*Corresponding Author:
Beghdad Mohamed,
Department of Otorhinolaryngology, Head and Neck Surgery, King Université Hassan II, Casablanca, Morocco
Tel: +212 664689902
Email: mohamedbeghdad13@gmail.com
Abstract
Introduction: Facial paralysis is defined as a partial or total deficit of the motor function of the facial nerve responsible for asymmetry of the face; Hypoglosso-facial anastomosis is a classic method of rehabilitating the paralyzed face when the trunk of the facial nerve is not repairable and its peripheral branches are intact.
Methods: This is a prospective case study, spread over a period of two years from February 2018 to December 2019, carried out in the department of ENT and head and neck surgery of the hospital on August 20, 1953. 23 patients benefited from a surgical rehabilitation of their PFP. Their average age was 31.4 years. A male predominance was noted (17 men/6 women). The side of the facial paralysis most affected was the right side, the traumatic origin was the most common cause of PFP with a percentage of 74% of the cases techniques. The surgical tools used in our series were surgical decompression of the facial nerve in 58℅ of the cases, followed by hypo-glosso-facial anastomosis in 25℅ of the cases. The facial paralysis was total (Grade VI) in 61℅ of the cases, severe (Grade V) in 22% of the cases, and moderately severe (Grade IV) in 17% of the cases.
Conclusion: The rehabilitation of the paralyzed face remains a challenge for the surgeon because facial paralysis remains a vast area, which combines many technical procedures for each area of the face.
Keywords
Anastomosis; Facial paralysis; Hypo-Glossofacial; Surgery
Abbreviations
HFA: Hypoglosso-Facial Anastomosis
PFP: Peripherique Facial Paralysisv
Introduction
Facial paralysis is a source of functional and psychological disorders; it causes significant aesthetic damage as well as a double discomfort: That of the patient who would like to hide his paralyzed hemiface and that of the practitioner who knows that his easy diagnosis will be followed by an always delicate and often discussed therapeutic choice.
It is defined as a partial or total deficit of the motor function of the facial nerve responsible for an asymmetry of the face. Hypoglosso-facial anastomosis is a classic method of rehabilitating the paralyzed face when the trunk of the facial nerve is not repairable and its peripheral branches are intact. It remains a process of choice to rehabilitate the paralyzed face, since the facial nerve can no longer be reconstructed by suture or graft.
Our work aims to describe the indications, the surgical technique of rehabilitation of peripheral facial paralysis by hypoglosso-facial anastomosis whatever their etiologies as well as the post-operative monitoring of patients by comparing our results with data from the literature.
Patients and Methods
I- Patients
Our work consists of a prospective study on patients with periph- eral facial paralysis, treated surgically by termino-terminal hypoglos- so-facial anastomosis.
Inclusion criteria
- We included all patients with peripheral facial paralysis (all etiol- ogies combined) who benefited from surgical rehabilitation of the facial nerve by termino-terminal Hypoglosso-facial
- The grades of facial paralysis included in our series were grades V or more of the House and Brackmann classification
Exclusion criteria
- We excluded from our series all patients treated for PFP and hav- ing benefited from a surgical technique other than HFA.
II- Methods
This is a prospective case study, spread over a period of two years from February 2018 to December 2019, conducted in the department of ENT and head and neck surgery of the hospital August 20, 1953.
Results
a) Epidemiological data
During the study period, 23 patients underwent surgical rehabilitation of their PFP. Their average age was 31.4 years with extremes ranging from 4 years to 64 years. A male predominance was noted (17 men/6 women). The side of the paralysis most affected was the right side in 61℅ of the cases (14 patients), while the left side was affected in 35% of the cases (8 patients). Only one case of bilateral facial paralysis has been reported.
The mode of facial paralysis was immediate in 15 patients (65℅ of cases), and progressive in 8 patients (35℅ of cases).
b) Severity of the reach (classification of house and brackmann)
The degree of facial paralysis treated surgically was variable, ranging from moderately severe facial paralysis to complete facial paralysis. The facial paralysis was total (Grade VI) in 61℅ of the cases (14 patients), severe (Grade V) in 22% of the cases, and moderately severe (Grade IV) in 17% of the cases (4 patients) (Figure 1).
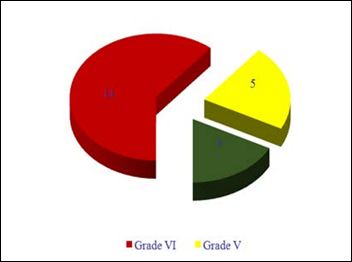
Figure 1: Severity diagnosis according to house and brackmann classification.
c) Etiological diagnosis
In our series, traumatic origin was the most common cause of PFP with 74% of cases (17 patients). Trauma to the rock was at the top with a percentage of 61% of cases (14 patients), followed by iatrogenic trauma in 13% of cases (3 patients), following ponto-cerebellar angle surgery in 9% of cases (2 patients), and to surgery for squamous cell carcinoma of the CAE in 4% of cases (only one patient). The sores of the face responsible for a section of the facial nerve are found in 13% of cases (3 patients). In 9% of cases (2 patients); facial paralysis is due to a neuroma of the facial nerve, while cholesteatoma is found in 4% of cases (only one patient).
d) Surgical management
The surgical techniques used in our series were surgical decompression of the facial nerve in 58℅ of the cases (14 patients), followed by hypoglosso-facial anastomosis in 25℅ of the cases (6 patients); (Figure 2) which is the subject of our study, then nerve suturing in 13% (3 patients), while nerve grafting was performed in 4℅ of cases (only one patient).
Discussion
The pre-therapeutique assessment of the patient
The patient who consults for a rehabilitation of the facial paralysis must benefit from a precise assessment in order to propose the most appropriate technique of management.
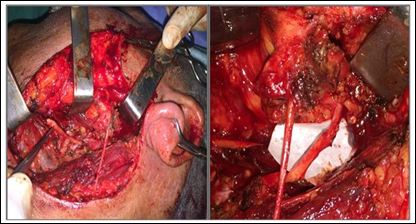
Figure 2: HFA surgical technique.
Interrogation
The interrogation makes it possible to specify: The clinical context in which the facial paralysis occurred, its date of onset, its mode of installation, its signs of accompaniment, its evolution, the assessments and the treatment already carried out. The start date must be specified for two reasons. To know if there is still a spontaneous evolutionary possibility and for the choice of the type of rehabilitation. The delay between the installation of the paralysis and the management also intervenes for the choice of surgical techniques, an HFA remains possible during the 3 to 4 years following the attack.
Physical examination
Allows to grade FP according to the classification of House and Brackmann. It allows to differentiate complete or almost complete FP (grade V and VI), and paralysis having recovered with sequelae (grade III and IV) type of spasms and synkinesias. These sequelae are better evaluated by the Sunnybrook grading. An electromyographic evaluation completes this clinical examination.
a) Topographic assessment Schirmer’s test
Compare the humidification of a blotting paper placed in the lower conjunctival cul-de-sac on the paralyzed side and the healthy side, In case of pathological result (unilateral lacrimal deficit), it locates the damage upstream of the large superficial petrous nerve (origin at the level of the geniculate ganglion) or on its path (isolated involvement of this contingent without affecting the rest of the facial functions, in particular motor) [1].
Stapedian reflex
It is abolished in the event of a lesion located upstream or on the stapedial nerve (origin on the mastoid portion of the facial). About 50% of patients with hemiface spasm have abnormalities in this reflex arch, normalizing after surgery [2].
b) Electroneuromyogram [3]
It makes it possible to confirm the existence of a lesion of the facial nerve, to characterize it (axonal or demyelinating involvement, conduction block), to quantify motor denervation and to provide prognostic information.
c) Imagery
CT scan of the rocks is only useful if there are petrous lesions. To be discriminating, it requires a high resolution exploration of the petrous pyramid, using 1.2 mm cuts every 0.5 mm in axial incidence and native coronal allowing, starting from axial acquisitions, reconstructions in all the planes of space, and in particular in the planes of sections parallel to the nervous path [4]. Magnetic Resonance Imaging (MRI) is used to characterize the normal and pathological facial nerve [5]. A moderate uptake of contrast can be observed in 76% of cases in the geniculate ganglion of the petrous nerves and at the beginning of the tympanic portion, apart from any pathology
Etiologies
a) Frigid or idiopathic facial paralysis
It is the most common cause of PFP, accounting for approximately 80% of patients. The evolution of knowledge to date has led many authors to no longer speak of idiopathic facial paralysis, but of herpetic facial paralysis [6]. Indeed, a bundle of clinical, paraclinical, and recent experimental approaches converge to implicate a resurgence of HSV1. Corticosteroids have the power to act powerfully on both the inflammatory factor. Treated patients show a significantly better prognosis than without treatment. The implication of herpes viruses has led some authors to evaluate the efficacy of aciclovir in addition to corticosteroid therapy [7].
b) Post traumatic facial palsies
- Trauma of the rock
One in five head trauma is associated with a fractured rock, 7% to 50% of which are complicated by facial dysfunction. The two regions most frequently involved are the elbow, between the second and third portion of the nerve, and the geniculate ganglion [8].
- Penetrating trauma
The associated damage is much more severe, comprising a very high proportion of nerve sections. The relative mediocrity of the results observed is unanimous, only 60% of patients obtaining a satisfactory result in grade III or IV.
- Iatrogenic trauma
The evolution of techniques and knowledge has considerably reduced the frequency of postoperative facial paralysis (0.06% according to Hermann [9]. The prognosis is very different depending on the site of the lesion and the immediate or delayed nature of the symptom.
II-Surgical treatment of peripheral facial paralysis with AHF
A-hypoglosso-facial anastomosis termino-terminale
The termino-terminale Hypoglosso-Facial Anastomosis (HFA tt) remains the method of choice for rehabilitation of the paralyzed face, as soon as the facial nerve can no longer be reconstructed by suture or graft and its branches at the periphery are intact [10].
Indications [10]
- Complete clinical facial paralysis with nerve inexcitability on the
- A spontaneous regression of the facial involvement is no longer possible due to the delay in paralysis which is a function of the lesion site, for example 9 months for the ponto-cerebellar
- The facial nerve is not (lesion in the angle or the brainstem) or is no longer repairable (delay greater than 1 year) or if direct repair fails beyond one year.
- The time since the onset of paralysis must not be more than 4 years except in special cases (long incomplete paralysis).
- The peripheral branches are intact, which eliminates the parotid
- The two hypoglossal nerves (ipsi and controlateral) are functional, as are the skin
- The extracranial facial nerve must be intact. The patient must be warned of the consequences of the interruption of XII (paralysis and amyotrophy of the hemi language) and psychologically ready to assume them.
Postoperative rehabilitative care [11]
Rehabilitation must be explained to the patient before the intervention. It begins the day after the surgical procedure with tongue movement exercises to correct denervation of the mobile hemitongue. These lingual exercises are associated with internal and external massages of the face initially promoting relaxation on the healthy side then decreasing the contracture that can appear on the operated side when the muscles are reinnervated.
B-HFA latero-terminale
By transposition of the mastoid facial, described in France by Vincent Darrouzet [12,13] is more complex. The result on the lingual function can deteriorate in the long term. Hypotonia can be marked, which explains why the number of reported failures is higher (3 grade 5 out of 19 patients in the series by Slattery et al. of (2014) [14]. Another study comparing HFA tt and HFA it shows that contractures and synkinesias are less important but the patients had not benefited from early rehabilitation [15].
C-Anastomosis XII-VII techniques with interposition graft [16]
It is identical to the hypoglosso-facial anastomosis technique, except that it involves the partial section of the hypoglossal nerve, by performing a neurolhaphietermino-lateral between the hypoglossal nerve and the interposition graft which is then connected to the facial nerve, preserving thus the hypoglossale ipsilateral function (May et al. 1991). It can be used when there is an ipsilateral dysfunction of the cranial nerves or if the patient does not want to accept the lingual sequelae.
Conclusion
Hetero-nerve anastomoses make it possible to re-innervate the paralyzed face in the event of impossibility of reconstruction of the facial nerve if the extracranial facial remains intact. Indeed, the HFA tt is a process of rehabilitation of the paralyzed face of simple realization, the results are remarkably consistent if the indications are respected and the patient is correctly rehabilitated but its drawbacks have led surgeons to think of d other alternatives of hetero-nervous anastomosis such as HFA and massetero-facial anastomosis. However, the choice of technique is adapted to the possibilities specific to each patient, to the extent of facial paralysis, and to the general condition of the patient.
References
- Darrouzet V, Houliat T, Fougere SL (2002) Paralysies Oto-Rhino-Laryngologie.
- Lacombe H (2009) Anatomie fonctionnelle du nerf facial functional anatomy of the facial Neurochirurgie 55: 113-119.
- Venail F, Mondain M, Uziel A, Shaadja J (1985) Exploration fonc- tionnelle et troubles du goût. Oto-Rhino-Laryngologie.
- Bonafe A, Holley P, Thorn M (1997) Imagerie normale et patho- logique du nerf facial intrapétreux. In: Charachon R (eds.). La paralysie faciale. Le spasme de l’hémiface. Rapport de la socié- té française d’ORL et de chirurgie cervico-faciale. L’Européenne d’édition,
- Girard N, Poncey M, Chays A, Florence A, Gignac D, et (1993) Exploration IRM du nerf facial intrapétreux. J Neuroradiol 20: 226- 238.
- Adour KK, Buboyeannes JM, von Doereten PG, Byl FM, Trent CS, et al. (1996) Bell’s palsy treatment with acyclovir and prednisone compared with prednisone alone: A double-blind, randomized, controlled Ann Otol Rhinol Laryngol 105: 371-378.
- Gantz BJ, Rubinstein JT, Gidley P, Woodworth GG (1999) Surgi- cal management of Bell’s Laryngoscope 109: 1177-1188.
- Nevoux J, Nowark C, Benoudiba F, Bobin S (2011) fractures du EMC.
- Castro D (1990) Facial nerve. Proceedings of the VIth internation- al symposium on the facial nerve, Rio de Janeiro, Bresil, 1988. Kugler and Ghedini publication, Amsterdam,
- Lamas G, Gatignol P, Barbut J, Bernat I, Tankéré F (2015) Reha- bilitation of the paralyzed face by hypoglosso-facial anastomosis. Indications and results. Hypoglossofacial anastomosis for facial palsy treatment: Indications and Annales de chirurgie plastique esthétique 60: 430-435.
- Demba C (2012) Aspects épidémiologiques, cliniques et théra- peutiques des paralysies faciales au CHU Gabriel Touré. Universi- té des Sciences, des techniques et des technologies de Bamako, Mali, West
- Darrouzet V, Dutkiewick J, Chambrin A, Stoll D, Bébéar JP (1997) Hypoglossal-facial anastomosis. Results and technical develop- ment towards end-to-side anastomosis with rerouting of the in- tra temporal facial nerve (modified May technique). Rev Laryngol Otol Rhinol (Bord) 118: 203-210.
- Atlas MD, Lowinger DS (1997) A new technique for hypoglos- sal-facial nerve Laryngoscope 107: 984-991.
- Slattery WH, Cassis AM, Wilkinson EP, Santos F, Berliner K (2014) Side-to-end hypoglossal to facial anastomosis with transposition of the intratemporal facial Otol Neurotol 35: 509-513.
- Le Clerc N, Herman P, Kania R, Tran H, Altabaa K, et al. (2013) Comparison of 3 procedures for hypoglossal-facial anastomosis. Otol Neurotol 34: 1483-1488.
- Sainsbury DCG (2019) Division of plastic and reconstructive sur- University of Toronto, Ontario, Canada.
Citation:Ardhaoui H, Beghdad M, Choukry K, Oukessou Y, Rouadi S, et al. (2020) Hypoglosso-Facial Anastomosis: Case Study and Review of the Literature. J Case Repo Imag 4: 020.
Copyright: © 2020 Ardhaoui H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.


