*Corresponding Author:
Kaihui Sha,
School of Nursing, Binzhou Medical University, School of Nursing, Binzhou, Shandong Province, China
Tel: +86 18654317708
Fax: +86 5433256893
Email: skhui328175@163.com
Abstract
Objective: We used a single group preand post-test design to identify the effects of long-term vigorous walking on sleep quality and physical fitness among perimenopausal women.
Methods: Forty perimenopausal women (mean age 53.6 years, standard deviation 1.13 years) were recruited from a community in Binzhou, China. Participating women performed long-term vigorous walking for 1 year. The Pittsburgh Sleep Quality Index was used to assess their sleep quality before and 1 year after starting the walking program. Participants’ physical fitness was measured at the two time points using response time, grip strength, closed-eyes single-foot standing time, and anterior body flexion distance when sitting.
Result: Compared with pre-exercise, participants’ sleep quality score showed a significant difference post-exercise (p < 0.01). Participants’ reaction time was significantly shortened (p < 0.01), grip strength significantly increased (p < 0.01), and closed-eyes single-foot standing time and anterior flexion distance when sitting were significantly increased (both p < 0.05).
Conclusion: Long-term vigorous walking can improve sleep quality and physical fitness among perimenopausal women, and may promote physical and mental health older adults.
Keywords
Long-term; Perimenopausal women; Physical fitness; Sleep quality; Vigorous walking
Introduction
Menopause usually starts around age 50 years, and is accompanied by permanent cessation of ovarian function [1]. About three-quarters of women complain of hot flushes, night sweats, fatigue, pain, loss of libido, and mood changes during menopause [2]. These symptoms tend to persist for years after menopause and may have a significant impact on women’s quality of life [1,3,4]. In addition, menopause is known to be associated with some psychological dysfunction. For many women, menopause is also associated with sleep difficulties and changes in physical health, weight, and psychosomatic condition (including stress and emotional state, self-confidence, work, ability to make decisions, and ability to concentrate), but not in personal life (family life, time spent with self, hobbies, and interests)[5].
The natural process of human aging leads to important organ changes that ultimately cause mental and physical changes, and affect the quality of life of older adults [6-8]. Sleep disorders are among the major health problems commonly observed among older adults; morbidity increases with age, and more than 50% of older adults complain about the quality of their sleep [9]. For this group, medication remains the most common treatment for sleep disorders [10]. However, frequent use of sleeping medication has been observed to alter sleep pat- terns in older people, and is associated with several adverse reactions, such as sedation, excessive daytime sleepiness, increased risk for falls, and increased drug dependence. Therefore, alternative strategies are needed to improve the quality of sleep among older adults.Physical exercise at mild to moderate intensity has a positive impact on the quality of sleep in older people, and is recommended as a non-pharmacological intervention for prevention and treatment of sleep problems in this group [11,12]. Decline in physical fitness can also cause older people to fall and slow down, leading to accidents. Therefore, it is important to improve sleep quality and physical fitness among older adults.
Aerobic exercise is thought to reduce anxiety, boost self-esteem, improve stress response, and reduce depression among postmenopausal women [5]. However, despite evidence that physical exercise is good for health and quality of life, older people rarely adhere to this method [13]. Walking is described as a “near perfect exercise” and is considered the most popular sport. Although less than 50% of people persist with many forms of exercise, walking tends to achieve greater compliance than other exercise types [14]. Positive effects of shortterm walking interventions on weight loss and changes in body composition have been demonstrated. Weight loss improves gait, walking speed, and balance control, thereby reducing the risk of falling and fractures [15]. A study by Stattin et al. [16] showed that walking reduces the incidence of all fractures, especially hip fractures, in men and women of all age groups. This study aimed to investigate the effect of long-term walking exercise on sleep quality and physical fitness among perimenopausal women.
Methods
Design and participants
We used a single group preand post-test design to evaluate the effects of long-term walking exercise on sleep quality and physical fitness among women during menopause. Participants were 40 community-based perimenopausal women with a mean (standard deviation [SD]) age of 53.6 (1.13) years who volunteered to participate in this study from Binzhou, China. Thirteen of these 40 women were retired and 16 were in post-menopause. Inclusion criteria were: 1) women aged 45-60 years; 2) with good physical strength and capable of moderate or above intensity of sports; 3) who could read and understand Chinese; 4) would be living in the community under study for at least 1 year; and 5) that volunteered to participate in this study. Exclusion criteria were: 1) women with serious diseases, such as malignant tumor, renal failure, heart failure, and hypertension; 2) with other diseases that affect exercise, such as diabetes and fractures; and 3) using drugs that affect the quality of sleep currently or in the past 2 weeks.
Exercise method
During the 1-year study period, participants maintained a 1-hour vigorous walk every day. Participants were instructed to walk vigorously but carefully, with a straight spine, upright chest, high head, firm abdomen, relaxed shoulder, and a firm and strong step. They were also advised that each walk should be of equal distance and at a uniform speed, and they should be aware of their breathing, look into the distance, and allow their arms to swing rhythmically back and forth. Participants should walk with ease and pleasure, but aim to get slightly sweaty or sweaty and raise their heart rate. The mode of exercise is described in (Table 1). All participants were asked to complete a daily evaluation diary of walking performance, including the date, number of steps, and time of that day’s walk. Through this diary, the present researchers could confirm whether participants completed walking exercise and had mastered the method, and could then provide necessary supervision and guidance.
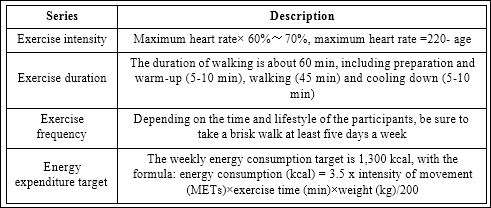
Table 1: Mode of exercise.
Evaluating sleep quality
We used the Pittsburgh Sleep Quality Index (PSQI) [17] to assess quality of sleep. This is a validated scale for assessing the quality of sleep and is applicable for various groups. The PSQI contains 19 items and provides seven component scores for subjective sleep quality, sleep latency, duration, habitual sleep efficiency, sleep disturbance, sleep medication, and daytime dysfunction [18,19]. In addition, the PSQI gives a total score for overall quality of sleep [20,21] ranging from 0-21; a higher score indicates worse sleep quality. The scale has been validated in different populations (with Cronbach’s alpha 0.8) and is considered an effective screening tool 17. The PSQI was administered to all participants before starting the walking program and 1 year after starting walking exercise.
Testing physical fitness
The physical fitness test was designed to effectively evaluate older adults’ abilities to physically perform activities of daily living, and is commonly used to evaluate their functional fitness [22]. Response time was used to evaluate participants’ sensitivity to a stimulus and grip strength was used to measure muscle strength. Balance was measured by testing one-leg standing time with closed eyes. Flexibility was assessed by measuring the distance of anterior flexion of the body when participants were sitting. We tested these variables for all participants before and 1 year after starting the walking exercise program. All indicators were tested in accordance with the requirements of the Manual of Physical Fitness Standards for Adults in China.
Statistical analyses
Data were analyzed using SPSS version 21.0. Data were expressed as mean (SD), and paired t-tests were performed before and after the intervention. The level of statistical significance was set at p < 0.05.
Result
Effects of vigorous walking on sleep quality among perimenopausal women
Table 2 shows the mean (SD) scores for sleep variables preand post-intervention. The mean PSQI score was 9.85 (1.24) before exercise and 4.76 (0.41) after exercise, and the difference was significant (p < 0.01, t=1.572). The score for all PSQI items (excluding sleep medication) before and after exercise was also significantly different (p < 0.01). This analysis indicated that long-term walking improved sleep quality.
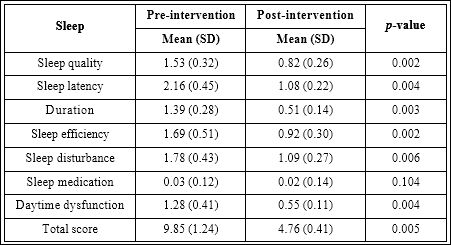
Table 2: Sleep quality preand post-intervention.
SD= standard deviation.
Effects of vigorous walking on physical fitness among perimenopausal women
Table 3 shows that after 1 year of walking exercise, participants had significantly shorter response time (p < 0.01), significantly increased grip strength (p < 0.01), significantly longer one-leg standing time with closed eyes (p < 0.05), and significantly increased body anterior flexion distance when sitting (p < 0.05). These results indicated that long-term walking can improve physical fitness among menopausal women.
Discussion
Long-term walking exercise improves sleep quality among perimenopausal women
Adults and older adults that engage in more physical activity have better sleep quality and a healthier quality of life that those that perform less exercise [23,24]. We found that 1 year of vigorous walking had a positive effect on sleep quality among perimenopausal women. This finding was congruent with a study by Bonardi et al. [25] that found aerobic exercise can reduce sleep fragmentation index and improve sleep efficacy and quality. The decrease in sleep latency, longer sleep duration, and a marked increase in sleep quality and efficiency may be attributable to relief of mental stress, diversion of focus excitation, and the promotion of sleep. In addition, moderate exercise consumes a certain amount of energy. In response, the body accelerates sleep through active compensatory mechanisms that increase sleep depth and promote physical recovery.
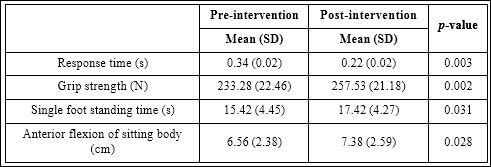
Table 3: Physical fitness preand post-intervention.
SD= standard deviation.
There was no difference in sleep medication use before and after exercise among our participants, mainly because most of the perimenopausal women in this study did not need drugs to sleep. Brandao et al. found that sleep disorders can cause mental disorders (e.g., anxiety and depression), and the rates of these disorders are significantly higher in people with sleep disorders than those without [9]. In turn, mental disorders can lead to decreased sleep quality, and depression and anxiety have a more pronounced effect on sleep disorders among older people. While the kind of aerobic exercise (e.g., walking) has a positive effect of regulating mood, it can also improve the quality of sleep and reduce bad moods, therefore promoting the mental and physical health among older adults.
Long-term walking exercise improves physical fitness among perimenopausal women
Physical fitness indicators include response time, grip power, closed-eyes single-foot standing time, and anterior body flexion distance when sitting. Consistent with the findings of Gaba et al. [15], we showed that vigorous walking had a positive effect on postural stability in perimenopausal women aged over 50 years with sedentary occupations. Response time reflects the body’s ability to respond to unexpected events and stimuli. This is largely controlled by the brain; exercise can increase blood flow to the brain, making the brain more responsive. Grip strength reflects the strength of upper limb muscles, and vigorous walking with constantly swinging upper limbs can fully exercise upper limb muscle groups, thicken muscle fibers, and increase strength. Handgrip strength is a rapid, simple, and noninvasive method to measure muscle fitness [26]. Handgrip is a sign of an individual’s overall strength, and also provides an indication of muscle mass, body function, nutritional status, and general health [27]. Single-foot standing time with closed eyes reflects the body’s balance ability [28]. The decrease in the balance ability of older adults is mainly due to decreases of joint muscle coordination and muscle strength, and insufficient blood supply to brain tissue and vestibular organs [28]. During walking (particularly over a long period), all lower limbs are involved in the movement. This enhances coordination, increases muscle strength, and improves the blood oxygen supply to brain tissue and vestibular organs. These improvements result in improved balance ability. Finally, the anterior flexion distance reflects the flexibility of the hip joint 28. As age increases, flexibility decreases because of degeneration of joints and decline of ligament elasticity. Vigorous walking repeatedly bends the hips and knees, which increases the activity of the hip and knee joints. In addition, long-term adherence to exercise can prevent the rapid loss of bone calcium, and help to improve the flexibility of older adults.
This study had some limitations. First, the use of a singlegroup preand post-test design lowered the statistical power.Furthermore, this study had a small sample size and lacked a control group. Therefore, a randomized controlled trialwith a larger sample is needed in future studies.
Implications for future research
Although this study had limitations, it offers promising evidence regarding the effect of vigorous walking on sleep quality and physical fitness among perimenopausal women. Furthermore, vigorous walking is a widely accepted form of exercise by both men and women. Therefore, people may readily engage in walking exercise and improve their sleep quality and physical fitness. We recommend testing the enduring effects of vigorous walking on sleep quality and physical fitness by conducting studies with long-term follow-up periods.
Conclusion
This study shows that the long-term walking exercise improves sleep and physical fitnessamong perimenopausal women. Because a walking intervention is simple and easy to implement, it can be used with older adult populations.However, our use of a single group preand post-test design lowered the statistical power of this study. A control group is recommended in future research. More studies are needed to confirm the effectiveness of long-term walking exercise among this population.
Acknowledgement
We thank Audrey Holmes, MA, from LiwenBianji, Edanz Group China (www.liwenbianji.cn/ac), for editing the English text of a draft of this manuscript.
References
- Cramer H, Peng W, Lauche R (2019) Yoga for menopausal symptoms-A systematic review and meta-analysis. Maturitas 109: 13-25.
- Daley A, Stokes-Lampard H, Thomas A, MacArthur C (2014) Exercise for vasomotor menopausal Cochrane Database of Systematic Reviews 4: CD006108.
- Davis SR, Lambrinoudaki I, Lumsden M, Gita DM, Lubna P, et al. (2015) Nature reviews Disease primers. Nat Rev Dis Primers 1: 15004.
- Monteleone P, Mascagni G, Giannini A, Monteleone P, Mascagni G, et al. (2018) Symptoms of menopause global prevalence, physiology and impli Nat Rev Endocrinol 14: 199-215.
- Garnier S, Gaubert I, Joffroy S, Auneau G, Mauriège P (2019) Impact of brisk walking on perceived health evaluated by a novel short questionnaire in sedentary and moderately obese postmenopausal women. Menopause 20: 804-812.
- Løppenthin K, Esbensen BA, Jennum P, Østergaard M, Christensen JF, et (2014) Effect of intermittent aerobic exercise on sleep quality and sleep disturbances in patients with rheumatoid arthritis–design of a randomized controlled trial. BMC Musculoskelet Disord 15: 49.
- Durcan L, Wilson F, Cunnane G (2014) The effect of exercise on sleep and fatigue in rheumatoid arthritis: a randomized controlled study. J Rheumatol 41: 1966-1973.
- Conte F, Arzilli C, Errico BM, Giganti F, Iovino D, et al. (2014) Sleep measures expressing ‘functional uncertainty’ in elderlies’ sleep. Gerontology 60: 448-457.
- Brandao GS, Gomes G, Brandao GS,CallouSampaio AA, Donner CF, et al. (2018) Home exercise improves the quality of sleep and daytime sleepiness of elderlies: A randomized controlled Multidiscip Respir Med 13: 2.
- Markota M, Rummans TA, Bostwick JM, Lapid MI (2016) Benzodiazepine Use in Older Adults: Dangers, Management, and Alternative Mayo ClinProc 91: 1632-1639.
- Akbari Kamrani AA, Shams A, Shamsipour Dehkordi P, Mohajeri R (1969) The effect of low and moderate intensity aerobic exercises on sleep quality in men older adults. Pakistan Journal of Medical Sciences. Pak J Med Sci 30: 417-421.
- Du S, Dong J, Zhang H, Jin S, Xu G, et (2015) Taichi exercise for self-rated sleep quality in older people: a systematic review and meta-analysis. Int J Nurs Stud 52: 368-379.
- Gobbi S, Sebastiao E, Papini CB, Nakamura PM, Netto AV, et (2012) Physical inactivity and related barriers: a study in a community dwelling of older brazilians. J Aging Res 2012: 685190.
- Kearney TM, Murphy MH, Davison GW, O’Kane MJ, Gallagher AM. (2014) Accumulated brisk walking reduces arterial stiffness in overweight adults: evidence from a randomized control J Am Soc Hypertens 8: 117-126.
- Gaba A, Cuberek R, Svoboda Z, Chmelík F, Pelclová J, et al. (2016) The effect of brisk walking on postural stability, bone mineral density, body weight and composition in women over 50 years with a sedentary occupation: a randomized controlled BMC Womens Health 16: 63.
- Stattin K, Michaëlsson K, Larsson SC, Wolk A, Byberg L (2017) Leisure-Time Physical Activity and Risk of Fracture: A Cohort Study of 66,940 Men and J Bone Miner Res 32: 1599-1606.
- Mollayeva T, Thurairajah P, Burton K, Mollayeva S, Shapiro CM, et (2016) The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non-clinical samples: A systematic review and meta-analysis. Sleep Med Rev 25: 52-73.
- Nishiyama T, Mizuno T, Kojima M, Suzuki S, Kitajima T, et al. (2014) Criterion validity of the Pittsburgh Sleep Quality Index and Epworth Sleepiness Scale for the diagnosis of sleep disorders. Sleep med 15: 422-429.
- Rshikesan PB, Subramanya P, Singh D (2017) Sleep Quality and Body Com- position Variations in Obese Male Adults after 14 Weeks of Yoga Intervention: A Randomized Controlled Int J Yoga 10: 128-137.
- Hinz A, Glaesmer H, Brahler E, Löffler M, Engel C, et al. (2017) Sleep quality in the general population: psychometric properties of the Pittsburgh Sleep Quality Index, derived from a German community sample of 9284 people. Sleep med 30: 57-63.
- Del Rio Joao KA, Becker NB, de Neves Jesus S, Isabel Santos Martins R (2017) Validation of the Portuguese version of the Pittsburgh Sleep Quality Index (PSQI-PT). Psychiatry Res 247: 225-229.
- Chang SF, Lin PC, Yang RS, Yang RJ (2018) The preliminary effect of whole- body vibration intervention on improving the skeletal muscle mass index, physical fitness, and quality of life among older people with BMC Geriatr 18: 17.
- American College of Sports M (2009) American College of Sports Medicine position stand. Progression models in resistance training for healthy adults. Medicine and science in sports and exercise. Med Sci Sports Exerc 41: 687-708.
- Williams DM, Matthews CE, Rutt C, Melissa AN, Bess HM (2008) Interven- tions to increase walking Med Sci Sports Exerc 40: 567-573.
- Bonardi JMT, Lima LG, Campos GO, Bertani RF, Moriguti JC, et al. (2016) Effect of different types of exercise on sleep quality of elderly Sleep Med 25: 122-129.
- Chung HS, Shin MH, Park K (2018) Association between hand-grip strength and erectile dysfunction in older Aging Male 21: 225-230.
- Bohannon RW (2015) Muscle strength: clinical and prognostic value of hand- grip Curr Opin Clin Nutr Metab Care 18: 465-470.
- Sha K, Liu T, Zhang X (2008) The influence of Tai Chi exercise on physical fitness of the Chinese Journal of Rehabilitation 23: 323-324.
Citation: Sha K, Liu T (2019) Effects of Long-Term Vigorous Walking on Sleep Qual- ity and Physical Fitness among Perimenopausal Women. J Acupun Tradit Med 3: 004.
Copyright: © 2019 Sha K and Liu T. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.