*Corresponding Author:
Gunes Orman,
Department of Radiology, Texas Children’s Hospital, Texas, USA
Tel: +1 8328225317
Email: gxorman@texaschildrens.org
Abstract
Graves’ Disease (GD) is the most common cause of clinically significant hyperthyroidism during pregnancy. Neonatal hyperthyroidism results from transplacental passage of thyrotropin receptor antibodies from mother to fetus. But, this condition is very rare, only 1% of the babies born to mothers with GD will have neonatal GD. Neonatal clinical manifestations may be delayed or neonatal hyperthyroidism symptoms can be confused with sepsis or congenital viral infections. Therefore, timely diagnosis and treatment is important. We present a two day-old newborn girl with acute onset of generalized abnormal movements and a large neck mass. Color Doppler ultrasound showed diffuse enlargement and increased vascularity of the thyroid gland. Magnetic resonance imaging confirmed a massively enlarged thyroid gland encasing and mildly narrowing the trachea, as well as enlargement of the anterior pituitary gland. The constellation of findings was consistent with neonatal hyperthyroidism secondary to maternal GD.
Keywords
Fetal hyperthyroidism; Graves’ disease; Maternal hyperthyroidism; Neonatal goiter; Neonatal hyperthyroidism; Neonatal thyrotoxicosis
Introduction
Clinical hyperthyroidism affects 0.1-0.4% of the pregnancies [1]. Graves’ Disease (GD) is the most common cause of clinically significant hyperthyroidism during pregnancy. In pregnant women with GD, maternal Thyrotropin Receptor Antibodies (TRAb) can cross the placenta and induce fetal or neonatal thyrotoxicosis [2].
Neonatal hyperthyroidism is rare and typically caused by maternal GD, which results from transplacental passage of TRAb from mother to fetus in the setting of maternal GD between 17th and 20th gestational weeks [3]. This leads to activation of the Thyroid Stimulating Hormone Receptor (TSHR) and consequently increases thyroid hormone production [4]. Therefore, pregnant women with current or past history of hyperthyroidism require screening to determine if the fetus or neonate is at risk to develop hyperthyroidism. Measurement of maternal serum TRAb identifies pregnancies at risk for fetal and neonatal hyperthyroidism development [2,5]. Only 1% of these babies born to these mothers will have neonatal GD [6].
Neonatal clinical manifestations may be delayed by 7 to 17 days due to maternal antithyroid drug use. In addition, neonatal hyperthyroidism symptoms can be confused with sepsis or congenital viral infections [7]. Therefore, timely diagnosis and treatment is important. Diagnosis of hyperthyroidism is made by elevated fT4/ T3, and low TSH. Furthermore, Color Doppler Ultrasound (CDUS) is helpful by showing normal/enlarged thyroid size and diffuse hypervascularisation [6]. Our goal is to present a rare neonatal hyperthyroidism case secondary to maternal GD.
Case Report
A two day-old newborn girl was admitted to pediatric emergency department with acute onset of generalized abnormal movements and a large neck mass at physical examination. In addition, arterial hypertension and hypoglycemia was noted next to pansystolic cardiac murmur suggestive of mitral regurgitation. The mother was treated with Propylthiouracil (PTU) for GD during pregnancy. Endocrine work up of the neonate showed initially high level of TSH consistent with a normal neonatal surge, followed by progressive decrease of TSH and increase in free Thyroxine (fT4).
Imaging workup was performed initially by neck CDUS (Figure 1) which shows diffuse enlargement and increased vascularity of the thyroid gland. Echocardiogram confirmed mitral regurgitation and a patent ductus arteriosus with right-to-left shunt as well as flow reversal in the descending aorta during diastole. Magnetic Resonance Imaging (MRI) of the neck and brain (Figure 2) confirmed a massively enlarged thyroid gland encasing and mildly narrowing the trachea, as well as enlargement of the anterior pituitary gland. The constellation of findings was consistent with neonatal hyperthyroidism secondary to maternal GD. The patient was followed in endocrine clinic for a week without any treatment. She had some hypoglycemia during the initial hospitalization, which resolved by discharge. She was generally well at the last follow up visit after 7 weeks from initial presentation.
Physical exam was normal and showed no signs of thyromegaly.
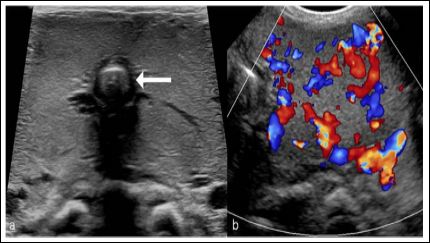
Figure 1: Neck Ultrasound (US) of the newborn patient. (a) Axial US image shows a diffusely enlarged hyperechoic thyroid gland encasing the trachea (arrow). (b) Color Doppler US shows a marked hyperperfusion of the enlarged thyroid gland.
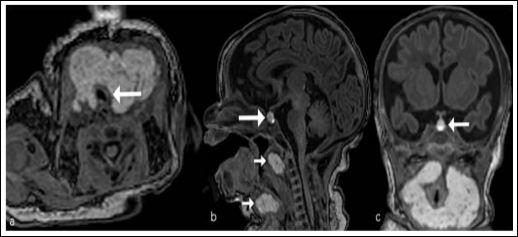
Figure 2: Magnetic resonance imaging (MRI) of the newborn patient. (a) Axial T1-weighted neck MRI shows a diffusely enlarged, lobulated T1-hyperintense thyroid gland with wrapping and mild compression of the trachea (arrow). (b, c) Sagittal and coronal T1-weighted brain MRI slices show a mildly T1-hyperintense hyperplasia of the anterior lobe of the pituitary gland (b, c, large arrow) as well as the enlarged thyroid (b, small arrows) encasing the airway. Note that, size and location of the T1-hyperintense posterior lobe of the pituitary gland are normal (b).
Discussion
Risk factors for neonatal thyrotoxicosis development mainly classified as: 1) Maternal risk factors: a) raised thyroid binding immunoglobulin levels in pregnancy; b) thyroid binding immunoglobulin level not assessed; c) clinical thyrotoxicosis in third trimester; d) thionamide required in third trimester; e) family history of TSH receptor mutation, 2) Neonatal risk factors: Evidence of fetal thyrotoxicosis [8].
Causes of neonatal goiter include neonatal GD, transplacental passage of goitrogens (methimazole, PTU, etc), and congenital hypothyroidism. Neonatal GD is a rare entity presenting in approximately 2% of children from mothers with GD. Only approximately 1% of childhood thyrotoxicoses occurs in the neonatal period [9]. Neonatal GD is an IgG antibody-like mediated autoimmune disease from antibody passage across the placenta during the third trimester of pregnancy.
Clinical findings may not be evident in the first few days of life that is before maternal anti-thyroid drugs have been cleared from the newborn circulation [9]. In addition to the classic clinical features of hyperthyroidism, newborns may display sign of intrauterine growth retardation, exaggerated Moro and other reflexes, microcephaly, craniosynostosis [7]. Congestive heart failure is another important concern in affected newborns [9]. Severe cases may result in hepatosplenomegaly, thrombocytopenia, jaundice, pulmonary hypertension or even death [3]. However, most cases are transient, depending on the level of antibodies present in serum and antithyroid drugs used, usually with spontaneous resolution within 3-16 weeks [7]. If a neonate presents at delivery with a goiter, fT4, Total Triiodothyronine (T3) and TSH should be measured at delivery, and at 3-5 and 10-14 days of life.
Diagnosis of GD is made by elevated fT4/T3, and low TSH. Elevation of fT4 during the first postnatal week predicts the development of neonatal hyperthyroidism [10]. Thyrotrophic anterior lobe pituitary gland hyperplasia (Figure 2) can be a secondary finding of primary hypothyroidism [11]. In neonates, as in the presented case, it may be a consequence of transplacental passage of PTU with resultant exaggerated TSH secretion.
References
- Kobaly K, Mandel SJ (2019) Hyperthyroidism and Endo- crinol Metab Clin North Am 48: 533-545.
- van Dijk MM, Smits IH, Fliers E, Bisschop PH (2018) maternal thy- rotropin receptor antibody concentration and the risk of fetal and neonatal thyrotoxicosis: A systematic Thyroid 28: 257-264.
- Samuels SL, Namoc SM, Bauer AJ (2018) Neonatal thyrotoxicosis. Clinics in Perinatology 45: 31-40.
- Joshi K, Zacharin M (2018) Hyperthyroidism in an infant of a mother with autoimmune hypothyroidism with Positive TSH Receptor Anti- J Pediatr Endocrinol Metab 31: 577-80.
- Cui Y, Rijhsinghani A (2019) Role of maternal thyroid-stimulating immunoglobulin in Graves’ Disease for predicting perinatal thyroid AJP Rep 9: 341-345.
- Clerc J (2014) Imaging the thyroid in children. Best Practice & Re- search Clinical Endocrinology & Metabolism 28: 203-220.
- Kurtoğlu S, Özdemir A (2017) Fetal neonatal hyperthyroidism: Di- agnostic and therapeutic Turk Pediatri Ars 52: 1-9.
- Ogilvy-Stuart A (2002) Neonatal thyroid disorders. Arch Dis Child Fetal Neonatal Ed 87: 165-171.
- Léger J (2017) Management of fetal and neonatal Graves’Horm Res Paediatr 87: 1-6.
- Besancon A, Beltrand J, Le Gac I, Luton D, Polak M (2014) Man- agement of neonates born to women with Graves’ Disease: A cohort Eur J Endocrinol 170: 855-862.
- Moumen A, Meftah A, El Jadi H, Elmoussaoui S, Belmejdoub G (2015) An unusual pituitary mass revealing a primary hypothyroid- ism! Clin Pract 5: 733.
Citation:Orman G, Beltran-Perez J, Huisman TAGM, Soares BP (2020) Neonatal Thy- rotoxicosis and Massive Goiter Secondary to Maternal Hyperthyroidism: Ultrasound and Magnetic Resonance Imaging Findings. J Case Repo Imag 4: 019.
Copyright: © 2020 Orman G, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.


