*Corresponding Author:
Delaune Leïlani,
Centre Hospitalier Universitaire Vaudois, Lausanne, Switzerland
Tel: +41 765890304
Email: delaune.leilani@gmail.com
Abstract
Background: Benign tumoral calcinosis is a rare disorder, often secondary to end-stage disease, hypercalcemia, hyperparathyroidism of hyperphosphatemia. Our case report presents a 76-year-old patient with an idiopathic benign tumoral calcinosis.
Case presentation: A female patient of 76-year-old, with a type 2 skin phototype, was admitted to the emergency department after a fall from standing height. Her only medical background was a road accident 46 years ago with a multioperated supracondylar left humeral fracture and a bilateral phacoemulsification. Through our clinical examination, a voluminous mass on the left elbow was observed and x-rays were taken of this elbow and of the right proximal humerus, since an opaque periarticular mass was fortuitously discovered on a thoracic x-ray.
A CT scan of these two localizations was performed and the presence of two fluid-calcium levels inside each lesion was pathognomonic of a benign tumoral calcinosis, but the patient refused any surgery of biopsy of the mass. Further test were realised to understand whether this disorder was secondary to another pathology, but the results came back negative, making us come to the conclusion that this disorder was this time, idiopathic.
Benign tumoral calcinosis has been described numerous times in literature. However, most of those articles described it in patients with a type 6 skin phototype, typically in adolescents or young adults, or secondary to end-stage renal disease, trauma, metabolic abnormalities, or a foreign body. Familial forms have also been described.
In our case, none of those disorders have been identified. Furthermore, our patient did have a traumatic event on the left elbow, but no history of trauma of the right shoulder was identified.
Conclusion: As a conclusion, our patient had a very rare form of idiopathic benign tumoral calcinosis diagnosed through diagnostic imaging, even though an anatomopathological examination remains the gold standard for diagnosis.
Keywords
Benign tumoral calcinosis; Case report; Clinical examination; Idiopathic; Physiopathology; Rare
Introduction
Numerous cases of benign tumoral calcinosis have been previously reported, but they are often secondary to end-stage renal disease (dialysis), hypercalcemia, hyperparathyroidism, or hyperphosphatemia.
Benign tumoral calcinosis (or pseudo-tumoral calcinosis) is a rare disorder, characterized by calcium deposits in periarticular soft tissue.
We present a case of an idiopathic benign tumoral calcinosis in a 76-year-old patient and discuss the radiological findings on X-ray, ultrasound, computed tomography and magnetic resonance imaging.
Case Presentation
A female patient of 76-year-old with a type 2 skin phototype, was admitted to the emergency department after a fall from standing height. A head trauma with no loss of consciousness, and a wrist deformity visible to the naked eye were present. No allergy and no underlying family pathology or oncologic history was known. Anamnesis included a road accident 46 years ago with a multi operated supracondylar left humeral fracture, and bilateral phacoemulsification.
Clinical examination was in favor of a distal right radial fracture. A voluminous mass on the left elbow was fortuitously observed. This mass, measuring 20cm in its major axis was painless, multinodular, and hard at palpation. No joint stiffness was present, with complete extension, flexion, and pronosupination possible. This mass appeared approximately 40 years ago, after a road accident responsible for multiple fractures. Three surgeries were necessary for treatment of the supracondylar humeral fracture. Following the surgeries, the mass appeared progressively, with intermittent production of a chalk-like liquid. No osteosynthesis equipment was present at time of consult.
A thoracic x-ray taken before hospitalization fortuitously showed the presence of an opaque periarticular mass located at the right proximal humerus. Additional x-rays of the right humerus were taken during her stay (Figure 1). These showed a large opaque mass located at the elbow joint, and an additional opaque mass located in the soft tissues of the proximal humerus.
A CT-scan of these two localizations was performed. The presence of two fluid-calcium levels inside each lesion was pathognomonic of a benign tumoral calcinosis (Figure 2). The patient refused any surgical treatment and/or biopsies of the mass.
Dosage of electrolytes, creatinine, and hormones were normal, except for a hyponatremia (due to a syndrome of inappropriate antidiuretic hormone secretion (Annex 1 and 2).
The CT-images and absence of any underlying cause allowed for diagnosis of a benign tumoral calcinosis.

Figure 1: X-ray of the right proximal humerus (a) and the left elbow (b).
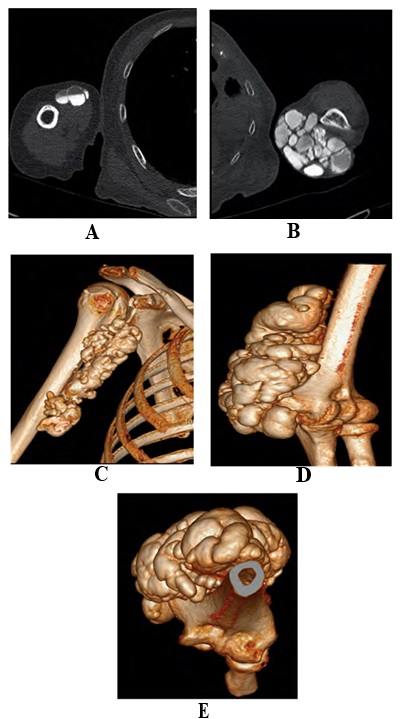
Figure 2: CT scan of the upper extremity of the right humerus (a+b+c): Coronal slice (a), axial slice (b), 3D reconstruction (c). CT scan of the left elbow (d+e+f): axial slice (d), 3D reconstruction (e+f).
Follow-up X-rays taken of the osteosynthesis of the distal right radius showed no abnormality.
Discussion
Benign tumoral calcinosis is a rare condition. Tumoral calcinosis is more frequently present in end-stage renal disease (hemodialysis), or with a hyperphosphatemia, hypercalcemia, or parathyroid diseases [1, 2].
Contrarily to our case, it has been described in patients with a type 6 skin phototype and typically affects adolescents or young adults. Common affected sites include the hip, shoulder, elbow, foot and wrist [1,3-9].
This disease was first described by Giard et al. in 1898 [2,3,5,10], and the term tumoral calcinosis was first used by Inclan et al. in 1943 [11,12,6]. Since then, more than 300 cases of tumoral calcinosis have been reported [1,11]. One retrospective study of 5 cases of pseudo- tumoral calcinosis [6,12-16] used standard x-rays, ultrasound, and a CT-scan for diagnosis
Review of the 300 cases reported showed a predominance of sporadic tumoral calcinosis secondary to end-stage renal disease [8,9,17,18]. Other cases are secondary to trauma, metabolic abnormalities (especially phosphocalcic), or a foreign body. In the case presented here, even if the tumoral calcinosis of the elbow was secondary to previous trauma, no history of trauma to the right shoulder was identified. Trauma was therefore an unlikely cause for the right proximal humerustumoral calcinosis.
Familial forms have also been described. They are linked with FGF23 deficiencies. Dosage of this protein was not performed in our case due to cost. However no other member of our patient’s family presented with this disease.
In this case, none of the previously cited pathologies were found. A benign tumoral calcinosis was therefore diagnosed.
Macroscopically (Figure 3), benign tumoral calcinosis nodules are nonencapsulated chalky masses, located in periarticular soft tissues. Histologically, they can be in an active or inactive phase. The active phase is identified by an amorphous calcified or granulated center associated with a surrounding macrophagic reaction: multinucleated giant cells and mononucleated inflammatory cells. The inactive phase is characterized by almost exclusively calcified material in a fibrotic tissue extending to the adjacent tissues [12,19,20]. However, biopsy is still needed in order to exclude other differential diagnosis, such as chronic tophaceous gout, milia, molluscum contagiosum or osteoma cutis [21].
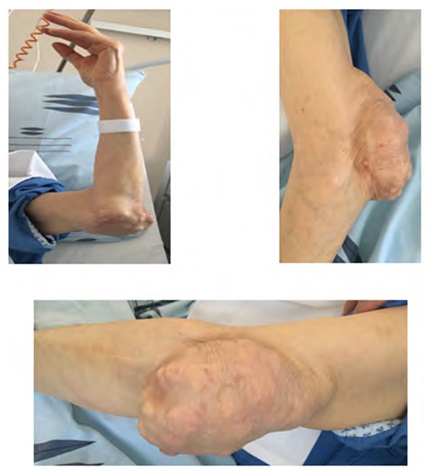
Figure 3: Physical examination.
Radiographic aspects of this disease are characteristic, with well delimited multilobulated calcified nodules, round or oval shaped, separated by fibrous septae. Adjacent bones and joints are generally not involved [7,8, 16,17,22-26]. As was seen with our patient, CT scanner shows high density, pseudo-cystic masses, separated by fibrous septae with multiple fluid-calcium levels caused by calcium layering (sedimentation sign), depending on the patient’s positioning [7-9,17,20,24,25,27].
The most useful exam is the MRI. T1-weighted sequences show inhomogeneous lesions with low signal intensity, T2-weighted sequences show inhomogeneous high-signal intensity despite calcification [8,17, 18,28,29].
Technecium-pyrophosphate scintigraphy shows hyperfixation to the pseudo-tumor [6-,8,23,30,31].
Treatment of idiopathic benign tumoral calcinosisis not essential if the patient is asymptomatique. However, if treatment is needed or desired, the treatment of choice is en bloc surgical resection of the tumor [21].
Electrolyte balance may be necessary. However, there is a high risk of recurrence, especially if surgical removal is incomplete.
Conclusion
Benign tumoral calcinosis is a rare condition, most frequently observed in end-stage renal failure, type 6 skin phototype patients, adolescents and young adults, with electrolyte imbalance or following trauma. It is very rarely idiopathic, as described in our case. Diagnostic imaging shows pathognomonic lesions, allowing for diagnosis. An anatomopathological examination of the lesion remains however the gold standard for diagnosis.
Treatment consists in total resection of the tumor, but the patient usually dictates whether this is indicated, depending on whether pain and/or discomfort are present. No case of malignant conversion has been reported, and risk of recurrence is high.
References
- 1. Hutt N, Baghla DP, Gulati V, Pastides PS, Beverly MC, et al. (2011) Acral post-traumatic tumoral calcinosis in pregnancy: A case report. J Med Case Rep
- 2. Franco M, Van Elslande L, Passeron C, Verdier JF, Barillon D, et al. (1997) Tumoral calcinosis in hemodialysis patients: A review of three Rev Rhum Engl Ed 64: 59-62.
- 3. Olsen KM, Chew FS (2006) Tumoral calcinosis: Pearls, polemics, and alternative possibilities. Radiographics 26: 871-885.
- 4. Harkess JW, Peters HJ (1967) Tumoral calcinosis: A report of six J Bone joint Surg Am 49: 721-731.
- 5. Lafferty FW, Reynolds ES, Pearson OH (1965) Tumoral calcinosis: A metabolic disease of obscure etiology. Am J Med 38: 105-118.
- 6. Ammar A, Ben Romdhane K, Khattech R (1994) La calcinose tumorale, étude anatomoclinique de 8 cas rapportés en Tunisie. Rev Chir Orthop Réparatrice Appar Mot 80: 262-266.
- 7. Mathieu G, Lemon F, Flouzat-Lachaniette, Sedel L CH (2006) Calcinose tumorale idiopathique: À propos de deux cas et revue de la littératureId- iopathic tumoral calcinosis: Two cases and review of the literature. Rev Chir Orthop Réparatrice Appar Mot 92: 358-363.
- 8. Fikri M, Allali N, Dafiri R (2007) Pédiatrie-la calcinose tumorale à propos de deux cas pédiatriques. J Radio 88: 595-598.
- 9. Huguet D, Legeay O, Guilleux C (2000) Calcinose pseudo-tumorale des deux pieds chez un hémodialysé Re Chir Orthop Reparatrice Appar Mot 86: 289-292.
- 10. Giard A (1898) Sur la calcification hibernale. Soc Biol 10: 1013-1015.
- 11. Inclan A, Leon P, Cameo MG (1943) Tumoral JAMA 121: 490-495.
- 12. Benchekroun TS, Benjelloun BS, Jorio-Bekhraba M, El Malki-Tazi A (1999) La calcinose tumorale - A propos d’un cas avec revue de la lit- térature. T Médecine du
- 13. Merzem A, Jadid I, Touil N, Chikhaoui N (2004) La calcinose pseudo-tu- morale: A propos de 5 Re Chir Orthop Reparatrice Appar Mot.
- 14. Rifi M, Kharmaz A, Bouchida A, Jahid A, El Bardouni Mo (2008) Calci- nose tumorale idiopathique bilatérale de la région trochantérienne: À propos d’un cas et revue de la littérature M yaacoubi rev marocchi or- thop traumato 34 : 48-50
- 15. Laleye A, biaou O, Ala MJ, Gbessi G, Adjagba M, et al. (2006) Darboux Rev Cames. Calcinose tumorale familiale: Aspects morphologiques et particularités Sériea.
- 16. Alj S, Dafiri R (2008) Rabat-Maroc Calcifications des parties molles chez l’enfant: A propos de 17 cas. Jfr.
- 17. En-Nafaa I, Africha T, Boussouga M, Semlali S, Chaouir S, et (2010) Tumoral calcinosis: A case report. Arch Pediatr 17: 1165-1168.
- 18. Barnacle AM, Gower PE, Mitchell AW (2002) Ultrasonography of acute and chronic tumoral calcinosis. Clin Radiol 57: 146-149.
- 19. Bard H, Kuntz D, Molle D (1984) Etude du métabolisme de phosphate dans un cas de calcinose Rev Rhum 51: 63 -68.
- 20. Haddad S, merzeau C, Montagne JPh (1989) Calcinose tumorale, rubri- que Arch F Pediatr 46: 373-374.
- 21. Kristen H Fernandez, Dana S Ward (2019) Calcinosis cutis: Etiology and patient Uptodate.
- 22. Palmer PE (1966) Tumoral Br J Radiol 39: 518.525.
- 23. Bittmann S, Gunther MW, Ulus H (2003) Tumoral calcinosis of the glu- teal region in a child: Case report with overview of different soft-tissue J Pediatr Surg 38: 4-7.
- 24. Hoskuldur B, Burke EE, Warren FD, Thomas JW (1969) Tumoral calci- nosis with hyperphosphatemia. Journal of Bone and Joint Surgey 51: 913-925.
- 25. Hug I, Gunçaga J (2014) Tumoral calcinosis with sedimentation sign. British Journal of Radiology 47: 734-736.
- 26. Knowles SAS, Declerck G, Anthony PP (1983) Tumoral Br J Surg 70:105-107.
- 27. Coumbaras M, Fossati P, Le hit P (2002) Opacités des parties molles. Feuil Radiol 42: 529-531.
- 28. Senol U, Karaali K, Cevikol C, Dinçer A (2000) MR imaging findings of recurrent tumoral calcinosis. Clin Imaging 24:154-156.
- 29. Neeman Z, Wood BJ (2003) Angiographic findings in tumoral Clin Imaging 27: 184-186.
- 30. Hacihanefioglu U (1978) Tumoral calcinosis: A clinical and pathological study of eleven unreported cases in Turkey. J Bone Joint Surg Am 60: 1131-1135.
- 31. Aprin H, Sinha A (1984) Tumoral calcinosis: Report of a case in a one-year-old child. ClinOrthop 185:83-86.
Citation:Leïlani D, Nils R, Thomas B, Thierry P, Stefan B, et al. (2021) Idiopathic Benign Tumoral Calcinosis: A Case Report. J Case Repo Imag 5: 034.
Copyright: © 2021 Leïlani D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.


