*Corresponding Author:
Thana Y Aljaraedah,
Faculty of Agriculture Department of Nutrition and Food Technology Amman, Jordan
Tel: +962 (7)76680817
E-mail: dejeniebiot2006@gmail.com
Abstract
Malnutrition is a popular disorder in patients in the hospitals that is predominately underdiagnosed and undertreated. Unluckily, hospitals are recognized as a contribution to further declines in nutritional status. The prevalence of malnutrition in the older inpatients is 42.0% and 14.5% in younger inpatients and in pediatric inpatients ranging from 2.5 to 51%. Malnutrition induced by hospitals has multifactorial causes and is related to undesirable clinical and fiscal outcomes. Indeed, an increase in the global prevalence of obesity among inpatients has been reported in many surveys. There are nowadays increasing proof from clinical trials aimed at the effectiveness and implementation of nutritional support at the clinical inpatient population. Meanwhile a lot of clinical inpatients at nutritional risk or malnourished, had been suffered from multiple morbidities, this make the supply of dietary entry a challenging mission, given that maximum of the medical nutrition strategies and approaches are committed to particular diseases. In this review we showed the major malnutrition assessment tools that are used among hospitalized patients to assess the degree of malnutrition and the importance of several approaches to individualized enteral nutrition during critical illness have been discussed.
Keywords
Hospitalized patients; Malnutrition; Nutritional assessment of malnutrition in inpatients; Specialized nutrition support
Introduction
Malnutrition is a common cause and outcomes of illness [1], Diseases that related to malnutrition are a prevailing condition that is able to be linked to multi morbidity [2], diseases related to malnutrition are a predominant disorder among the elderly as well as in patients in everywhere worldwide [3], disease-related malnutrition is linked together with the occurrence of chronic morbidity, greater hospital admittance and readmission rates, amplified requirements for societal resources like home nursing services and even a high death rate [4]. Recognizing patients who are malnourished and including this greatly prevalent diagnosis in medical documents, permits malnutrition coding and resulting raise in hospital costs [5].
The prevalence of malnutrition in the older inpatients is 42.0% and 14.5% in younger inpatients [6] and in pediatric inpatients ranging from 2.5 to 51% [7].
Malnutrition classified as an independent factor related to negative clinical outcomes in patients who suffered from cancer [8]. De Pinho et al. [9] they found about one-fourth of all Brazilian participants who suffered from cancer were aged ≥ 65 years. In this life stage the frequency of moderate or supposed and severe malnutrition was nearly half of inpatients, and through the of nutrition impact symptoms they were with a higher possibility of occurrence of appetite absence. It was about forty five percent of those who are aged between 51 and 64 years, and it was around thirty six percent of those were aged lower than or equal fifty years [7].
The first and chief step is nutritional screening. Nutritional screening is accomplished to immediately recognize the nutritional status of the patients on admission. The second step following nutritional screening is a nutritional assessment [10]. Nutritional Assessment is accomplished to determine clinically/disease-related malnutrition and provide nutritional advice or support based on the findings and continuously monitor the clinical outcome. Malnutrition is high during hospitalization due to the treatment, surgeries and other procedures where patients might have to follow a very restricted diet or at times not eat [10]. Illnesses and procedures can affect appetite and patients may eat less because they don’t like their food choices or they are worried or depressed [10]. Malnutrition during hospitalization weakens the immune system and leaves patients vulnerable to infection, slower recovery and delayed wound healing, frequent hospital readmissions etc [10]. The most common vulnerable group of patients for malnourishment during hospitalizations are pediatrics (children), pregnant women and geriatrics (elderly). Malnourishment also prevails in the adult group with reference to specific disease conditions which affect their food intake. Nutritional care is, therefore, an important as well as an integral part of patient care in hospitalized patients [10].
Malnutrition induced by hospital’s affected on pediatric inpatients by undesirably affect medical outcomes, such as disturbances in immune response, thus causing children to have piteous wound healing with higher risk of infections and complications of their underlying disease, malnutrition may, on long-term, impact the growth and cognitive development trajectory [7]. Moreover, these adverse effects lead to delayed recovery and extend hospitalization, by this means increasing the financial burden on the health care system (in-patient day costs, treatments) and limiting hospital bed availability [7]. In contrast to adults, kids are particularly vulnerable to malnutrition, having a lower caloric reserve and higher nutritional supplies per unit of body weight, to account for growth. It follows that early identification of malnourished children or children who are possibly at risk for malnutrition is key to preventing weakening sequels. Most of methods were used to describe the malnutrition in children based on anthropometric parameters, old methods like weight-for-height percentile, heightfor-age percentile were used, and anthropometric measurements be expressed as z-scores [7]. screening tools had been used to detect and assess the malnutrition in hospitalized patients were seven tools ion screening tools for hospitalize, screening tool for risk on nutritional status and growth, pediatric yorkhill malnutrition screening, the pediatric digital scaled malnutrition risk screening tool, pediatric nutrition screening tool, and the pediatric malnutrition screening tool. Conversely, not yet completely validated, and no universal nutritional assessment tool that used to determine the early signs of nutritional status alteration and to classify children rendering to their risk of developing nutritional and medical complications through stay in hospitals [7].
In spite of the proof on the prevalence of malnutrition, it is predominatingly under-recognized and uncured. Thus, it is important validated nutritional screening and assessment tools were applied for early identification of nutritional problems during the length of hospital stay. While many nutrition screening and assessment tools are available, there is no universally accepted method for defining malnutrition risk and nutritional status [8]. CINAHL, Cochrane, Science Direct, Google Scholar, PubMed, and Scopus databases were searched starting date of inception in 1950 to the end of March 2020. Malnutrition can happen to anyone irrespective of gender, socio-economic status, affordability. Malnutrition in hospitals remains a common problem affecting patients of all ages. Consequences of malnutrition are very serious during hospitalization because, without proper nutrition, patients cannot stay healthy to deal with an illness that they already have [11,12]. There is no universal nutritional assessment tool used in studies to detect the malnutrition induced by hospitals, and the lack of consistency in the type of measures and their cut-off values prevents estimating the true prevalence of malnutrition the nutritional assessment of hospitalized patients is complex. Therefore, in this review we made comparisons between malnutrition screening and assessment approaches and tools were used in assessing the malnutrition in hospitalized patients through life stages, and to overview the importance of specialized nutrition support.
The Definition of Hospital-Induced Malnutrition and Outcomes Resulted
The characterization of malnutrition stays a query of debate, generally, unintentional weight loss more than five percent in a tiny time frame and reduced dietary intake are related to a worsening in dietary status [13]. “Hidden hunger” micronutrients the alternative name of Malnutrition or under nutrition [13]. Thus, no golden standard for characterizations of malnutrition, while the mutual international agreement is that malnutrition is an inadequate nutritional status concomitant with unfavorable clinical consequences [11]. Also, it’s explained by the European Society for Clinical Nutrition and Metabolism (ESPEN) as a condition causing by lack of intake or uptake of nutrition that leads to change body composition, decreases in fat free mass and body cell mass leading someone to reduce physical, mental function and impaired clinical outcome resulted from disease [14].
Regrettably, hospitals are recognized as a contribution to additional declines in nutritional status [15], Malnutrition is able to affect response to medication and surgical therapy and complications and reduction in survival [16]. Diseases are related to malnutrition in hospitalized sufferers is a major public health problem in mutually industrialized and rising countries around the worldwide [15]. Poor nutritional status is related to accelerated morbidity and mortality, enlarged time of stay in hospital, extra frequent re-admission, and elevated health care costs [17], Malnutrition in the health facility, putting can develop as an outcomes of insufficient nutrient intake, reduced in absorption of nutrients because of infection or trauma, or increased metabolic stresses during diseases [18]. Malnutrition considered as a costly problem in many countries, Curtis et al. [19] reported that over forty percent of patients were established to be malnourished (33% moderate and 0.1 severe). Malnourished inpatients had lengthier hospital stays and as a result cost other than well-nourished inpatients [19].
The Prevalence of Diseases Caused by Malnutrition
The prevalence of diseases associated with malnutrition had been informed to be between twenty percent and fifty percent, while data fluctuate noticeably because of differences in having a look at populations, ascertainment methods, and clinic setting [20]. The prevalent frame of epidemiological evidence comes from Europe, where several enormous studies have mentioned prevalence figures within the range of twenty to thirty percent [7], with a larger prevalence pragmatic within the older adults (32%-58%) [21], and who sufferers with malignant disease (31%-39%) [22] Studies performed in Asia have stated prevalence records between twenty seven percent to and thirty nine [23], through a greater prevalence in older adults were eighty eight percent [24] the critically ill (87%) [25], surgical patients (56%) [26], then patients with gastrointestinal malignancies forty eight percent [27]. Prevalence statistics from studies conducted in North America and Australia variety from thirty seven percent to forty five percent [28] and 23%-42% [29], respectively.
Specialized Nutrition support for Adult Patients and Malnutrition Induced by Hospitals
Estimations suggested about one third of all adult inpatients were malnourished, the outcomes of this on patient health and services are well acknowledged [30]. Bell et al. [28] examined the continuing implementation and evaluation of interdisciplinary or delegated malnutrition care processes of SIMPLE approach outlined in Figure 1 that is predictable to facilitate supply of great-value malnutrition care in Queensland public hospitals, and studied the need for development using the they reported the care processes focused towards highly individualized, dietitian supplied care, and they didn’t testing implementation if this interdisciplinary approach recovers malnutrition induced by hospitals [31].
Leandro-Merhi et al. [29] they reported prevalence of malnutrition by dissimilar nutritional indicators and identified factors that related to malnutrition in hospitalized patients, they examined anthropometric, laboratory standards, Subjective Global Assessment (SGA), Mini Nutritional Assessment (MNA), Nutritional Risk Screening (NRS), and Habitual Energy Consumption (HEC). Leandro-Merhi et al. [29] they found NRS remained more sensitive than else tools in the identification of malnutrition. Older patients who were at risk and had lower HEC values, calf circumference, body mass index and lymphocyte count. They considered the low lymphocyte count as a factor related to nutritional risk by the NRS. Twenty one percent of malnourished inpatients were established by the SGA; about thirty five percent of inpatients have a nutritional risk affording to NRS and a twelve percent has a low body mass index [32].
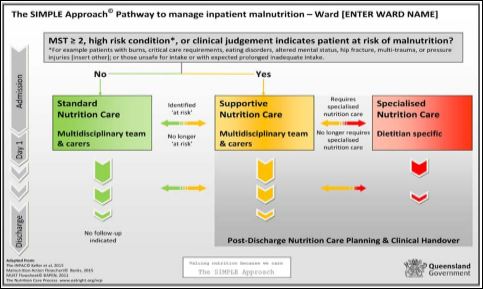
Figure 1: The SIMPLE approach pathway.
Specialized Nutrition for Inpatients Children and Malnutrition Induced by Hospitals
The American Society for Parenteral and Enteral Nutrition and the Society of Critical Care Medicine reviewed cautiously studies to assess the finest performs in nutritional support in critically ill child, they found there is a necessity for improved attention on accurate estimation of energy requirements and consideration about adjusting protein intake, immunonutrition cannot be currently recommended [33]. Generally, the critically ill child care is varied, and a nuanced method to specializing nutritional therapy with the purpose of improving clinical consequences is essential and several approaches to individualized enteral nutrition during critical illness have appeared [33].
The malnutrition among children frequently worsens due to the lengthy time stay in hospital. With a view to avoid acute hospital-acquired malnutrition and its consequences, the risk of nutritional diminution status requires to be identified at the time of admittance so that suitable nutritional intervention can be initiated at an early phase. Javed et al. [31] they measured the rate of recurrence of malnutrition amongst inpatient child with NRS more than four at presentation, they found the occurrence of malnutrition is quite high sixty five percent of hospitalized children with NRS more than four at admission have frequent malnutrition during hospitals stay. The sources of this malnutrition require to be addressed, and guiding principle may be modified to control and reduces malnutrition induced by hospitals [33].
Specialized Nutrition for Elderly Patients and Mal- nutrition Induced by Hospitals
Inflammation is a key motive force of malnutrition at some stage in diseases, and is regularly followed by metabolic changing, containing insulin resistance and absence of appetite [33]. Merker et al.[32] they examined whether sufferers’ baseline inflammatory popularity is associated with the result of nutritional support on thirty day mortality. Nevertheless, it quiet remains uncertain if inflammation impacts the response to nutritional assist amongst sufferers with disease-related malnutrition.
Multicenter prospective observational cohort study conducted by Ruiz et al. [33] covered eight hundred inpatients at four Colombian hospitals who have a diagnosis of congestive heart failure, community-acquired pneumonia, acute myocardial infarction, or chronic obstructive pulmonary disease. All inpatients were diagnosed for malnutrition by the Malnutrition Screening Tool (MST). Ruiz et al. [33] they determined, verified an excessive affiiction of malnutrition while of sanatorium admission, which undesirably impacted length of stay and mortality and extended the charges of hospitalization. These outcomes highlight the necessity for stepped forward prognosis and remedy of malnutrition induced by hospitals to enhance affected person outcomes and shrink health care costs.
Burgos et al. [2], they had been to determine the prevalence of diseases are related to malnutrition in a cohort study of a chronic patients with complex requirements admitted to 2 hospitals, and to estimate the influence of malnutrition of their hospitalization outcomes. Nutritional risk changed into estimated with MNA Tool and NRS2002. Hospitalization consequence records were assessed, counting the time of the sanatorium stay, mortality at some point on admission and placement when left the hospitals. +Afterward 5 months, a novel assessment turned into performed to evaluate death and readmissions. The prevalence of mutually malnutrition and its risk is very high in hospital admitted chronic patients with complex needs, and has a thoughtful effect on the placement at left hospitals and death rate. This high prevalence is not clarified with the aid of the multi-morbidity design. Also, other factors necessitate to be evaluated in this group of high requirements, high-cost patients [2] (Table 1).
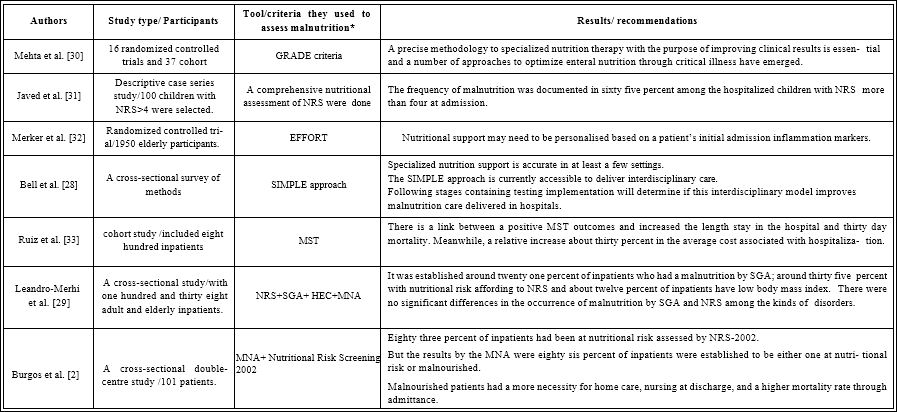
Table 1: Studies Reporting the Tools They Used in the Assessment of Malnutrition in Hospitalized Patients.
*GRADE: Grading of Recommendations, Assessment, Development, and Evaluation
NRS: Nutritional Risk Screening Tool.
EFFORT: Effect of Early Nutritional Support on Frailty, Functional Outcomes, and Recovery of Malnourished Medical Inpatients Trial.
SIMPLE: Systematized, Interdisciplinary Malnutrition Pathway for Implementation and Evaluation.
MST: Malnutrition Screening Tool.
SGA: Subjective Global Assessment.
HEC: Habitual Energy Consumption.
MNA: Mini Nutritional Assessment.
NRS-2002: Nutritional Risk Screening 2002.
Conclusion
Malnutrition is a common cause and outcomes of illness, no golden standard were detected for defined the malnutrition, deprived nutritional status is related to accelerated morbidity and mortality, increased time of stay in hospital, extra frequent re-admission, and elevated health care costs the classification of malnutrition stays a query of discussion. In the summary of studies examined the effect of malnutrition in hospitalized patients and the criteria used to assess malnutrition. Unfortunately, hospitals are documented as a contribution to further declines in nutritional status, and there is no specific nutritional assessment tools and approaches used to cover specialized nutritional adequacy.
References
- Ellis E (2019) The Causes of Geriatric Malnutrition: A Gerontological Nursing Honors Project. The Midwest Quarterly 60: 351-359.
- Burgos R, Joaquín C, Blay C, Vaqué C (2019) Disease-related malnutrition in hospitalized chronic patients with complex needs. Clinical Nutrition 5614: 30261-30264.
- Munoz Díaz B, Molina-Recio G, Romero-Saldaña M, Redondo Sánchez J, Aguado Taberné C, et al. (2019) Validation (in Spanish) of the Mini Nutritional Assessment survey to assess the nutritional status of patients over 65 years of age. Family practice 36: 172-178.
- Alvarez Hernández J, Planas Vilá M, León Sanz M, Garcia de Lorenzo y, Mateos A, et (2012) Prevalence and costs of multinutrution in hospitalized patients; The PREDyCES study. Nutr Hosp 27: 1049-1059.
- Fernandes A, Pessoa A, Vigário M, Jager-Wittenaar H, Pinho J (2020) Does malnutrition influence hospital reimbursement? A call for malnutrition diagnosis and coding. Nutrition 74: 38.
- Huang C, Lue K, Hsieh T, Liu S, Wang T, et al. (2020) Association between Sarcopenia and Clinical Outcomes in Patients with Esophageal Cancer under Neoadjuvant Therapy. Anticancer Research 40: 1175-1181.
- De Pinho N, Martucci R, Rodrigues V, D’Almeida C, Thuler L, et (2020) High prevalence of malnutrition and nutrition impact symptoms in older patients with cancer: Results of a Brazilian multicenter study. Cancer 126: 156-164.
- Lim Y (2010) Malnutrition and clinical outcomes in elderly patients from a Singapore acute hospital. QUT 1-6.
- Cederholm T, Bosaeus I, Barazzoni R, Bauer J, Van Gossum A, et (2015) Diagnostic criteria for malnutrition–an ESPEN consensus statement. Clinical nutrition 34: 335-340.
- Cederholm T, Barazzoni R, Austin P, Ballmer P, Biolo G, et al. ( 2017) ESPEN guidelines on definitions and terminology of clinical Clinical nutrition 36: 49-64.
- Corish C, Bardon L (2019) Malnutrition in older adults: Screening and Proceedings of the Nutrition Society 78: 372-379.
- Correia M, Hegazi R, Higashiguchi T, Michel J, Reddy B, et al. (2014) Evidence-based recommendations for addressing malnutrition in health care: An updated strategy from the feedM. E. Global Study Journal of the American Medical Directors Association 15: 544-550.
- Dorner T, Luger E, Tschinderle J, Stein K, Haider S, et al. (2014) Association between nutritional status (MNA®-SF) and frailty (SHARE-FI) in acute hospitalised elderly patients. The Journal of Nutrition, Health & Aging 18: 264-269.
- Ljungqvist O, Van Gossum A, Sanz ML, De Man F (2010) The Euro-pean fight against malnutrition. Clinical Nutrition 29: 149-150.
- Soeters P, Reijven P, Allison S, Konig W (2011) Diagnosis of malnutrition-Screening and assessment. In Basics in clinical Nutrition 3: 21-32.
- Curtis L, Bernier P, Jeejeebhoy K, Allard J, Duerksen D, et (2017) Costs of hospital malnutrition. Clinical Nutrition 36: 1391-1396.
- Norman K, Pichard C, Lochs H, Pirlich M (2008) Prognostic impact of disease-related malnutrition. Clinical Nutrition 27: 5-15.
- Vanderwee K, Clays E, Bocquaert I, Gobert M, Folens B, et al. (2010) Malnutrition and associated factors in elderly hospital patients: A Belgian cross-sectional, multi-centre study. Clinical Nutrition 29: 469-476.
- Planas M, Álvarez-Hernández J, León-Sanz M, Celaya-Pérez S, Araujo K, et (2016) Prevalence of hospital malnutrition in cancer patients: a sub-analysis of the PREDyCES® study. Supportive Care in Cancer 24: 429-435.
- Volpato S, Custureri R, Puntoni M, Bianchi L, Daragjati J, et al. (2018) Effects of oral amino acid supplementation on Multidimensional Prognostic Index in hospitalized older patients: A multicenter randomized, double-blind, placebo-controlled pilot study. Clinical Interventions in Aging 13: 633-640.
- Wakabayashi H, Sashika H (2014) Malnutrition is associated with poor rehabilitation outcome in elderly inpatients with hospital-associated deconditioning: A prospective cohort Journal of Rehabilitation Medicine 46: 277-282.
- Lee S, Choi M, Kim Y, Lee J, Shin C (2003) Nosocomial infection of malnourished patients in an intensive care unit. Yonsei Medical Journal 44: 203-209.
- Pham N, Cox-Reijven P, Greve J, Soeters P (2006) Application of subjective global assessment as a screening tool for malnutrition in surgical patients in Vietnam. Clinical Nutrition 25: 102-108.
- Wu B, Yin T, Cao W, Gu Z, Wang X, et (2009) Clinical application of subjective global assessment in Chinese patients with gastrointestinal cancer. World Journal of Gastroenterology: WJG 15: 3542- 3549.
- Rahman A, Wu T, Bricknell R, Muqtadir Z, Armstrong D (2015) Malnutrition matters in Canadian hospitalized patients: Malnutrition risk in hospitalized patients in a tertiary care center using the malnutrition universal screening tool. Nutrition in Clinical Practice 201530: 709-713.
- Valente K, Barreto M, Silva N, Guandalini V (2016) Use of the thickness of the adductor pollicis muscle in the identification nutritional status in different clinical conditions. Journal of Advanced Nutrition and Human Metabolism 2: 1487.
- Agarwal E, Ferguson M, Banks M, Bauer J, Capra S, et al. (2012) Nutritional status and dietary intake of acute care patients: Results from the Nutrition Care Day Survey 2010. Clinical nutrition 31: 41-
- Bell J, Young A, Hill J, Banks M, Comans T, et (2018) Rationale and developmental methodology for the SIMPLE approach: A Systematised, Interdisciplinary Malnutrition Pathway for impLementation and Evaluation in hospitals. Nutrition & dietetics 75: 226-234.
- Leandro-Merhi VA, Costa CL, Saragiotto L, Aquino JL (2019) Nutritional indicators of malnutrition in hospitalized Arquivos de Gastroenterologia 56: 447-450.
- Mehta N, Skillman H, Irving S, Coss-Bu J, Vermilyea S, et (2017) Guidelines for the provision and assessment of nutrition support therapy in the pediatric critically ill patient: Society of Critical Care Medicine and American Society for Parenteral and Enteral Nutrition. Journal of Parenteral and Enteral Nutrition 41: 706-742.
- Javed I, Mehmood M, Khalid J, Shamim S, Iqbal S, et al. (2019) Malnutrition; Malnutrition among Hospitalized Children in Tertiary Care Hospital. Professional Medical Journal 26: 653-657.
- Merker M, Felder M, Gueissaz L, Bolliger R, Tribolet P, et (2020) Association of Baseline Inflammation with Effectiveness of Nutritional Support among Patients with Disease-Related Malnutrition: A Secondary Analysis of a Randomized Clinical Trial. JAMA Network Open 3: 200663.
- Ruiz A, Buitrago G, Rodríguez N, Gómez G, Sulo S, et al. (2019) Clinical and economic outcomes associated with malnutrition in hospitalized patients. Clinical Nutrition 38: 1310-1316.
Citation: Aljaraedah TY (2020) Nutritional Assessment of Hospital-induced Malnutrition in All Hospitalized Patient: A Critical Review. J Nutr Food Sci 3: 014.
Copyright: © 2020 Aljaraedah TY. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and re- production in any medium, provided the original author and source are credited.