*Corresponding Author:
Ian Hewson,
Dental Services Alfred Hos- pital Melbourne Victoria, Australia
Tel: +61 0418103845
E-mail: ihewson@bigpond.net.au
Summary
Historically inherited bleeding disorder patients have had factor support for oral surgery procedures, this factor support is time consuming, expensive and has the potential to transmit blood borne diseases or for the patient to develop inhibitors to the factors. A protocol has been developed by the Alfred Hospital Dental Unit in consultation with the Ronald Sawers Haemophilia Centre where rigorous local measures of careful surgical technique, 5% tranexamic acid, placement of surgicel and careful suturing in conjunction with a course of oral tranexamic acid were used to obtain haemostasis post oral surgery with no or minimum factor support. Oral surgery can be safely performed using local measures on this population.
Keywords
Factor support; Haemophilia; Oral surgery; von Willi- brand’s disorder
Introduction
Haemophilia A and B are inherited sex linked defects, affecting 1 in 5000 male births, there are approximately 3,000 people living in Australia with varied degrees of severity of the disorder, Haemophilia can be mild, moderate or severe:
- Mild Haemophilia - 5-40% factor VIII or IX activity
- Moderate Haemophilia - 1-5% factor VIII or IX activity
- Severe Haemophilia - Less than 1% factor VIII or IX activity
80% of these individuals have haemophilia A (factor VIII defi- ciency) and 20% haemophilia B (factor IX deficiency), 30% of hae- mophilia A patients have a severe form of the disease [3] and 18% of haemophilia B patients have a severe form of the disease. 30% of the severe haemophilia A and 6% of the severe haemophilia B patients develop inhibitors [2,12].
Von Willibrand’s Disorder is an autosomal recessive disorder where the numbers of male patient’s equal female, about 200,000 peo- ple are affected in Australia (1% - 2% of population). Von Willebrand’s disease is due to a dysfunction or deficiency of the von Willebrand factor (vWF) a large multimeric glycoprotein essential in platelet ad- hesion, initially the vWF mediates the adhesion of platelets to sites of vascular injury and then binds and stabilizes the pro-coagulation factor VIII allow the formation of a clot.
There are three main types of von Willibrand’s disorder:
- Type 1: 60% - 80% of cases vWF 10%-45% of normal quantitative defect
- Type 2: 20%-30% of cases vWF level normal but qualitative defect
- Type 2 subtypes 2A, 2B, 2N, 2M
- Type 3: Most severe form with very low vWF and Factor VIII
Dental treatment and oral surgery have traditionally been asso- ciated with a high risk of bleeding in patients with inherited bleed- ing disorders. Published literature has identified use of clotting factor replacement therapy for inferior alveolar nerve blocks, periodontal procedures and all surgical procedures [1,11]. The need for dental extractions particularly has required a multidisciplinary approach and stringent protocols [2,4]. These protocols involve administrating exogenous clotting factors replacements with either plasma-derived or recombinant products, depending on the type and severity of the bleeding disorder [5]. Factor VIII for patients with haemophilia A and factor IX for haemophilia B has previously been given pre and post operatively with an aim of increasing the clotting factor levels to a concentration of 50-100 IU dL for a period of 5-7 days to reduce the risk of peri and postoperative bleeding [9]. Previously at the Alfred this necessitated the patients being admitted for a day prior to their surgery and up to five days post surgery to receive their factor support.
The main recognised issues with providing factor replacements for patients with bleeding disorders during oral surgery is the poten- tial development of inhibitors within these patients [5]. For therapeu- tic infusions, alloantibodies against the foreign factor VIII develop in approximately 30% of patients with severe haemophilia A and allo- antibodies against the foreign factor IX develop approximately 6% of patients with severe haemophilia B [5]. Viral transmission including hepatitis A and Hepatitis B traditionally has been a significant risk fac- tor in human-derived blood products, with many patients previously been infected with HIV and hepatitis C [7,8]. Furthermore, limiting the place of treatment to those who can provide factor support can create burden on the patient, in where if the factor replacement is un- available, the patient cannot receive care. The administration of factor replacement involves additional appointments, practitioner time, and is expensive to the treating facility.
Patients who develop inhibitors to factor FIII or IX replacement require any further factor support treatment with factor VII which is extremely expensive. The Alfred Dental Unit have in consultation with the Ronald Sawers Haemophilia Centre developed a protocol for the provision of a method of safe bleeding control post dental extraction in patients with bleeding disorders [6,13]. The protocol includes the use of systemic antifibrinolytic agents (oral tranexamic acid) and lo- cal haemostatic measures, involving suturing, the placement of 5% tranexamic acid solution into the surgical site, the use of haemostatic packing material and local tranexamic acid mouthwash [10].
Materials and Methods
250 consecutive patients of the Ronald Sawers Haemophilia Centre requiring oral surgery were recruited onto the study; all patients provided written consent for the procedures. Ethic approval was granted by The Alfred Ethics Committee. Patients who were on regular prophylactic factor cover continued with the same cover, severe patients who have on demand factor cover received a single dose of appropriate factor an hour pre-operative, no other pre-operative, peri-operative or post-operative clotting factors were given for any procedure irrelevant of the patient’s baseline factor levels or the degree of difficulty of the procedure except in the case of a post-operative bleed that required treatment with factors.
All patients were advised to take 1g tranexamic acid oral tablets TDS starting the day before, and continuing 7- 10 days post surgery. All surgical procedures were performed by or under the supervision of an experienced oral surgeon and carried out as atraumatically as possible with careful removal of teeth. Where mucoperiosteal flaps were raised, incisions were placed within the attached gingival margin if possible. These procedures were carried out under either local or general anaesthetic depending on the complexity of the procedure.
Following removal of the tooth/teeth, the sockets were carefully filled with 5% tranexamic acid solution so as not disrupt any clot formed, surgicel© (Johnson Johnson, New Yorkshire, UK) was then placed into the socket containing the clot and tranexamic acid and the surgical site was tightly closed with 4-monocryl© (Ethicon Johnson & Johnson, Somerville, NJ, USA) in the case of repositioning a mucoperiosteal flap or 3-0 Vicryl rapide© (Ethicon Johnson Johnson) to close sockets.
Patients requiring general anaesthesia were managed with a laryngeal mask to reduce the risk trauma and possible bleeding to the nose or vocal cords that could be caused by nasal or oral tube intubation. These patients had administration of local anaesthesia, Marcain 0.5% (Bupivacaine; AstraZeneca, Sydney, Australia) with 1:200 000 adrenaline, via infiltration and/or inferior alveolar nerve block as required, using a 27-gauge single use needle, aspiration was used to ensure the needle was not a vessel. As Marcain© is no longer available in dental cartridges, the local anaesthetic was drawn up from vial in a 10-mL syringe.
Patients having extractions in the chair under local anaesthesia were administered 2% xylocaine© (AstraZenica) 1:80 000 adrenaline via a single use 30 gauge needle for infiltrations and 27 gauge single use needle for inferior dental nerve blocks, auto-aspirating syringes were used. All patients were prescribed 5% tranexamic acid mouth wash to use three times a day as a gentle mouthwash for up to 7 days post operatively or to place on gauze to apply pressure to the socket in the case of moderate bleeding. The patients were given a questionnaire to complete and return to the Dental Clinic, they were advised to represent to the clinic or the hospital ED if there was any significant bleeding.
All patients were given a questioner to fill out for eight days postoperative, to provide information about any postoperative bleeding, returning this to the clinic (Form 1).

Data concerning the patients smoking habits, standard of oral hygiene and the use of COX-2 inhibitors for peri and post-operative analgesia was also collected and reviewed to determine if any of these factors contributed to post operative bleeding. As adequate post-operative pain relief was often a problem especially with the surgical extraction patients the use of COX-2 inhibitors was introduced, this involved Parecoxib 40 mg IV peri-operative with a follow up of oral Celebrex 100 mg bd for four to five days commencing the day after the procedure, as long as the patient had normal kidney function (Graph 1).
COX-2 inhibitors where used to obtain the required anti-inflammatory effect required post-surgery without the potentially detrimental anti-platelet effect of nonselective NSAIDs.

Graph 1: Total percentage of degree of post-op bleeding.
Results
The 250 consecutive inherited bleeding disorder patients consisted of 137 haemophilia A (27 severe, 22 moderate and 88 mild) 42 haemophilia B (4 severe, 4 moderate and 34 mild) 60 von Willebrand’s (3 type 3, 15 type 2 and 42 type 1) there were 11 patients with other factor deficiencies including factor VII and XI (Graph 2).
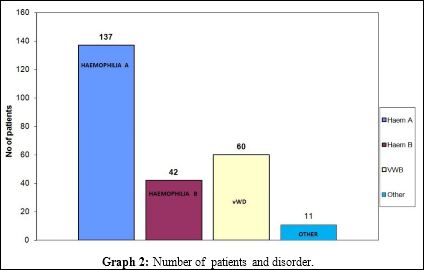
Graph 2: Number of patients and disorder.
All patients included in the study filled in and returned the post bleeding questioner (Form 1). A total of 422 extractions were performed on these patients, 147 surgical extractions (included muco- periosteal flap raised, tooth sectioning and or bone removal) and 375 simple extractions. A total of 172 inferior dental nerve blocks and 229 infiltration local anaesthetic injections were administered with no haematoma formation.
Of the 34 severe patients (factor activity < 1%) seventeen were on regular prophylaxis of 13-19 IU/Kg three times a week, as the surgery was always performed on a Friday this corresponded to the prophylaxis patients taking there usual does on the day of surgery. Sixteen were on demand factor support with factor being available at home for the patient to administer as required.
With von Willebrand’s type 3 If prophylaxis was for consideration it would be Biostate (pd FVIII /VWF ); the dose and frequency would be very individual. A total of 22 patients (8.8%) presented with a post-operative bleed that required some form of management for a total of 49 days (2.45% of duration of study time) (Graph 3 & Table 1).
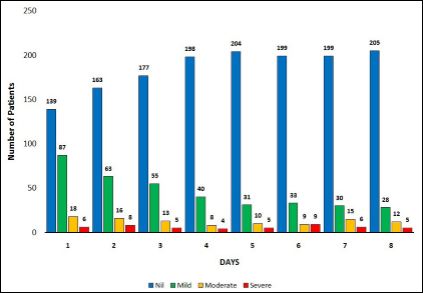
Graph 3: Total number of patients and degree of post operative bleeding.
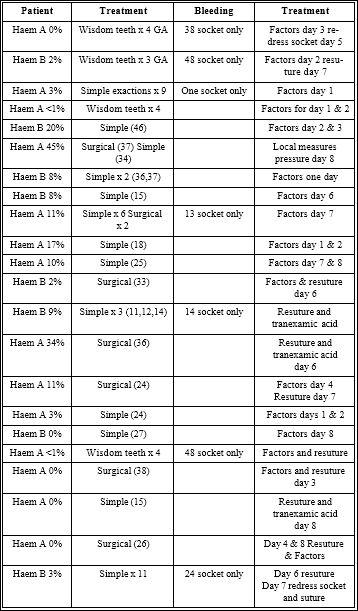
Of the severe patients 7 returned for some form of post-operative bleeding management (Table 1) this is 20.5% of these patients, for a total of 10 days of post-operative treatment (3.7% of duration of study time). Of the Moderate patients 5 returned for some form of post-operative bleeding management (Table 1) this is 12.2% of these patients, for a total of 8 days of postoperative treatment (2.4% of duration of study time). Of the Mild patients 10 returned for some form of post-operative bleeding management (Table 1) this is 6.1% of these patients, for a total of days of postoperative treatment (0.7% of duration of study time).
Conclusion
With careful surgical technique combined with the protocol of oral tranexamic acid 1 g tds for a day prior and seven day post surgery, the placement of surgical and 5% tranexamic acid into the socket and careful suturing of the socket Oral surgery can be safely carried out for patients with inherited bleeding disorders with the use of minimal factor support.
Inferior dental nerve blocks can be safely administered using single use 27 gauge needles and careful technique.
With surgical cases as Cox-1 inhibiting NSAIDs cannot be used we found there was a problem in achieving adequate post-op pain control with Panadol or opioids, in consultation with the haemophilia unit it was decided to provide these patients with peri-operative IV and post-operative oral administration of Cox-2 inhibitors. The use of Cox-2 inhibitors to obtain adequate post-operative pain management does not increase the risk of post-operative bleeding, Cox-2 inhibitors were only used in general anaesthetic cases, which involved the surgical removal of wisdom teeth or multiple extractions scenarios that would be expected to have a higher risk of post-operative bleeding than single or simple extractions.
The reduction in factor usage reduces the risk of haemophilia patients developing inhibitors and possible blood borne diseases, there is a significant decrease in cost of treatment with a reduction in factors used and duration of hospitalisation.
We recommend that any inherited bleeding disorder patients who have severe disease are managed in the hospital setting that has a haemophilia treatment centre that can provide expert assessment of their possible factor requirements and have oral surgery facilities with the required expertise, patients who have moderate or mild disease maybe managed away from this setting if the appropriate protocols outlined in this paper are followed carefully.
All patients were assessed to determine if smoking or non-smoking, good or poor oral hygiene and the use of Cox-2 inhibitors had any effect, either positive or negative on post-operative bleeding events (Graph 1). There was no significant difference in post-operative bleeding events between smokers and non-smokers, good and poor oral hygiene and the use of Cox-2 inhibitors.
Smokers were patients who were currently smoking; those who had previously quit were classified as non-smokers.
Patients were classified as having poor oral hygiene when there was an obvious plaque and or calculus deposit or obvious periodontal disease.
References
- Brewer A, Correa ME (2006) Guidelines for Dental Treatment of Patients with Inherited Bleeding Disorders. World Federation of Hemophilia, Montreal, Quebec, Canada.
- Frachon X, Pommereuil M, Berthier AM, Lejeune S, Hourdin-Eude S, et al, (2005) Management options for dental extraction in hemophiliacs: a study of 55 extractions (2000-2002). Oral Surg Oral Med Oral Pathol Oral Radiol Endod 99: 270-275.
- Franchini M, Favaloro EJ, Lippi G (2010) Mild hemophilia J Thromb Haemost 8: 421-432.
- Givol N, Hirschhorn A, Lubetsky A, Bashari D, Kenet G (2015) Oral surgery-associated postoperative bleeding in haemophilia patients a tertiary centre’s two decade experience. Haemophilia 21: 234-240.
- Heiland M, Weber M, Schmelzle R (2003) Life-threatening bleeding after dental extraction in a hemophilia A patient with inhibitors to factor VIII: a case J Oral Maxillofac Surg 61: 1350-1353.
- Hewson I, Makhmalbaf P, Street A, McCarthy P, Walsh M (2011) Dental surgery with minimal factor support in the inherited bleeding disorder population at the Alfred Hospital. Haemophilia 17: 185-188.
- Klein HG, Dodd RY, Dzik WH et al. (1998) Current status of solvent/detergent-treated frozen plasma. Transfusion (Paris) 38: 102-107.
- Mahlangu J, Powell JS, Ragni MV, Chowdary P, Josephson NC, et (2014) Phase 3 study of recombinant factor VIII Fc fusion protein in severe hemophilia A. Blood 123: 317-325.
- Mulkey TF (1965) Outpatient treatment of hemophiliacs for dental ex J Oral Surg 34: 428-434.
- Sindet-Pedersen S, Ramström G, Bernvil S, Blombäck M (1989) Hemostatic effect of tranexamic acid mouthwash in anticoagulant-treated patients undergoing oral surgery. N Engl J Med 320: 840-843.
- Stubbs M, Lloyd J (2001) A protocol for the dental management of von Willebrand’s disease, haemophilia A and haemophilia Aust Dent J 46: 37-40.
- Walker I, Pai M, Akabutu J, Ritchie B, Growe G, et al. (1995) The Canadian Hemophilia Registry as the basis for a national system for monitoring the use of factor concentrates. Transfusion 35: 548-551.
- Hewson ID, Daly J, Hallett KB, Liberali SA, Scott CL, et (2011) Consensus statement by hospital based dentists providing dental treatment for patients with inherited bleeding disorders. Aust Dent J 56: 221-226.
Citation: Hewson I, Hutcheson A (2017) Management of the Inherited Bleeding Disorder Patients Undergoing Oral Surgery Procedures at the Alfred Hospital. J Hematol Hemother 2: 004.
Copyright: © 2017 Hewson I. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and re- production in any medium, provided the original author and source are credited.