of macular edema, found decreased retinal parafoveal capillary density together with qualitative changes of the FAZ [12].
Using the en-face swept source OCTA; uveitis cohort with and without choroidal involvement were compared to normal controls. Patients with posterior uveitis had significantly larger choriocapillaries flow deficits than those with other forms of uveitis, however; no significant differences were found between controls and patients without choroidal involvement [13].
Khairallah et al. studied 44 eyes of twenty-five patients diagnosed with clinically active Behçet uveitis and found that perifoveal microvascular changes were more frequently observed using the OCTA. The deep capillary plexus seemed to be more severely involved than the superficial capillary plexus.
Capillary vessel density was significantly lower in patients than in control group prominently in the deep capillary plexus. Disruption of the perifoveal capillary arcade, areas of retinal capillary nonperfusion/ hypoperfusion, and perifoveal capillary abnormalities, including rarefied, dilated, or shunting vessels were observed more frequently using OCTA than FA [14].
Kim et al. quantitatively analysed parafoveal capillary density in patients with uveitis and found significantly lower capillary density and complexity whether retinal layers boundaries identified by semi-automated or manual segmentation methods compared to healthy controls. Skeleton density and vessel density were significantly lower in the deep retinal layers of subjects with uveitis compared to healthy subjects. Worth noting that patients with anterior uveitis were included in their study, but we did not. Also, they analysed vessel density in the superficial and deep retinal layers not into segmented retinal slabs as in our study [15].
In a case-control, cross-sectional observational study of sarcoid eyes; the DCP was more affected by hypo-/non-perfusion than the SCP, but the SCP showed to be more affected by capillary abnormalities together with choriocapillaries flow void areas [16].
Our study showed that both vessel density of retinal vascular plexuses and choriocapillaries are significantly reduced in patients with uveitis compared to normal subjects as measured by OCT angiography. Analysis of both superficial and deep inner retinal capillary plexuses separately showed that those changes are more significant in the deep capillary complex (middle and inner retinal capillary plexuses).
Our findings support the histologic and FA findings of uveitis-associated retinal vascular changes in the macula and offer a foundation for future qualitative and quantitative studies on uveitic eyes using OCTA. Future studies using larger field of view on OCTA would be useful to investigate peripheral microvascular changes which have previously been documented with FA but without the level of quantified capillary details that OCTA provides [7,8].
In a study included eyes with Behçet’s disease, OCTA quantified associated microvascular changes that also proved to be more prominent in the deep capillary plexus than in the superficial layer [17].
In a case-control study of 29 eyes from patients with intermediate uveitis versus 30 healthy eyes, reduced vascular density and complexity in both superficial and deep retinal layers together with altered choriocapillaris perfusion were found [18].
In another prospective cross-sectional study included 156 eyes with intermediate uveitis; 36 of which had concomitant vasculitis, were evaluated using widefield swept-source SS-OCTA found reduced capillary non-perfusion and perfusion that were more frequently observed in the choroid, choriocapillaris, and deep capillary plexus than in the superficial capillary plexus [19].
Limiting our study, the non-randomized nature and the relatively small sample size included. Secondly, innocent vague nature of symptoms and preservation of good visual acuity until late in the course of some diseases. Thirdly, lacking the follow-up of cases raises the importance of a cohort longitudinal study in future studies for documenting the disease course and treatment effects.
An inherent limitation is associated with the currently used OCT-A system that we could go only through the choroid as deep as the choriocapillaries slab which was defined being 10µm deeper to Bruch’s membrane but no more through the deeper Sattler’s and Haller’s layers. Hence, a future enhanced-depth OCT-A protocol using the swept-source OCT is highly recommended for more accurate quantification of the microvascular changes which would be a helpful tool monitoring the disease activity and assessing treatment effects.
Declaration
Ethics approval and informed consent: the study research protocol was approved by the institutional review board at Faculty of Medicine Research Ethics Committee (FMREC), Minia University, Egypt. All study procedures were performed in compliance to the ethical standards guided by the institutional research committee together with the Helsinki declaration (1964) and its later amendments or comparable ethical standards. Informed consent was obtained from all subjects participated in the current study.
Data availability
Datasets analyzed in the current study are readily available on request from the corresponding author.
Funding
No funding received for the current study.
Competing interests
The authors declare that they have no competing interests.
Authors’ contribution
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Acknowledgment
Authors thank all subjects kindly agreed to participate in the current study.
References
- Liu T, Bi H, Wang X, Gao Y, Wang G, et (2015) Macular abnormalities in Chinese patients with uveitis. Optom Vis Sci 92: 858-862.
- Durrani OM, Tehrani NN, Marr JE, Moradi P, Stavrou P, et al. (2004) Degree, duration, and causes of visual loss in uveitis. Br J Ophthalmol 88: 1159-1162.
- Freeman G, Matos K, Pavesio CE (2001) Cystoid macular oedema in uveitis: An unsolved Eye (Lond) 15: 12-17.
- Antcliff RJ, Stanford MR, Chauhan DS, Graham EM, Spalton DJ, et al. (2000) Comparison between optical coherence tomography and fundus fluorescein angiography for the detection of cystoid macular edema in patients with Ophthalmology 107: 593-599.
- Xu J, Han S, Balaratnasingam C, Mammo Z, Wong KS, et al. (2015) Retinal angiography with real-time speckle variance optical coherence tomograBr J Ophthalmol 99: 1315-1319.
- Kwan AS, Barry C, McAllister IL, Constable I (2006) Fluorescein angiography and adverse drug reactions revisited: The Lions Eye Clin Exp Ophthalmol 34: 33-38.
- Hong BK, Nazari Khanamiri H, Rao NA (2013) Role of ultra-widefield fluorescein angiography in the management of Can J Ophthalmol 48: 489-493.
- Karampelas M, Sim DA, Chu C, Carreno E, Keane PA, et (2015) Quantitative analysis of peripheral vasculitis, ischemia, and vascular leakage in uveitis using ultra-widefield fluorescein angiography. Am J Ophthalmol 159: 1161-1168.
- Freiberg FJ, Pfau M, Wons J, Wirth MA, Becker MD, et (2016) Optical coherence tomography angiography of the foveal avascular zone in diabetic retinopathy. Graefes Arch Clin Exp Ophthalmol 254: 1051-1058.
- Spaide RF, Klancnik JM, Cooney MJ (2015) Retinal Vascular Layers Imaged by Fluorescein Angiography and Optical Coherence Tomography Angiography Imaging of Retinal Vascular Layers Imaging of Retinal Vascular JAMA Ophthalmol 133: 45-50.
- Jia Y, Tan O, Tokayer J, Potsaid B, Wang Y, et al. (2012) Split-spectrum amplitude-decorrelation angiography with optical coherence tomography. Opt Express 20: 4710-4725.
- Dingerkus VLS, Munk MR, Brinkmann MP, Freiberg FJ, Heussen FM, et (2019) Optical coherence tomography angiography (OCTA) as a new diagnostic tool in uveitis. J Ophthalmic Inflamm Infect 28: 9-10.
- Chu Z, Weinstein JE, Wang RK, Pepple KL (2020) Quantitative Analysis of the Choriocapillaris in Uveitis Using En Face Swept-Source Optical Coherence Tomography Am J Ophthalmol 218: 17-27.
- Khairallah M, Abroug N, Khochtali S, Mahmoud A, Jelliti B, et (2017) Optical Coherence Tomography Angiography in Patients with Behçet Uveitis. Retina 37: 1678-1691.
- Kim AY, Rodger DC, Shahidzadeh A, Chu Z, Koulisis N, et al. (2016) Quantifying Retinal Microvascular Changes in Uveitis Using Spectral-Domain Optical Coherence Tomography Angiography. Am J Ophthalmol 171: 101-112.
- Cerquaglia A, Iaccheri B, Fiore T, Fruttini D, Belli FB, et al. (2019) New insights on ocular sarcoidosis: An optical coherence tomography angiography Ocul Immunol Inflamm 27: 1057-1066.
- Somkijrungroj T, Vongkulsiri S, Kongwattananon W, Chotcomwongse P, Luangpitakchumpol S, et al. (2017) Assessment of vascular change using swept-source optical coherence tomography angiography: A new theory explains central visual loss in Behcet’s J Ophthalmol 2017: 2180723.
- Wintergerst MWM, Pfau M, Müller PL, Berger M, de Sisternes L, et al. (2018) Optical coherence tomography angiography in intermediate uveAm J Ophthalmol 194: 35-45.
- Tian M, Tappeiner C, Zinkernagel MS, Huf W, Wolf S, et al. (2019) Evaluation of vascular changes in intermediate uveitis and retinal vasculitis using swept-source wide-field optical coherence tomography angiography. Br J Ophthalmol 103: 1289-1295.
Citation: Ahmed MAA, Abdelhalim AS (2021) OCTA Quantitative Macular Micro-vascular Changes in Series of Uveitic Patients J Ophthal Opto 3: 012.
Copyright: © 2021 Ahmed MAA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.