*Corresponding Author:
María Santos,
Clinica Alemana (Clínica Alemana), Santiago, Chile
Tel: +56 982561025
Email: mariasantosc@gmail.com
Abstract
Hydronephrosis (HN) can be found on ultrasound in 1-5% of pregnancies. This dilatation can be a transitory physiologic state like in most cases, however it can also entail congenital abnormalities. The antenatal diagnosis and the evaluation of these patients can identify complications at an early age, which helps preserve renal function.By far the most common etiology of Antenatal Hydronephrosis (ANH) is Transient HN (THN). There is no uniformity on how to define, classify or grade HN, neither on antenatal or postnatal US. Our main objective is to describe the management of patients with ANH at a public hospital in Chile, during a period of 10 years. We retrospectively reviewed the charts of patients with ANH in our hospital. 75 renal units were available to be classified with antenatal ultrasound. The most common etiology in our series was transient HN and only 23% had urinary abnormalities. 2% of antenatal US were classified as mild HN requiring surgery, compared to 13% and 33% for moderate and severe HN respectively. 61% resolved spontaneously in postnatal ultrasound. 27 patients presented UTI during follow up, 14 of the patients who developed UTI were surgically resolved. Due to the variability of our findings compared to the literature we propose a protocol for the management and study of AHN and a prospective study to evaluate the results after the implementation of the protocol.
Keywords
Antenatal diagnosis; Antenatal ultrasound; Hydronephrosis; Megaureter; Ureteropelvic junction obstruction; Vesicoureteral reflux
Introduction
Hydronephrosis (HN) or dilatation of the renal collecting system with or without dilatation of the renal calyces can be found on ultrasound in 1-5% of pregnancies [1]. It is more frequent in boys than girls, with a ratio of 2:1 respectively, and it has bilateral presentation in 20-40% of cases [2]. This dilatation can be a transitory physiologic state like in most cases, however it can also involve congenital abnormalities such as clinically significant urinary collecting systemobstruction or Vesicoureteral Reflux (VUR), which can lead to future complications like Urinary Tract Infection (UTI), kidney stones and renal dysfunction or failure. The antenatal diagnosis and the evaluation of these patients can identify complications at an early age, which helps preserve renal function [1,3].
The most common etiologies of Antenatal Hydronephrosis (ANH) are Transient HN (THN), Pyeloureteral Junction Obstruction (PUJO), VUR, Ureterovesical Junction (UVJ) obstruction, megaureters, multicystic dysplastic kidney, Posterior Urethral Valves (PUV), ureterocele, ectopic ureter, duplex system, urethral atresia, among others [1]. Of all the mentioned THN is the more frequent with an incidence reported from 64-94%.
There is no uniformity on how to define, classify or grade HN, neither on antenatal or postnatal US. To assess ANH the most common parameter used is the measurement of the Anterior- Posterior Diameter (APD) of the renal pelvis. Usually, APD cannot identify a specific disease but it is used as a marker of potential congenital renal abnormalities. The dimensions of renal pelvis increase with gestational age so the threshold APD values for early and later gestational age vary according to this [1,4]. Furthermore, APD is a dynamic parameter affected by many factors, such as hydration, bladder filling, position and respiration. As there is no consensus on grading HN there are many different classifications used for antenatal and postnatal diagnosis, including renal pelvic diameter, the Society of Fetal Urology (SFU) criteria and Urinary Tract Dilation (UTD) [3,5,6].We used SFU for antenatal classification as we considered it the most specific classifications including not only APD and UTD for postnatal classification as we did not have all the information required to classify it according to SFU postnatal classification; P1 was considered <10mm and P3 was considered >15mm or with any of the following; additional ureteral dilation, abnormal renal echogenicity or cysts, or bladder abnormalities regardless of DAP measurement.
When treating a postnatal diagnosis of HN, we know that mild HN usually does not require further evaluation, moderate HN should resolve spontaneously before 18 months and severe HN are at risk of developing kidney disease that requires surgical correction, therefore requiring further studies and a stricter follow up [7].
Our main objective is to describe the management of patients with antenatal diagnosis of HN at a public hospital in Chile, during a period of 10 years. Furthermore, we analyzed the antenatal history, additional imaging studies, and the presence of UTI during follow up, hospitalizations, antibiotic prophylaxis and surgeries performed. Comparing our management with international literature hence creating a standardized management protocol for these patients.
Materials and Methods
Medical records of patients with diagnosis of AHN during the last ten years (2010-2020) were selected and reviewed. Inclusion criteria were patients who were born between 2010 and 2020 and those who had antenatal diagnosis of hydronephrosis.
Medical records of all patients were reviewed for gestational age at birth, pregnancy complications, comorbidities, family background, age of diagnosis, imaging study, surgeries performed, imaging studies and treatments received. Exclusion criteria were: (i) Patients with postnatal hydronephrosis diagnosis. (ii) Patients born before 2010.
Patient information was registered in a secure web database called “REDcap” in a confidential way; access was granted to only one of the researchers.
To analyze certain parameters, we investigated each renal unit separately, instead of each patient. Every renal unit that presented altered findings in the antenatal US was selected and its follow up was reviewed from its chart.
Demographic and variable data were presented using summary statistics. Categorical variables were evaluated as a frequency in percentages. The means and interquartile ranges of continuous variables such as patient’s age or gestational age of diagnosis were calculated.
The study was approved by the Ethics Review Board of Hospital Padre Hurtado and Metropolitan south west health service of Santiago, Chile. Exemption of informed consent was approved.
Results
A total of 83 patients were included in this study from January 2010 to November 2020. Only 7 patients were preterm neonates, the median gestational age at birth was 38 weeks. 24 patients had pregnancy complications, needing urgent c-section in the majority. These pathologies were: premature rupture of membranes, intrauterine growth retardation, acute fetal distress, preeclampsia, gestational diabetes, syphilis, oligohydramnios and macrosomia. (Table 1) 23 patients had comorbidities such as recurrent UTI, constipation, luxating hip dysplasia, recurrent wheezing, chronic malnutrition, among others (Table 2). No patients had family history of nephrological disease.
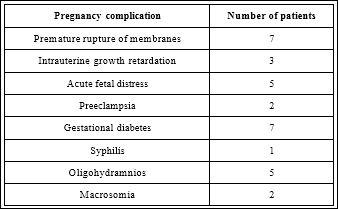
Table 1: Patients with pregnancy complications.
The median of gestational age of antenatal diagnosis was 33 weeks. Regarding laterality, 3 patients had only right HN, 23 had only left and 55 had bilateral (66%).
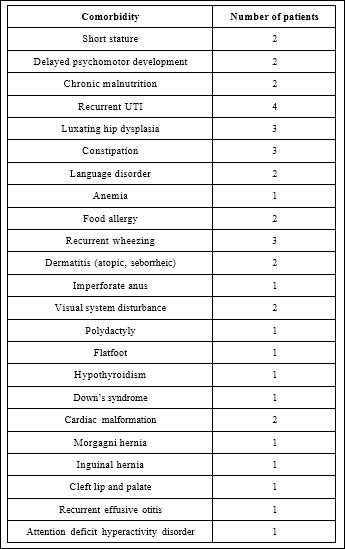
Table 2: Patients comorbidities.
Only 52 out of 83 patients had sufficient antenatal ultrasound values to classify them according to the SFU classification and 67 had postnatal ultrasound values that had sufficient information to classify UTD classification.
Of the 52 patients who had an antenatal US that were able to be classified, 75 renal units were available to be classified, of these 46 (61%) resolved spontaneously in postnatal ultrasound. Of the 75 renal units, 35 (47%) were mild HN, of these only one (3%) had surgical treatment because of a PUJO. 31 (41%) renal units with moderate HN, of these 4 (13%) had surgery related to their HN. On the other hand, only 9 (12%) renal units were classified as severe HN, of these 3 (33%) had surgical treatment with the diagnose of VUR, obstructive megaureter and double PU system (Table 3).

Table 3: Laterality and surgical procedure according to severity.
39 renal units were classified as moderate to severe HN on postnatal US, and of these 26 (67%) had further studies. Postnatally 20 patients were studied with renal MAG 3, 19 patients had a renal Tc-99 DMSA and 24 had a VCUG, the findings of each study are described in table 4.

Table 4: Further Studies in moderate to severe HN (26 of 39 renal units (67%)).
27 patients presented UTI during follow up, of these 14 (52%) where febrile managed as inpatients with cephalosporins or aminoglycosides and the most common microbe was Escherichia Coli. 14 (52%) of the patients who developed UTI were surgically resolved (they were not all the same patients who had a febrile UTI). 60 patients were managed with Continuous Antibiotic Prophylaxis (CAP) and cefadroxil was the most common antibiotic in 55 patients (2 were not identified in medical charts). All patients were followed up through time with vesical and renal US: 46 patients had a second postnatal US, 27 had a third, 28 had a fourth, 18 had a fifth, 8 had a sixth, 5 had a seventh and 1 had an eighth postnatal US.
18 patients required a surgical intervention related to their HN, the most common diagnosis was megaureter, the different surgeries done are described in table 5 with its corresponding complications. 11 patients were circumcised, 9 in the same surgical procedure and 4 were isolated circumcision because of UTI.

Table 5: Surgical interventions and its complications.
Discussion
Postnatal HN can be classified as; transient, not pathological which includes dilatation in children older than one year without VUR or obstructive pathology and pathological includes patients with known etiology, generally urinary abnormalities. In our series the most common ANH etiology was transient, needing only US follow up and uroprophylaxis.
The most common etiology in our series of ANH was transient HN, the literature describes from 64-94% of ANH with no identifiable postnatal urinary abnormalities [8]. In our series only 23% (19/83) had urinary abnormalities. Only 2 % of antenatal US classified as mild HN had urinary abnormalities requiring surgery, compared to 13% and 33% for moderate and severe HN respectively. This is concordant with our management as we know that patients with severe HN have a higher risk of urinary abnormalities.
Further imaging studies were done in all but one (97%) renalunits that were classified as severe HN on postnatal US. On the other hand, 6/21 (29%) moderate HN on postnatal US required further imaging studies. This correlates with the risk of having associated urinary abnormalities that need further imaging studies. Therefore, our results confirm that patients with severe HN need further studies to rule out urinary malformations.
Half of the patients that presented UTI needed surgical treatment, therefore UTI would not be a prognostic factor for urologic abnormalities, as half of the patients were treated with conservative management (CAP and US follow up) with good response. The use of CAP is controversial and there is no formal consensus on the use of them. Song et al. [9] report a 36% incidence in patients with severe HN, which is less than ours. Furthermore, Braga et al. [10] report a 28.9% incidence of UTI in high grade HN patients with no CAP and 14.6% in patients using CAP. Patients with low grade ANH were similar whether or not CAP was used. Therefore, patients with high grade are benefited from the use of CAP. The indications in the reported literature [7] for CAP are: postnatal SFU grade 2 or higher, female patients, uncircumcised males in the first years of life, and patients with low ureteral dilation such as megaureter and UVJ obstruction.
There was no relation between antenatal complications during pregnancy or other pathologies with the degree of HN or urologic malformation.
The main limitation of this study is the lack of detailed information on the antenatal ultrasounds, as many charts were incomplete. The number of patients was scarce; therefore, no significant conclusions were able to be extracted. Added to this, the retrospective form of the study is also a limitation.
Conclusion
Our results are not surprising, as the majority of patients resolved spontaneously as known through many studies in literature. 54% were moderate to severe needing further studies to rule out malformations, which is the correct way to follow these patients. Therefore, our results are generally eliciting the knowledge of literature.
The grading system for HN is still not fully defined, antenatal and postnatal classifications are very heterogenous, having inter-rater variability. We believe that every multidisciplinary center should use only one single grading system for antenatal and postnatal periods, and therefore avoid inter-rater variability between urologists, surgeons, pediatricians and radiologists. This should lead to more precise and specific diagnosis and treatment.
Due to the variability of our findings compared to the literature we propose a protocol for the management and study of AHN and a prospective study to evaluate the results after the implementation of the protocol.
Acknowledgements
Ristopher Gumera. Informatics engineer, RedCap data manager. Department of biomedical informatics. ClinicaAlemana, Santiago Chile.
References
- Nguyen HT, Herndon CDA, Cooper C, Gatti J, Kirsch A, et (2010) The Soci- ety for fetal urology consensus statement on the evaluation and management of antenatal hydronephrosis. J PediatrUrol 6: 212-231.
- González R, Schimke CM (2001) Ureteropelvic junction obstruction in infants and children. Pediatr Clin North Am 48: 1505-1518.
- Baskin LS (2019) Overview of antenatal UpToDate.
- Oliveira EA, Oliveira MCL, Mak RH (2016) Evaluation and management of hy- dronephrosis in the neonate. Curr Opin Pediatr 28: 195-201.
- Nguyen HT, Benson CB, Bromley B, Campbell BB, Chow J, et (2014) Mul- tidisciplinary consensus on the classification of prenatal and postnatal urinary tract dilation (UTD classification system). J Pediatr Urol. 10: 982-998.
- Fernbach SK, Maizels M, Conway JJ (1993) Ultrasound grading of hydrone- phrosis: Introduction to the system used by the society for fetal urology. Pediatr Radiol 23: 478-480.
- Baskin LS (2020) Postnatal management of fetal UpToDate.
- Liu DB, Armstrong WR, Maizels M (2014) Hydronephrosis: Prenatal and post- natal evaluation and management. Clin Perinatol 41: 661-678.
- Song SH, Lee SB, Park YS, Kim KS (2007) Is antibiotic prophylaxis necessary in infants with obstructive hydronephrosis? J Urol 177: 1098-1101.
- Braga LH, Mijovic H, Farrokhyar F, Pemberton J, DeMaria J, et (2013) An- tibiotic prophylaxis for urinary tract infections in antenatal hydronephrosis. Pediatrics 131: 251-261.
Citation:Santos M, Lüer MI, Solano S, Recabal X, Acuña C (2021) Management of Antenatal Hydronephrosis 10 Year Experience In a Non-Pediatric Centre. A Retro- spective, Descriptive Study. J Perina Ped 5: 011.
Copyright: © 2021 Santos M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.