*Corresponding Author:
Huma Liaqat,
Department of Biochemistry,Institute of Molecular Biology and Biotechnology, University of Lahore, Lahore, Pakistan
E-mail: humma2408@gmail.com
Abstract
Neuroblastoma (NB) is the most much of the time happening extracranial childhood tumor. It is named an embryonal neuroendocrine tumor, starting from neural peak forebear cells. Subsequently, it can happen anyplace along the sympathetic sensory system, including the predominant cervical, para-spinal, and celiac ganglia; the larger part emerge in the adrenal organs. Neuroblastoma is a malignancy that creates from juvenile nerve cells found in a few zones of the body. Neuroblastoma most generally emerges in and around the adrenal organs, which have comparative starting points to nerve cells and sit on the kidneys. Be that as it may, neuroblastoma can likewise create in different territories of the stomach area and in the chest, neck and close to the spine, where gatherings of nerve cells exist. Neuroblastoma most generally influences children age 5 or more youthful, however it might once in a while happen in more established kids. A few types of neuroblastoma leave individually, while others may require numerous medicines.
Keywords
Embryonal tumor; Immunotherapy; Neuroblastoma
Introduction
Neuroblastoma fundamentally influences more youthful kids and is the most as often as possible happening strong tumor in babies younger than one year representing around a fifth (22%) of all malignancies analyzed at this age. The rate of neuroblastoma is uncommon after the age of five. Just 2% of neuroblastoma is analyzed in kids over the time of 10 years and 0.5% in those beyond 15 years old years. Neuroblastoma is uncommon in adolescents, youthful grown- ups and grown-ups and current treatment is extensively equivalent to in more youthful kids, however may change later on. In these patient gatherings the infection is generally increasingly moderate developing [1]. When all is said in done, the viewpoint isn’t in the same class as in more youthful patients, yet the ailment can regularly be controlled for a long time because of its moderate development. Neuroblastoma is an ‘embryonal tumor’, a kind of malignancy that creates from the cells abandoned from a child’s advancement in the belly. The phones that it creates from are called neuroblasts, offering ascend to the name neuroblastoma: ‘neuro’ means nerve ‘blast’ means cells in an early stage of development and ‘oma’ means a group of cells, or a tumour.
Neuroblastoma can happenany place in the body. The site of inception is either in one of the two adrenal organs arranged in the mid-region (belly) or in nerve tissue that keeps running close by the spinal string in the neck, chest, mid-region or pelvis. The most widely recognized site for the tumor to develop is in the mid-region (belly). A few tumors develop at the back of the chest and incidentally significantly higher up towards the neck [2]. About half of tumors begin in the adrenal organs. The adrenal organs are specific organs found above the kidneys. They typically discharge hormones to keep up pulse, and empower us to react to pressure. In a few cases, neuroblastoma can spread to tissues past the first site, for example, the bone marrow, bone, lymph hubs, liver and skin.
Epidemiology
Neuroblastoma is the most well-known extracranial strong tumor in adolescence. Its yearly frequency is roughly 9 for each million kids with roughly 150 new cases analyzed yearly in France and 650 new cases in the United States. NB is the main strong tumor of adolescence for which there have been expansive screening activities, spearheaded to a great extent in Japan. All-inclusive screening of half year old asymptomatic babies by identification of raised urinary catecholamines brought about a 2-crease increment in NB occurrence to 20.1 per million kids; notwithstanding, the greater part of the recognized tumors had positive clinical and organic attributes [3]. Concentrates in Germany furthermore, Quebec additionally showed an expanded frequency and identification of tumors with good science and pathology. When all is said in done, widespread screening has not recognized poor anticipation malady, which as a rule presents at a more established age and, consequently, has not influenced death rates. Interestingly, in chose populaces with an acquired hereditary inclination to NB, screening might be shown.
Signs and Symptoms
The symptoms of neuroblastoma may change contingent upon where the kid’s tumor is.
- If the tumor is in the stomach area, belly might be swollen and may gripe of blockage or experience issues passing pee.
- If the tumor influences the chest region, child may be winded and experience issues gulping.
- If the tumor happens in the neck, usually unmistakable as a protuberance and infrequently influences breathing and gulping. A tumor in the neck may cause extraordinary understudy estimate, diminished perspiring, redness or a ‘saggy’ eyelid on one side of the face (Horner’s disorder).
- Occasionally, there are stores of neuroblastoma in the skin that show up as little, blue-hued irregularities.
- If the tumor is pushing on the spinal line, youngsters may have shortcoming in the legs and walk On the off chance that child isn’t yet strolling, you may see diminished leg developments. They may likewise have stoppage or trouble passing pee. There may likewise be related back agony.
- Children might be found to have high blood
- Very once in a while, children may have jerky eye and muscle developments (opsoclonus-myoclonus-ataxia disorder, or ‘moving eyes disorder’), and general instability related with the neuroblastoma [4].
There are frequently dubious and non-explicit related symptoms of tiredness, pale composition, loss of hunger, weight reduction, bone torment and summed up inconvenience which can make a kid rather peevish and miserable. Numerous children with neuroblastoma have little in the manner of manifestations. Maybe they have appeared ‘rotten’ for a brief period or have had lost craving, unclear a throbbing painfulness or perspiring. Except if a parent or specialist feels a knot, while washing, dressing or looking at the child, a finding of neuroblastoma may not be at first considered [5]. It is conceivable that a large number of the indications your kids given are like those of increasingly normal, less genuine youth sicknesses. Numerous guardians wonder in the event that they or on the other hand a specialist ought to have seen something sooner, however since this is such an uncommon ailment, the determination is once in a while suspected if just genuinely dubious side effects are available. Neuroblastoma, especially ‘high hazard’ neuroblastoma, frequently displays at a late stage.
Tests for diagnosis

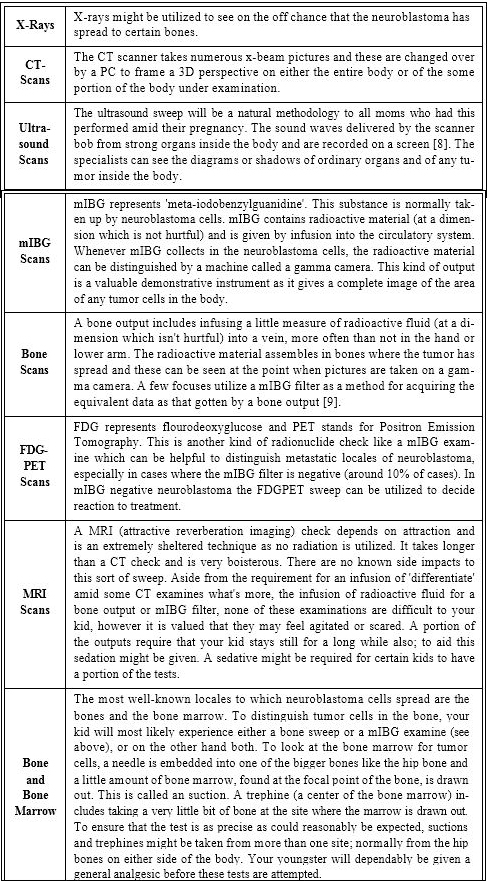
Scans for diagnosis
Stages of tumor
Stage 1: Neuroblastoma (INRSS stage L1)
This implies the tumor is genuinely little and kept to one site. It has not spread anyplace else in the body and can be evacuated totally by a task. This kind of tumor is generally reparable by medical procedure alone.
Stage 2: Neuroblastoma (INRSS stage L1)
Similarly as with stage 1, the tumor is restricted to one site and has not spread to far off pieces of the body. Notwithstanding it might be bigger than a phase 1 neuroblastoma and, at activity, it might be progressively hard to expel totally. Some of the time a lymph hub or a few organs close to stage 2 neuroblastoma may likewise have been influenced by the tumor. Stage 2 is normally treated by medical procedure alone be that as it may, contingent upon the site and aftereffects of specific tests, extra treatment, for example, chemotherapy might be required [10].
Stage 3: Neuroblastoma (INRSS stage L2)
This phase of tumor is likewise limited to the essential site in that it has not spread to different pieces of the body. The tumor might be extremely vast and said to have crossed the ‘mid-line’ of the body. This implies the tumor has developed appropriate over the kid’s belly or chest from the first side where it started. This kind of tumor would ordinarily be hard to securely expel precisely. Chemotherapy will be at first prescribed to attempt to contract the tumor for resulting safe careful evacuation. After the activity, radiotherapy might be given.
Stage 4: Neuroblastoma (INRSS Stage M)
This implies the essential tumor might be of any size, in any case, some neuroblastoma cells have split away and spread to different organs of the body, generally usually bones, bone marrow or liver. Chemotherapy will be prescribed for a phase 4 neuroblastoma to execute the tumor cells that have spread to various body parts what’s more, to shrivel the essential tumor for later evacuation by an task. After medical procedure, further chemotherapy is given, utilizing large portions. After this ‘high portion chemotherapy’, the following piece of the treatment may include radiotherapy [11]. In the event that your kid is enlisted on a clinical preliminary, this might be trailed by immunotherapy which plans to support the youngster’s own safe framework to help execute any remaining tumor cells.
Immunotherapy is given nearby a treatment which makes neuroblastoma cells develop into typical nerve cells called 13 cis retinoic corrosive. Most newborn children who present with stage 4 neuroblastoma who are analyzed when they are under one year of age normally have less ‘forceful’ neuroblastoma than that happening in more established kids. In this manner, they may get a less serious course of chemotherapy than the treatment lay out above.
Stage 4s: Neuroblastoma (INRSS stage MS)
This is a unique kind of neuroblastoma found in very youthful children, under one year old. The tumor cells may have spread past the ‘essential’ site to different pieces of the body, yet the cells generally act in a less forceful style than in a more seasoned kid. The locales of the body influenced by stage 4s neuroblastoma notwithstanding a little essential tumor which is frequently in one of the adrenal organs are most commonly the liver, skin and here and there the bone marrow [11]. At the point when this example of malady is noted the oncologist may feel genuinely certain that the kid will show signs of improvement with no, or practically nothing, treatment as the tumors can recoil and vanish unexpectedly without any treatment. At times if the tumor is causing clinical issues or if there are sure hereditary changes in the tumor cells low dosages of chemotherapy will be given to urge the tumor to begin contracting.
Treatments
There are four primary sorts of treatment that are utilized in the treatment of neuroblastoma: surgery, radiotherapy, chemotherapy and immunotherapy.
Surgery: This is a task to evacuate the tumor on the off chance that it is conceivable. Medical procedure might be included at a later phase of treatment, regularly after a few courses of chemotherapy have been given to recoil the tumor with the goal that it very well may be all the more effectively furthermore, in this way more securely expelled by the specialist [12,13].
Surgical Complications
Radiotherapy: This is treatment with high vitality x-beams to attempt and slaughter the tumor cells. A treatment machine called a straight quickening agent focuses on the x-beams at the tumor from outside the body (Figure 1).


Figure 1: Therapy (IMRT plan) for a solitary but extensive skull metas- tasis. The percentage of the prescription radiation dose is represented by the colored “isodose”lines. This technique maximizes sparing of adjacent critical structures.
Chemotherapy: This is the primary treatment for medium and high hazard neuroblastoma. Chemotherapy is the utilization of medications, generally given through a dribble into a vein (intravenously), to decimate disease cells. When the analysis of neuroblastoma is affirmed, the site, organize and once in a while the outcomes from exceptional hereditary tests on the tumor will help the oncologist responsible for your youngster’s treatment to settle on the best treatment routine, which is frequently called the convention [15,16]. The recommended treatment will be examined completely with you. Further on in this booklet you can discover a depiction of how the drugs picked for your kid will be conveyed and an clarification of the potential reactions related with chemotherapy. For medium and high hazard neuroblastoma, the general example of treatment in most European focuses is to give chemotherapy to pulverize neuroblastoma cells all through the body. After a time of chemotherapy, the position furthermore, site of the tumor and any metastases will be reassessed cautiously by bone marrow examinations, a CT or on the other hand MRI examine, mIBG sweep and bone output [17]. Careful expulsion of the essential tumor will at that point be endeavored. In all respects sporadically, regardless of whether the fundamental tumor has contracted down great, it might be close to the fundamental blood vessels or a sensitive body organ that would make medical procedure entangled and hazardous. For this situation, it might be proposed that the specialist does not endeavor to evacuate the tumor.
Immunotherapy: Immunotherapy is another type of treatment for neuroblastoma which depends on cells of the body’s own resistant framework to slaughter disease cells. There are unique approaches to do this yet presently a counter acting agent treatment is most usually utilized. The counter acting agent acts against a sugar-fat particle present on almost all neuroblastoma cells called GD2 (disialoganglioside) [18]. At the point when the neutralizer ties to GD2 on the neuroblastoma cells, the cells kick the bucket in a unexpected route in comparison to after chemotherapy or radiotherapy. This distinctive way is called counter acting agent subordinate or supplement subordinate cytotoxicity.
There is proof that different cells in the insusceptible framework, for example, regular executioner cells and macrophages, may advance neuroblastoma cell passing. Medications can be given to build the quantity of these insusceptible framework cells, however these expanded numbers might be mindful for genuine reactions related with the counter acting agent treatment [19].
Possible side effects of treatments include:
- Temporary hair loss
- Nausea and Vomiting
- Weight loss
- Depression of blood and bone marrow
- Fertility
- Constipation or Diarrhoea
- Kidney damage
- Damage to hearing
- Sore mouth
- Veno-occlusive disease (VOD)
Conclusion
Neuroblastoma is very solid tumor in children with early developing stages of their brain. It can found in several areas of their body where there is immature nerve cells are present. Symptoms of neuroblastoma can be in abdomen and in chest as well. The tumor usually begins with a genetic mutation from a normal cell to the abnormal division of cells in its development process. The average survival rate for 5 years children with neuroblastoma is 81% while with no tumor the survival rate of 5 years old children is 95%. However, neuroblastoma can be cured in early stages. Many tests are available to diagnose neuroblastoma like blood, urine and genetic tests and also scanning processes that can diagnose neuroblastoma at early stage. There are 4 stages of neuroblastom. The stage known as 4s neuroblastoma (INRSS stage MS) is unique kind of tumor found in the children. There are four primary sorts of treatment that are utilized in the treatment of neuroblastoma known as surgery, radiotherapy, chemotherapy and immunotherapy. We must continue to refine our ability to better identify the rare symptoms that cannot be diagnosed easily but have apparent low-risk or intermediate-risk disease in a child. Advances in understanding the biology and genetics of neuroblastoma will be the key in the individual management of disease as well as in development of new drugs for the treatment in better ways.
References
- Geoerger B, Hero B, Harms D, Grebe J, Scheidhauer K, et al. (2001) Met- abolic activity and clinical features of primary ganglioneuromas. Cancer 91: 1905-1913.
- Woods WG, Gao RN, Shuster JJ, Robison LL, Bernstein M, et al. (2002) Screening of infants and mortality due to neuroblastoma. N Engl J Med 346: 1041-1046.
- Nickerson HJ, Matthay KK, Seeger RC, Brodeur GM, Shimada H, et al. (2000) Favorable biology and outcome of stage IV-S neuroblastoma with supportive care or minimal therapy: A Children’s Cancer Group study. J Cli- nOncol 18: 477-486.
- Mitchell WG, Gonzalez YD, Brumm VL, Aller SK, Burger E et al. (2002) Op- soclonus-ataxia caused by childhood neuroblastoma: Developmental and neurological sequelae. Pediatrics 109: 86-98.
- Matthay KK, Seeger RC, Reynolds CP, Stram DO, Leary MCO, et (1994) Allogeneic versus autologous purged bone marrow transplantation for neuro- blastoma: A report from the Children’s Cancer Group. J ClinOncol 12: 2382- 2389.
- Gaspar N, Hartmann O, Munzer C, Bergeron C, Millot F, et (2003) Neuro- blastoma in adolescents. Cancer 98: 349-355.
- Seeger RC, Reynolds CP, Gallego R, Stram DO, Gerbing RB, et al. (2000) Quantitative tumor cell content of bone marrow and blood as a predictor of outcome in stage IV neuroblastoma: A Children’s Cancer Group J Cli- nOncol 18: 4067-4076.
- Kushner BH, Kramer K, LaQuaglia MP, Modak S, Cheung N-KV (2003) Neu- roblastoma in adolescents and adults: The Memorial Sloan-Kettering experi- Med Pediatr Oncol 41: 508-515.
- Vassal G, Doz F, Frappaz D, Imadalou K, Sicard E, et al. (2003) A phase I study of irinotecan as a 3-week schedule in children with refractory or recur- rent solid tumors. J ClinOncol 21: 3844-3852.
- Kletzel M, Katzenstein H, Haut PR, Yu AL, Morgan E, et (2002) Treatment of high-risk neuroblastoma with triple-tandem high-dose therapy and stem- cell rescue: results of the Chicago Pilot II Study. J ClinOncol 20: 2284-2292.
- Miano M, Garavanta A, Pizzitola MR, Piccolo MS, Dallorso S, et al. (2001) Megatherapy combining I131 metaiodobenzylguanidine and high-dose che- motherapy with haematopoietic progenitor cell rescue for neuroblastoma Bone Marrow Transplant 27: 571-574.
- Pfluger T, Schmied C, Porn U, Leinsinger G, Vollmar C, et al. (2003) Inte- grated imaging using MRI and 123I metaiodobenzylguanidine scintigraphy to improve sensitivity and specificity in the diagnosis of pediatric AJR Am J Roentgenol 181: 1115-1124.
- Yeung HWD, Grewal RK, Gonen M, Schoder H, Larson SM (2003) Patterns of 18F-FDG uptake in adipose tissue and muscle: a potential source of false- positives for PET. J Nucl Med 44: 1789-1796.
- Schilling FH, Bihl H, Jacobsson H, Ambros PF, Martinsson T, et al. (2000) Combined (111) In-pentetreotide scintigraphy and 123I-mIBG scintigraphy in neuroblastoma provides prognostic information. Med PediatrOncol 35: 688- 691.
- Kushner BH, Yeh SDJ, Kramer K, Larson SM, Modak S, et (2003) Impact of MIBG scintigraphy on assessing response of high-risk neuroblastoma to dose-intensive induction chemotherapy. J ClinOncol 21: 1082-1086.
- George R, London WB, Maris JM, Cohn SL, Diller L, et al. (2003) Age as a continuous variable in predicting outcome for neuroblastoma patients with metastatic disease: Impact of tumor biological features [abstract]. Proc Am Soc Clin Oncol 22: 799.
- Shulkin BL, Shapiro B (1998) Current concepts on the diagnostic use of MIBG in children. J Nucl Med 39: 679-688.
- Ruffini V, Fisher GA, Shulkin BL, Sisson JC, Shapiro B (1996) Iodine-123- MIBG imaging of neuroblastoma: utility of SPECT and delayed imaging. J Nucl Med 37: 1464-1468.
- Biasotti S, Garavanta A, Villavecchia GP, Cabria M, Nantron M, et (2000) False-negative metaiodobenzylguanidine scintigraphy at diagnosis of neuro- blastoma. Med Pediatr Oncol 35: 153-155.
Citation: Liaqat H, Hassan Z (2020) Neuroblastoma-An Extracranial Childhood Tumor. J Cell Mol Onco 2: 004.
Copyright: © 2020 Liaqat H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.