*Corresponding Author:
Thiago Mamoru Sakae,
Universidade do Sul de Santa Catarina (UNISUL), Tubarão-SC, Brazil.
Email: thiagosakae@gmail.com
Introduction
Postoperative anesthesia and analgesia for medium and large-sized thoracic and upper abdominal surgeries are still a great challenge to modern anesthesiology. Peripheral blocks for these surgeries are a major milestone in the adjuvant of intraoperative anesthesia and, mainly, in postoperative analgesia [1,2].
These frequently used blocks aim to prolong the time of postoperative analgesia and promote improvement in the quality of anesthesia and analgesia, in addition to reducing the consumption of anesthetics and venous opioids (intra and postoperative), with all the positive consequences, including early mobilization and reduction in the incidence and extension of atelectasis in the postoperative period, decrease in the incidence of thromboembolism and consequences of early non-mobilization [1,2].
There are many ultrasound-guided (USG) blocks described in recent years that are used as associated techniques and also for the treatment of chronic chest and abdominal pain. The Erector Spinae Plane Block (ESP) is a recent technique, originally described for controlling chest pain when performed at the level of the T5 vertebra [3,4], but its success has also been realized when used with abdominal analgesia when performed at the level of T8-10 or even lower levels [5,6].
ESP block has been described as relatively easier to perform when compared to other conventional blocks, such as epidural anesthesia and paravertebral block. The clinical findings of previous studies were supported by anatomical studies in cadavers that demonstrated the dissemination of the anesthetic solution injected in the deep interphase layer of the erector spine muscle, close to the intervertebral foramen, surrounding the dorsal and ventral portions of the nerve roots of the thoracic spine [3-6] (Figure 1).
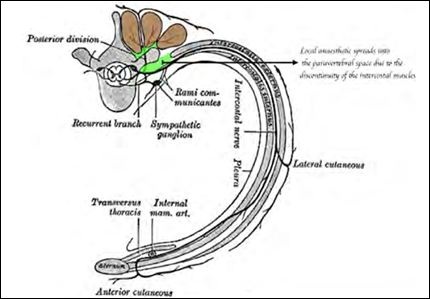
Figure 1: Brown highlighted structures indicate erector spinae muscles. The green highlighted area indicates local anaesthetic (LA) deposited below the erector spinae complex. The LA injection spreads into the paravertebral space because of the discontinuity of the intercostal muscles. Source: Henry Vandyke Carter [public domain], image reproduced from Gray’s Anatomy (figure 819; ‘‘Diagram of the Course and Branches of a Typical Intercostal Nerve’’). CC BY 3.0.
Some positions of the patient were well described: sitting, lying as an afterthought, or lying inclined. The method can be performed with the patient alert or under the effects of general anesthesia. However, there is no consensus about the best method for adult patients. The wakeful strategy gives the benefit of having the option to evaluate the viability and level of analgesia by methods for a skin sensitivity test [6,7].
Typically, a high-frequency linear ultrasound transducer is utilized to perform the block in the thoracic level, and a convex transducer is utilized to block the lombar level [7] (Figure 2).

Figure 2: Erector spinae plane sonoanatomy.
The probe is placed in a transverse direction to distinguish the spinous process. When the level is distinguished, the prove is moved 3 cm along the side until the transverse process is recognized.The probe must to be turned 90 degrees on the transverse process by setting it in a parasagittal plane. Three muscles must be distinguished as shallow to the hyperechoic transverse procedure shadow, and they are the trapezius, rhomboid major, and erector spinae. The needle is inserted in the plane. The technique can be acted in the cranio-caudal or inverse direction upon the conditions and the area to be treated [7] (Figure 1).
Thoracic Anesthesia
Due to the particularities related to the innervation of the rib cage, the retraction of the ribs and the incision of the chest wall muscles commonly make the thoracic surgery very painful in the postoperative period, requiring more intense analgesic control, after all, the thoracic bellows moves continuously with the movements of inhalation and exhalation. Their respective impact on respiratory mechanics is the same as that of patients with rib fractures and these patients will suffer the same complications if the pain is not treated aggressively [8,9].
The multimodal analgesic approach with the use of adjuvant thoracic paravertebral block or neuraxial block (neuraxial analgesia, example: Thoracic epidural analgesia or adjuvants via intrathecal). However, this will not be an adequate management for all patients, and the failure rates reported for thoracic Paravertebral Block (PVB) and thoracic epidural block (ASD) are up to 15% [8].
In a randomized study analyzing the use of ESP blocks in adults undergoing video-assisted thoracoscopic surgery, Ciftci et al., [9] compared opioid consumption and pain scores in single-dose ESP blocks with a control group (in these, without block). The results showed that there was a statistically significant less consumption of opioids and lower pain scores in the ESP group. In this study, they also found statistically lower rates of nausea and itching in the ESP group. This work suggested that ESP block is an opioid-sparing block suitable for patients undergoing video-assisted thoracoscopic surgery, but pain scores were measured only up to 24 hours, and there are not many studies comparing PVB / ASD with this technique. In open chest surgery, there are several case reports and case series that describe the successful use of ESP catheters for posterolateral thoracotomy analgesia [10,11].
Ribs fractures
ESP also has applicability in non-surgical patients, as in the case of patients with chronic pain and rib fractures. An American study showed analgesic results and the effect on respiratory volumes when performing ESP in patients with non-pathological (traumatic) rib fractures [12].
Incentive spirometry volumes, 12-hour opioid consumption and pain scores on the numerical scale highest (NRS) were recorded at baseline (ie pre-ESP block) and up to 72 hours after ESP. All patients received multimodal analgesia before blocking performance [12].
The majority (53%) had between 5 and 7 fractured ribs and 77% of patients received a PES catheter to allow a continuous infusion of LA in the myofascial plane, with the others receiving a single injection technique. The catheters remained in place until the acute pain team considered that the pain could be treated only with oral analgesia (mean duration of 3.7 days; range of 0.6 to 9.3 days) [12].
Incentive spirometry volumes almost doubled from baseline during the first 24 hours, with an average increase of 545 mL. In addi- tion, this effect was maintained for 72 hours. Maximum pain scores in numerical pain scale were statistically reduced significantly and opioid consumption in 12 hours was reduced in patients who received a continuous technique (but this did not reach statistical significance) [12].
There was no change in mean arterial pressure. Those who had a single injection ESP block showed less convincing results overall. The authors concluded that ESP block became the main regional intervention for patients with rib fractures at their institution. They also suggested its benefit in the safety profile for patients with contraindications to neuraxial and perineuraxial techniques (that is, anticoagulated patients) [12].
Scoliosis surgeries and other spinal deformities
Postoperative pain after scoliosis correction surgery is severe and usually requires prolonged intravenous opioid therapy. Regional anesthesia options are limited and include opioid and epidural intrathecal analgesia; however, they remain underused due to side effects and inconsistent effectiveness [1,13].
A two-level ESP block was described associated to a multimodal anesthetic regimen, along with a combination of several opioid-based intraoperative analgesic strategies [1]. Both patients had minimal pain in the emergency room. They successfully transitioned to oral analgesia on the first postoperative day, with modest opioid requirements, with no side effects and low pain scores during hospital stay [1].
Bilateral two-level ESP blocks are a simple method of providing preventive regional analgesia in extensive multilevel spine surgery. The integration of ESP blocks in a multimodal regimen that employs other opioid-sparing strategies can have additive and potentially synergistic benefits in improving postoperative analgesia and reducing opioid requirements [1,13].
Cardiac surgery
Cardiac surgeries involve a wide range of surgeries with procedures that require high intraoperative doses of anticoagulant agents and, therefore, regional anesthesia is traditionally avoided. Patients undergoing elective cardiac surgery with Cardiopulmonary Bypass (CPB) had significantly lower pain scores (up to 12 hours after extubation) if bilateral ESP blocks were performed instead of isolated standard therapy with venous analgesia [14].
In one study, that adverse events in the postoperative period, time for removal of the chest drain and time for the first mobilization were significantly shorter if ESP blocks were performed [15]. When comparing ASD and continuous bilateral ESP blocks for cardiac surgery, one study found scores pain, incentive spirometry, duration of the intensive care unit and number of days of ventilation with similar levels [16].
Breast surgery
Despite the various peripheral blocks specific to breast surgeries, ESP has shown to be promising as a regional technique for analgesia for these surgeries.
Studies have shown effective analgesia and reduced opioid consumption in the postoperative period when compared to standard treatment in patients undergoing surgery for breast cancer (including mastectomy) [17,18]. However, a prospective randomized study in radical mastectomy surgery showed lower postoperative pain scores and tramadol consumption if a modified pectoral nerve block (PECs 2) is performed instead of a ESP block [19].
Larger comparator studies need to be conducted to assess the true effectiveness and benefit of this surgical cohort, however, it seems that the blockages of this type are more effective in analgesia for mastectomies.
Abdominal surgery
Postoperative pain following a cholecystectomy using a Kocher incision, with a somatic and visceral component. More recently, ESP block proved its effectiveness, providing ample thoracic support [1,2,20], abdominal somatic and visceral analgesia [5,6,20], when performed at the T5-T6 level.
Therefore, bilateral ESP blocking the T8 cross-sectional process can provide effective post-cholecystectomy analgesia and reduce the incidence of adverse effects associated with opioid overuse [5,6,17]. On the other hand, the results of the study by Sakae et al., [21] show inferiority of the analgesic plan associated with ESP block, when compared to the group submitted to epidural anesthesia.
Technically, based on anatomical studies in fresh cadavers, the likely site of action of the ESP block covers an extensive area after the injection of local anesthetics, spreading through the dorsal and ventral regions of the thoracic spinal bundles and nerve branches [2,3,10,11].
Therefore, effective blocking of the ventral branch and sympathetic fibers is expected to occur concurrently and can promote effective anesthesia and analgesia, somatic and visceral pain control. In practical terms, however, thissatisfactory response of analgesia in thoracic surgery and abdominal wall, with stilllimited evidence in the literature to controlboth visceral and somatic pain [10,11,13,21].
Some studies on cadavers have shown that the dissemination of anesthetics injected through ESP in the ventral branches at multiple levels, in the neural foramen and the epidural spaces were not well established [14,19].
After injecting effective concentrations and volumes of local anesthetics using ESP, although there are reports showing relief from visceral and somatic pain, there arestill some variability in the treatment of visceral pain, without a consensusestablished in the control of this type of pain when anesthesia with ESP is done [14,19,21].
Other studies [15,18] documented the reach of local anesthetics was limited to branches only when performed at multiple levels and is unlikely to spread to the thoracic paravertebral space. There are studies reporting that ESP block was more limited to the dorsal branches andonly approximately 10% involved the ventral branch or the dorsal root ganglion [14,18] that could explain the differences between visceral and somatic pain control.
In addition, the use of adjuvants (corticosteroids, alpha 2 agonists, ketamine), already well established in other types of block, has not yet been described for the ESP Block, and could improve the potential of the block to control visceral pain that apparently does not occur in initial studies [19,21].
New approaches
There are plenty of case reports and small case series in the literature with positive results. Doctors investigated the effectiveness of ESP block in patients undergoing surgery on the upper limbs and spine. There is even a case report suggesting the effectiveness of the technique for a refractory tension headache. Several articles have suggested that ESP block can be used for chronic shoulder pain and upper arm surgery [22,23].
Conclusion
Based on the available evidence, ESP block should be considered an alternative analgesic option for patients with acute or chronic chest pain and even upper abdominal pain. Most favorable data for ESP block is based on its use as part of a multimodal analgesic package, and this should be considered when planning a patient’s care, including cases of clinical (and not only surgical) patients.
More research needs to be carried out to determine its potential compared to other regional techniques, as well as the best anesthetic doses and volumes to be used.
The fact that ESP does not seem to block the visceral abdominal component well may be effectively one of the limitations of the use of ESP for some types of abdominal surgeries, which is perceived in some thoracic surgeries and even hip arthroplasties, depending on the level at which the block is performed.
We need more comprehensives studies to assess the effectiveness of ESP for the visceral system, considering the specific level of block.
ESP is an easy-to-perform regional anesthesia technique, with a wide range of clinical applications, most current research has focused on its use in thoracic surgery and several experts consider ESP an alternative analgesic option to thoracic epidural and even paravertebral blocks, mainly in options which these techniques have some contraindication. It has a good safety profile, with few complications reported so far.
References
- Chin KJ, Dinsmore MJ, Lewis S, Chan V (2019) Opioid-sparing multimodal analgesia with bilateral bi-level erector spinae plane blocks in scoliosis surgery: A case report of two Eur Spine J.
- Blanco R (2007) TAP block under ultrasound guidance: The description of a ‘no pops trechnique’. Reg Anesth Pain Med 32:
- Chin KJ, McDonnell JG, Carvalho B, Sharkey A, Pawa A, et al. (2017) Essentials of our current understanding: Abdominalwall Reg Anesth Pain Med 42: 133-183.
- Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ (2016) The erector spinae plane block: A novel analgesic technique in thoracic neuropathic Reg Anesth Pain Med 41: 621-627.
- Tsui BCH, Fonseca A, Munshey F, McFadyen G, Caruso TJ (2019) The erector spinae plane (ESP) block: A pooled review of 242 cas J Clin Anesth 53: 29-34.
- Chin KJ, Adhikary S, Sarwani N, Forero M (2017) The analgesic efficacy of pre-operative bilateral erector spinae plane (ESP) blocks in patients having ventral hernia Anaesthesia 72: 452-460.
- Muñoz-Leyva F, Mendiola WE, Bonilla AJ, Cubillos J, Moreno DA, et al. (2018) In reply to “Continuous Erector Spinae Plane (ESP) block: Optimizing the analgesia technique”. J Cardiothorac Vasc Anesth 32: 3-4.
- Romero A, Garcia JEL, Joshi GP (2013) The state of the art in preventing post-thoracotomy pain. Semin Thorac Cardiovasc Surg 25: 116-124.
- Ciftci B, Ekinci M, Cem Celik E, Cem Tukac I, Bayrak Y, et (2019) Efficacy of an ultrasound-guided erector spinae plane block for postoperative analgesia management after video-assisted thoracic surgery: A prospective randomized study. J Cardiothorac Vasc Anesth 34: 444-449.
- Kelava M, Anthony D, Elsharkawy H (2019) Continuous erector spinae block for postoperative analgesia after thoracotomy in alung transplant J Cardiothorac Vasc Anesth 32: 9-11.
- Nath S, Bhoi D, Mohan VK, Talawar P (2018) USG-guided continuous erector spinae block as a primary mode of perioperativeanalgesia in open posterolateral thoracotomy: A report of two Saudi J Anaesth 12: 471-474.
- Adhikary SD, Liu WM, Fuller E, Cruz-Eng H, Chin KJ (2019) The effect of erector spinae plane block on respiratory and analgesic outcomes in multiple rib fractures: A retrospective cohort Anaesthesia 74: 585-593.
- Kline J, Chin KJ (2019) Modified dual-injection lumbar Erector Spine Plane (ESP) block for opioid-free anesthesia in multi-level lumbar Korean J Anesthesiol 72: 188-190.
- Krishna SN, Chauhan S, Bhoi D, Kaushal B, Hasija S, et al. (2019) Bilateral erector spinae plane block for acute post-surgical pain in adult cardiac surgical patients: A randomized controlled J Cardiothorac Vasc Anesth 33: 368-375.
- Macaire P, Ho N, Nguyen T, Nguyen B, Vu V, et al. (2019) Ultrasound-guided continuous thoracic erector spinae plane block within an enhanced recovery program is associated with decreased opioid consumption and improved patient postoperative rehabilitation after open cardiac surgery a patient-matched, controlled before-and-after J Cardiothorac Vasc Anesth 33: 1659-1667.
- Nagaraja PS, Ragavendran S, Singh NG, Asai O, Bhavya G, et al. (2018) Comparison of continuous thoracic epidural analgesia with bilateral erector spinae plane block for perioperative pain management in cardiac Ann Card Anaesth 21: 323-327.
- Gürkan Y, Aksu C, Kuş A, Yörükoğlu UH, Kılıç CT (2018) Ultrasound guided erector spinae plane block reduces postoperative opioid consumption following breast surgery: A randomized controlled J Clin Anesth 50: 65-68.
- Altıparmak B, Toker MK, Uysal AI, Demirbilek SG (2019) Comparison of the efficacy of erector spinae plane block performed with different concentrations of bupivacaine on postoperative analgesia after mastectomy surgery: Randomized, prospective, double blinded BMC Anesthesiol 19: 31.
- Altıparmak B, Toker MK, Uysal AI, Turan M, Demirbilek SG (2019) Comparison of the effects of modified pectoralnerve block and erector spinae plane block on postoperative opioid consumption and pain scores of patients after radical mastectomy surgery: A prospective, randomized, controlled J Clin Anesth 54: 61-65.
- Chin KJ, Malhas L, Perlas A (2017) The erector spinae plane block provides visceral abdominal analgesia in bariatric surgery: A report of 3 Reg Anesth Pain Med 42: 372-376.
- Sakae TM, Yamauchi LHI, Takaschima AKK, Brandão JC, Benedetti RH (2020) Comparison between erector spinal plane block and epidural block techniques for postoperative analgesia in open cholecystectomies: A randomized clinical Rev Bras Anestesiol 70: 22-27.
- Ueshima H, Inagaki M, Toyone T, Otake H (2019) Efficacy of the erector spinae plane block for lumbar spinal surgery: a retrospective Asian Spine J 13: 254-257.
- Ueshima H, Otake H (2019) Successful cases of bilateral erector spinae plane block for treatment of tension J Clin Anesth 54: 153.
Citation: : Brandão JC, Sakae TM (2020) Erector Spine Plane Block in Different Surger- ies. J Anes Perio Manag 4: 005.
Copyright: © 2020 Brandão JC, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.