*Corresponding Author:
Naveen Yadav,
Intensive Care Unit, Level 4, Royal Adelaide hospital, Port Road 5000, Adelaide, South Australia
Email: nyadav01@sa.gov.au; naveen.dv2@gmail.com
Abstract
Use of bedside ultrasound by intensive care provider is increasing for vascular access, invasive procedural real time guidance, diagnostic, therapeutic, and progress during critical/Intensive care unit stay. Multiple of literatures are available on ultrasound uses in critical care setting. We review the recent literature related to vascular access, lung ultrasound, echocardiography, use in trauma patients, airway examinations, for guiding fluid therapy and use for cardiopulmonary resuscitation.
Keywords
Ultrasound by intensivist in intensive care; Echo-guided pericardiocentesis; Pericardial effusions
Introduction
Ultrasound has emerged as versatile tool for various specialities of medicine. Ultrasound has found exit from its radiology suites and from the mastery of radiologist to real bedside tool for diagnosis and intervention in real time. Its benefits, in general, includes easy easily available, low running cost, portable, availability of different types of probes and non-invasive. A critically ill patient requires investigations for concluding a diagnosis and to evaluate the response to the therapy. Also, at times, certain invasive procedures are required in such critically ill patients. Shifting these patients out of the Intensive care unit area is challenging and carries a lot of risk during transport. Availability of ultrasound has circumvented many of these issues. Ultrasound has emerged truly as point of care tool for the critically ill patient. Its use has been not only for diagnostic purpose but also for real time therapeutic intervention tool as well (Table 1). Use of ultrasound increases the safety of procedure done in intensive care unit. Echo-guided pericardiocentesis is a safe, standard practice for clinically significant pericardial effusion [1]. Echo-guided pericardiocentesis with extended catheter drainage are considered as primary management strategy for clinically significant pericardial effusions in paediatrics patients [2]. Use of ultrasound for thoracentesis & paracentesis is associated with decreased risk of pneumothorax & bleeding complications respectively [3]. Ultrasound guided percutaneous dilatational tracheostomy provide a more safety than unguided tracheostomy [4]. A lot of invasive procedures can be done with ultrasound like, foreign body identification, suprapubic aspiration, abscess incision and drainage and arthrocentesis.
A lot of invasive procedures are done with help of ultrasound with less complication like central venous catheterization, arterial catheterization, and pericardiocentesis in ICU. It helps in ideal location for insertion of needle and catheter for localised collection. In percutaneous tracheostomy it helps in avoiding unintentional injury. Ultrasound for lung scan [1] detects various lung conditions like pleural effusion, pneumothorax, lung consolidation, lung abscess and alveolar recruitment in critical care setting. This reduces the x-ray and CT scan exposure [2] and prevents shifting patient outside ICU. No ionising radiation makes it safe for children and pregnant female. In trauma patients, Focussed Assessment Sonography in Trauma (FAST) and eFAST are done for abdominal and chest injury. Airway scan done for airway trauma with ultrasound in real time. Ultrasound is used by critical care provider for doing echocardiography and detect basic feature of cardiovascular system like wall motion abnormality, ventricular contractility, valve status, size of cardiac chamber and pericardial fluid. It detects intravascular fluid status and response to volume replacement. During cardiopulmonary resuscitation it gives valuable information regarding different causes of arrest, prognosis of the resuscitation effort and can guide correct management of the situation. Ultrasound finds the source of embolus by detecting thrombus in vascular lumen. If pulmonary embolism occurs ultrasound can give important information in echocardiography. New uses of ultrasound are increasing in literature which supports its use in intensive care unit. Multiple studies show benefit of the use of ultrasound in the critical care setting for specific condition.
Airway
Ultrasound has an emerging role in airway armamentarium for critical care unit. It has its role not only for assessment of the airway but also aids the real time airway management.
Assessment
The airway assessment may be done with linear array probe usually but at time curvilinear probe may be required for specific evaluation. Assessment and evaluation of airway and pre tracheal structure before intubation increases the probability of detection of difficult airway [5]. Suprahyoid and infrahyoid structures are visible in medial, sagittal, or transverse view. Thyroid cartilage, cricoid, epiglottis, and vocal cord, sub glottis and tracheal rings are observed. Ultrasound detects subglottic stenosis and prediction of paediatric ETT [6] and DoubleLumen Tube (DLT) size [7]. Sublingual ultrasound examination is new in the assessment of airway.
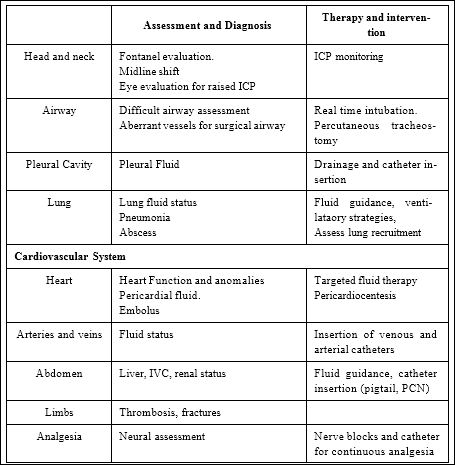
Table 1: Role of ultrasound in critically ill patient.
Ultrasound is also useful for surgical airway. It helps in assessing the correct landmark like cricothyroid membrane, tracheal rings, and presence of any aberrant vessels. Ultrasound can be used for detection of extubation success or failure (Figure 1). Strength of diaphragm is directly related to the extubation success. Downward displacement of liver and spleen due to diaphragmatic movement predict the success. Ultrasound image air column width in vocal cord can be used for predicting post extubation stridor [8].

Figure 1: Ultrasound for assessment of extubation.
Intervention
Real time dynamic endotracheal intubation can be done. Ultrasound confirm correct endotracheal and bronchial tube placement easily through direct visualisation of tube going through vocal cord or in oesophagus (Figure 2), [9] diaphragmatic movement or lung sliding sign. Direct visualisation of intra tracheal tip is difficult in adult but in neonate it can be visualised, and it can be confirmed [10]. Oesophagus is seen as a cauliflower shape structure in poster lateral to trachea in the transverse view, deglutition confirms this as peristalsis is seen in ultrasound image [11].
Percutaneous dilatational tracheostomy and cricothyroidotomy can be performed under ultrasound guidance with fewer complications compared to blind technique [12]. Tracheostomy is done between 2nd and 3rd tracheal ring most commonly (Figure 3). With the use of ultrasound tracheal rings and vessels are identified and high placement of the tube, vessel puncture avoided [13] by guiding the needle and guide wire in real time. Guide wire and final tracheal tube positions were immediately verified with bronchoscopy further enhance the surety of correct level. Patients with morbid obesity, sub-optimal palpable neck anatomy, previous tracheostomy or cervical spine injury can also tracheotomised with use of ultrasound successfully.

Figure 2: Transverse view of neck showing vocal cords.

Figure 3: Sagittal scan of the neck showing tracheal cartilages.
Lung and Pleural Cavity
Assessment
Ultrasound has found its important indispensable role for assessment of thoracic cavity including lung and pleural cavity for critically ill patients. Ultrasound beam scatters and disperses sound waves by air. Lichtenstein work on lung ultrasound gives us knowledge of different pattern of ultrasound image due to change in water air ratio in various lung diseases and it gives a lot of information about condition of lung. Linear and curvilinear probe are used for viewing superficial like pleura and deep structure in the lung.
Pleural cavity
Ultrasound has been used for assessing for presence and quantification of fluid in the pleural cavity. At times, it is useful to detect loculations of the fluid filled cavities and thus appropriate intervention. It is also used for assessing the response to the intervention like chest tube drainage.
Lung
The blue protocol is designed for early diagnosis of acute respiratory failure with use of ultrasound [14]. In this protocol patient position is semi recumbent or supine if patient is intubated. Longitudinal scan of upper and lower half of three wall of chest anterior, lateral, and posterolateral gives six zone of investigation. Depending on presence or absence of different signs various lung conditions can be diagnosed in about 90.5% of cases [15].
Intervention
Diagnostic thoracocentesis with the use of ultrasound is associated with a reduced rate of pneumothorax and tube thoracostomy [11]. Ultrasound-guided thoracocentesis is a safe procedure, any amount of fluid drained in one session [16].
First analysis of artifacts i.e. ‘A’ lines and ‘B’ line: ‘A’ line are repetitive horizontal lines arising from the pleural line generated by intra alveolar air. ‘B’ lines are hyper echoic lines, comet tail shape, well defined, spreading up indefinitely, erasing ‘A’ lines, and moving with lung sliding arises from pleural line when lung sliding is present. Excess fluid in lung interstitium results in 3 or more number of ‘B’ line [17]. Second is the analysis of lung sliding sign: absence of lung sliding occurs when parietal pleura does not slide over visceral pleura. Third is presence or absence of alveolar consolidation and pleural effusion. Pleural effusion seen as anechoic and is located in most dependent area, quadrangular shape with a regular lower border of visceral pleura called as lung line, was required for the diagnosis. Shifting of the lung line toward the pleural line during inspiration is called the sinusoid sign. (Figure 4) For diagnosis of alveolar consolidation tissue like image pattern, absence of the lung line, absence of the sinusoid sign. Depending on the result of their observational study they suggested an algorithm for diagnosing different lung condition.

Figure 4: Lung Point.
- Anterior lung-sliding with predominant A-lines i.e. A-profile with presence of thrombosed vein in pulmonary embolism and absence of thrombus in vein needs posterolateral scan. Presence (in Pneumonia) or absence (in COPD or ASTHMA) of PLAPS (Postero Lateral Alveolar and/or Pleural Syndrome) suggest the
- Bilateral anterior scan predominant B line, B-profile with lung sliding (pulmonary edema) and without lung sliding in pneumonia.
- A-profile with absent lung-sliding (with lung point in pneumothorax and without lung point need other diagnostic modality).
- A/B profile is a half A-profile at one lung and half B-profile at another and C-profile in anterior lung consolidation (pneumonia).
Specificity and sensitivity for diagnosing with ultrasound above condition is more than 90 % [18]. Combination of above sign in ultrasound correctly diagnoses 90.5% lung conditions [18] like, pneumothorax, pneumonia, pleural effusion, pulmonary oedema, pulmonary embolism, COPD and asthma, lung consolidations.
Cardiovascular System
Assessment
Heart: Unstable patient in critical care with the aim of a quick diagnosis abbreviated and focused transthoracic echocardiography are done. TTE led to a change in management due to fluid deficit, fluid overload or where there was no significant abnormality on TTE, but which led to a management change, such as cessation of cardiac failure medication in 49% of cases [19]. Focus Assessed Transthoracic Echocardiography (FATE) protocol are followed by critical care providers performed from four transthoracic positions subcostal, parasternal, and apical views of the heart, as well as the left and right pleural views [20]. With TTE in 97% of the patients one or more image obtained which helps us to take a decision [21]. This basic examination diagnoses the majority of life threatening conditions like pericardial tamponade, wall motion abnormality and hypovolemia. Repeated examinations allow us to monitor therapeutic intervention and patient progress [22]. Qualitative measure of ejection fraction of left ventricle can be estimated by observation and is comparable to quantitative measures [23]. Echocardiography do accurate hemodynamic evaluation of right ventricular function in patients at risk for acute cor pulmonale [24]. Acute pulmonary embolism and other right ventricular dysfunction results in dilatation, hypokinetic, abnormal motion of the interventricular septum, Dshaped LV, tricuspid regurgitation, and lack of collapse of the inferior vena cava during inspiration [25]. For pericardial effusion subcostal view for diagnosis and guided therapeutic intervention is safe and effective [26]. Kissing sign i.e. papillary muscle of the left ventricle approximate in systole is suggestive of hypovolemia. In shock that require prompt intervention such as pericardial tamponade, severe valve failure, pulmonary embolism, and wall motion abnormalities can be detected easily with echocardiography [27].
Vessels: Fluid status: In intensive care fluid administration without guidance some time result in adverse outcome. Volume status assessment requires invasive central venous access for CVP and pulmonary capillary wedge pressure monitoring. It can be done noninvasively and immediately with use of bedside ultrasound. IVC diameter and its variation with respiration in M-mode give an idea of fluid load in right atrium. IVC diameter more than 2 cm in volume overload and variation of 18% in septic shock patients was strongly correlated with preload sensitivity [28]. In spontaneously breathing patient with curvilinear probe in sub-xiphoid space in the long axis scan including liver if shows collapse of inferior vena cava during inspiration suggest fluid responsiveness of patient. Stroke volume variation with respiration and left ventricle end diastolic volume measurement needs more training but gives accurate idea of fluid status in critical care patients.
Ultrasound is also used for assessment of any vessel thrombosis and to rule out deep vein thrombosis.
Intervention
Limited echocardiography guided subacute shock management result in improved 28-day survival, reduced acute kidney injury [29].
Vascular access: Ultrasound imaging guides vascular access in real time. Most commonly used probe for this purpose is linear array probe. A lot of literature proved that use of ultrasound increase success rate, reduces number of attempts and complications. The internal jugular vein, subclavian and femoral vein can be catheterized (Figures 5 and 6). Femoral is less preferred because of infection. Complications of central venous catheterisation are more with inexperienced inserter, difficult patients and abnormal anatomy or co-morbid condition in ICU like coagulopathy. The most common complications of IJV cannulation are arterial puncture and hematoma. The most common complication of subclavian vein cannulation is pneumothorax [30]; it can be detected post procedure with ultrasound better than chest X-ray. Subclavian vein cannulations in critical care patients shown that ultrasound use decrease the access time and complications rates [31]. Subclavian venous catheterization even inexperienced person and failure of landmark technique, ultrasound guidance improves the success rate of catheterisations [32]. Infraclavicular subclavian vein cannulation using micro-convex paediatric probe instead of linear probe appears to be a safe and effective method of placing subclavian vascular catheters [33]. Further study is required in this for better probe for infraclavicular subclavian vein cannulation.

Figure 5: Central venous cannulation using USG.

Figure 6: Central venous cannulation using USG.
For axillary and subclavian vein cannulation using real-time ultrasound guidance have shown lower but same complication rate as internal jugular vein compared with landmark technique, when competent individuals with appropriate training apply it [34]. Femoral vein position in relation to leg position shown that 95%, of people have some degree of overlap of the femoral vein by the femoral artery. Abduction and internal rotation decrease the overlap, increase the size and maximize the chance of cannulation [35]. Ultrasound-guided radial artery catheterization in infants and small children shows more successful than the usual palpation technique [36]. Examination of vessels with ultrasound prior to cannulation for patency. Post cannulation confirmation of cannula within the lumen reduces the complication rate [37].
Ultrasound assisted Cardiopulmonary Resuscitation
Cardiopulmonary resuscitation is done frequently in the ICU setting and can be guided by the use of ultrasound for prediction of successful resuscitation. Causes of cardiac arrest like Ventricular Tachycardia/Ventricular Fibrillation is decreasing trends due to early detection and treatment but pulseless electrical activity and asystole increasing [38]. Various cause of pulseless electrical activity and asystole like severe hypovolemia, tension pneumothorax, cardiac tamponade, and massive pulmonary embolus can be diagnosed and managed under ultrasound guidance easily and quickly. In subxiphoid view placement of the probe just before chest compressions are paused for a planned rhythm assessment enables a well-trained operator to obtain views within few second. Presence of cardiac activity in ultrasound significantly associated with survival and absence with poor prognosis [39].
Ultrasound for Trauma Critical Care Patients
Airway examination in trauma patient diagnose airway trauma as breach in continuity of the air mucosal interface and deviation from normal ultrasound image.
Focused Abdominal Sonography for Trauma in blunt trauma abdomen (FAST) and Extended FAST (EFAST) for associated chest injury reduces the unnecessary CT examination44. FAST detects the free fluid usually blood in the pericardial, pleural, or intraperitoneal spaces. Probe is placed in longitudinal orientation in the second or third intercostal space in the mid-clavicular line for detection of pneumothorax. Subxiphoid space scan for pericardial issue in trauma patient. Hepatorenal and splenorenal, suprapubic spaces scan detect the free fluid in peritoneal cavity (Figure 7). Shifting the probe one rib space in hepatorenal and splenorenal view for evaluation of the area above the diaphragm for detection of free fluid in pleural cavity. If condition of patient is deteriorating and become unstable early repeat eFAST done and should be observed for at least 4 hours. The use of eFAST can decrease time to definitive care.

Figure 7: FAST Scan of Right-side showing liver and kidney.
References
- Cho BC, Kang SM, Kim DH, Ko YG, Choi D, et al. (2004) Clinical and echocardiographic characteristics of pericardial effusion in patients who underwent echocardiographically guided pericardiocentesis: Yonsei Cardiovascular Center experience, 1993-2003. Yonsei Med J 45: 462-468.
- Tsang TS, El-Najdawi EK, Seward JB, Hagler DJ, Freeman WK, et (1998) Percutaneous echocardiographically guided pericardiocentesis in pediatric patients: Evaluation of safety and efficacy. J Am Soc Echocardiogr 11: 10721077.
- Mercaldi CJ, Lanes SF (2013) Ultrasound guidance decreases complications and improves the cost of care among patients undergoing thoracentesis and Chest 143: 532-538.
- Mitra S, Kapoor D, Srivastava M, Sandhu H (2013) Real-time ultrasound guided percutaneous dilatational tracheostomy in critically ill patients: A step towards safety! Indian J Crit Care Med 17: 367-369.
- Ezri T, Gewürtz G, Sessler DI, Medalion B, Szmuk P, et (2003) Prediction of Difficult Laryngoscopy in Obese Patients by Ultrasound Quantification of Anterior Neck Soft Tissue. Anaesthesia 58: 1111-1114.
- Shibasaki M, Nakajima Y, Ishii S, Shimizu F, Shime N, et (2010) Prediction of pediatric endotracheal tube size by ultrasonography. Anesthesiology 113: 819-824.
- Sustić A, Miletić D, Protić A, Ivancić A, Cicvarić T (2008) Can ultrasound be useful for predicting the size of a left double-lumen bronchial tube? Tracheal width as measured by ultrasonography versus computed J Clin Anesth 20: 247-252.
- Ding LW, Wang HC, Wu HD, Chang CJ, Yang PC (2006) Laryngeal ultrasound: A useful method in predicting post-extubation A pilot study. Eur Respir J 27: 384-389.
- Milling TJ, Jones M, Khan T, Tad-y D, Melniker LA, et (2007) Transtracheal 2-d ultrasound for identification of esophageal intubation. J Emerg Med 32: 409-414.
- Sethi A, Nimbalkar A, Patel D, Kungwani A, Nimbalkar S (2014) Point of care ultrasonography for position of tip of endotracheal tube in neonates. Indian Pediatr 51: 119-121.
- Singh M, Chin KJ, Chan VWS, Wong DT, Prasad GA, et (2010) Use of sonography for airway assessment: an observational study. J Ultrasound Med 29: 79-85.
- Holdgaard HO, Pedersen J, Jensen RH, Outzen KE, Midtgaard T, et (1998) Percutaneous dilatational tracheostomy versus conventional surgical tracheostomy. A clinical randomised study. Acta Anaesthesiol Scand 42: 545-550.
- Kristensen MS (2011) Ultrasonography in the management of the Acta Anaesthesiol Scand 55: 1155-1173.
- Lichtenstein DA, Mezière GA (2011) The BLUE-points: three standardized points used in the BLUE-protocol for ultrasound assessment of the lung in acute respiratory failure. Crit Ultrasound J 3:109-110.
- Lichtenstein DA, Mezière GA (2008) Relevance of lung ultrasound in the diagnosis of acute respiratory failure: The BLUE protocol. Chest 134: 117-125.
- Mynarek G, Brabrand K, Jakobsen JA, Kolbenstvedt A (2004) Complications following ultrasound-guided thoracocentesis. Acta Radiol 45: 519-522.
- Lichtenstein D, Mézière G, Biderman P, Gepner A, Barré O (1997) The comet-tail artifact. An ultrasound sign of alveolar-interstitial syndrome. Am J Respir Crit Care Med 156: 1640-1646.
- Lichtenstein D, Goldstein I, Mourgeon E, Cluzel P, Grenier P, et al. (2004) Comparative diagnostic performances of auscultation, chest radiography, and lung ultrasonography in acute respiratory distress syndrome. Anesthesiology 100: 9 -15.
- Alam SR, Docherty A, Mackle I, Gillies MA (2013) The introduction of intensive care-led echocardiography into a tertiary care unit. JICS 14: 15-19.
- Neskovic AN, Hagendorff A, Lancellotti P, Guarracino F, Varga A, et al. (2013) Emergency echocardiography: the European Association of Cardiovascular Imaging recommendations. Eur Heart J Cardiovasc Imaging 14: 1-11.
- Jensen MB, Sloth E, Larsen KM, Schmidt MB (2004) Transthoracic echocardiography for cardiopulmonary monitoring in intensive Eur J Anaesthesiol 21: 700-707.
- Liteplo AS, Murray AF, Kimberly HH, Noble VE (2010) Real-time resolution of sonographic B-lines in a patient with pulmonary edema on continuous positive airway pressure. Am J Emerg Med 28: 541.
- Rich S, Sheikh A, Gallastegui J, Kondos GT, Mason T, et (1982) Determination of left ventricular ejection fraction by visual estimation during real-time two-dimensional echocardiography. Am Heart J 104: 603-606.
- Vieillard-Baron A, Prin S, Chergui K, Dubourg O, Jardin F (2002) Echo-Doppler demonstration of acute cor pulmonale at the bedside in the medical intensive care unit. Am J Respir Crit Care Med 166: 1310-1319.
- Jardin F, Dubourg O, Bourdarias JP (1997) Echocardiographic pattern of acute cor pulmonale. Chest 111: 209-217.
- Vayre F, Lardoux H, Pezzano M, Bourdarias JP, Dubourg O (2000) Subxiphoid pericardiocentesis guided by contrast two-dimensional echocardiography in cardiac tamponade: Experience of 110 consecutive patients. Eur J Echocardiogr 1: 66-71.
- Manasia AR, Nagaraj HM, Kodali RB, Croft LB, Oropello JM, et al. (2005) Feasibility and potential clinical utility of goal-directed transthoracic echocardiography performed by noncardiologist intensivists using a small hand-carried device (SonoHeart) in critically ill patients. J Cardiothorac Vasc Anesth 19: 155-159.
- Barbier C, Loubières Y, Schmit C, Hayon J, Ricôme JL, et al. (2004) Respiratory changes in inferior vena cava diameter are helpful in predicting fluid responsiveness in ventilated septic patients. Intensive Care Med 30: 1740-
- Kanji HD, McCallum J, Sirounis D, MacRedmond R, Moss R, et al. (2014) Limited echocardiography-guided therapy in subacute shock is associated with change in management and improved outcomes. J Crit Care 29: 700-
- McGee DC, Gould MK (2003) Preventing complications of central venous N Engl J Med 348: 1123-1133.
- Fragou M, Gravvanis A, Dimitriou V, Papalois A, Kouraklis G, et (2011) Real-time ultrasound-guided subclavian vein cannulation versus the landmark method in critical care patients: A prospective randomized study. Crit Care Med 39: 1607-1612.
- Gualtieri E, Deppe SA, Sipperly ME, Thompson DR (1995) Subclavian venous catheterization: Greater success rate for less experienced operators using ultrasound guidance. Crit Care Med 23: 692-697.
- Lanspa MJ, Fair J, Hirshberg EL, Grissom CK, Brown SM (2014) Ultrasound-guided subclavian vein cannulation using a micro-convex ultrasound Ann Am Thorac Soc 11: 583-586.
- Mochida T, Seino Y, Matsuda K, Haga M, Yamamoto G (2014) Safety of axillary and subclavian vein cannulation using real-time ultrasound guidance. Masui 63: 57-61.
- Randall C, Schmeiser E, Fiers E, Little A, Dogbey G, et (2014) Ultrasound investigation of leg position to enhance femoral vein exposure for cannulation. J Emerg Med 47: 176-181.
- Ishii S, Shime N, Shibasaki M, Sawa T (2013) Ultrasound-guided radial artery catheterization in infants and small children. Pediatr Crit Care Med 14: 471-473.
- Vezzani A, Brusasco C, Palermo S, Launo C, Mergoni M, et (2010) Ultrasound localization of central vein catheter and detection of postprocedural pneumothorax: an alternative to chest radiography. Crit Care Med 38: 533538.
- Parish DC, Chandra KMD, Dane FC (2003) Success changes the problem: why ventricular fibrillation is declining, why pulseless electrical activity is emerging, and what to do about it. Resuscitation 58: 31-35.
- Salen P, O’Connor R, Sierzenski P, Passarello B, Pancu D, et al. (2001) Can cardiac sonography and capnography be used independently and in combination to predict resuscitation outcomes? Acad Emerg Med 8: 610-615.
Citation: Yadav N, Garg R (2021) Emerging Use of Ultrasound by Intensivist in Intensive Care as Point of Care. J Anes Perio Manag 5: 010.
Copyright: © 2021 Yadav N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.