*Corresponding Author:
Robert Mutagwanya,
School of Food Technology, Nutrition and Bioengineering, Makerere University, Uganda
Tel: +256392944426/+256701245160
E-mail: robertmutagwanya@gmail.com
Abstract
Background: Nutrition knowledge practice, medication and physical exercises are the three cornerstones of diabetes management. This is because diabetic patients have a major role in the control and treatment of type 2 diabetes. This study therefore aimed at assessing the effect of nutrition education on the knowledge level and physical activity duration among type 2 diabetic patients.
Methodology: One hundred type 2 diabetic patients were randomly selected and divided into two groups of intervention and control (50 patients in each group) to participate in the study. The intervention consisted of two educational sessions each for 30 minutes twice a week. Data were collected using a pre-tested questionnaire (22 questions) before and after intervention every after one month for a period of four months of intervention. Data was entered and analyzed using SPSS software version 21.
Results: The average age of patients was 48 years. Most of the patients were females (65.39%) compared to males (34.01%). Results further revealed that 41.34% of the patients’ duration of diabetes was between 5-10 years; 32.84% had diabetes less than 5 years, and only 18.63% had diabetes 11-15 years while 7.19% had diabetes for more than 15 years. There was a significant (p<0.001) increase in knowledge scores (41.26 ± 8.85% to 84.02 ± 5.84%) and duration of physical exercises (0.03 ± 0.17 to 17.20 ± 14.61 minutes) in the intervention group compared to the control group.
Conclusion: Nutrition education significantly improves diabetes nutrition knowledge and duration of physical activity among type 2 diabetes patients.
Keywords
Nutrition education; Physical activity; Type 2 diabetes mellitus
Introduction
Diabetes is a heterogeneous group of metabolic diseases characterized by either insulin resistance or insulin insufficiency. Diabetes mellitus is one of the non-communicable diseases that is on the rise globally [1]. The incidence is of alarming concern to health care providers with the main burden of this disease also affecting all developing countries. The number of diabetic patients is estimated to reach 300 million by the end of 2025 with dramatic and significant impacts mostly experienced in developing countries [2]. Prevalence of diabetes mellitus in adults stands at 463 million people globally, 3.9% in Africa and 1.6% in Uganda [3]. Type 2 diabetes is a chronic condition that develops when the body becomes resistant to insulin. It should be noted that the exact cause of insulin resistance or failure of pancreas to produce enough insulin is unknown, although genetics like family history, fat distribution, race or ethnicity and environmental factors, such as being overweight and inactive, are the contributing factors. The long-term complications of type 2 diabetes are diabetic retinopathy, kidney disease (nephropathy), diabetic neuropathy, diabetic foot and macrovascular problems.
Type 2 diabetes used to be known as adult-onset diabetes, but today more children are being diagnosed with the disorder, probably due to the rise in childhood obesity. There’s no cure for type 2 diabetes, but losing weight, eating well and exercising can help manage the disease. If diet and exercise aren’t enough to manage blood sugar well, there is need for diabetes medications or insulin therapy. In the management of type 2 diabetes, Diet, physical activity and medication are the three cornerstones. However, many diabetes patients in Uganda have less dietary knowledge, attitude and practice towards the importance of dietary management care [4,5]. Dietary knowledge among diabetes type 2 patients is a significant factor to improve the dietary pattern, hyperglycemia and the dyslipidemia. Therefore, acquisition of nutrition and physical activity knowledge is vital in changing the unfavorable dietary pattern and sedentary life style among the diabetes patients [6]. With nutrition knowledge and positive attitude towards dietary management, diabetes patients may control their blood sugar [7,8]. In addition, following proper practices to the recommended diet by expert dietician and physical exercises by health workers are important in preventing further complications of diabetes [9]. According to Gray and Threlkeld [10], emphasis on the proper dietary food choices, physical exercises, attitude and practices among diabetes patients is important in improving the maximum level of dietary knowledge, attitude and practices. In the health care settings, poor dietary knowledge, attitudes and practices among diabetes have effects on patients’ care [11]. Type 2 diabetes patients’ lifestyle changes regarding dietary pattern, attitude, knowledge and practices are vital in the control and management of type 2 diabetes. Therefore, understanding the risk factors is an effective way for managing type 2 diabetes. The American Diabetes Association (ADA) recommends that patients who are diagnosed and are suffering from diabetes need to be aware of their nutrition requirement, that is the carbohydrates intake should be 45 to 65% of daily total calorie; fats 25 to 35%. Protein should be 12 -20% of daily calories although there may be some differences depending on the status of the patient’s health [12]. Dietary knowledge is a vital perspective that assumes a major part of dietary information by developing the awareness and ultimately the health of the public. Knowledge regarding healthy diet and food safety can be a predisposing factor for enhancing the dietary patterns, habits and for adopting eating routines among patients with diabetes [13]. The knowledge, attitude and practice must be considered with a specific end goal to advance the society well-being. The aim of this study was to identify the effect of diabetes nutrition education on the level of dietary knowledge and duration of physical exercises among type 2 diabetes patients.
Materials and Methods
Study area, design and population
A longitudinal cohort non blinded intervention study was conducted for five months that is from March to July. In this study, 100 type 2 diabetes out-patients attending Endocrine unit of Mulago National referral and teaching Hospital, Kampala were randomly selected by requesting patients to pick a folded piece of paper written on either ‘’I’ ’for intervention or ‘’C’’ for control group. Patients were then divided into two groups of intervention and control (50 patients in each group). To control potential confounding factors, the two groups were matched. Although, only 34 and 18 of the 50 patients in the intervention and control group respectively completed the study. More females than males participated in the study due to the fact that females easily respond to health practices and other development related activities or programs. Inclusion criteria included; having type 2 diabetes, aged at least 18 years, attending the diabetic clinic, able and willing to perform physical activity for atleast 30 minutes daily during the study period. Those excluded from the study included; very ill type 2 diabetes patients, type 1 diabetes patients, type 2 diabetes patients who were not willing to perform physical activity, and all pregnant diabetic patients. Those patients who were not willing to participate or continue the study were also excluded. The intervention group received nutrition education geared towards promoting dietary diversity, change in the feeding practices, health lifestyle like physical activity, abstinence from alcohol and smoking in addition to the usual care (medication and some rudimental teaching about the dos and don’ts of diabetes) that was provided in the diabetes clinic. A health belief model was used in this nutrition education and the learning segments included; (i) Foods available in Uganda and classification of these foods into food groups according to FAO, 2008. (ii) Recommended foods and non-recommended foods for consumption by the type 2 Diabetic persons, (iii) Food preparation and cooking methods of foods for type 2 Diabetic patients, (iv) Fruits and preparation of fruit juices for consumption by the type 2 Diabetic patients, (v) Meal calculation to meet a glycemic load of 50 (fifty) and food choices, (vi) Special Nutraceutical foods that improve insulin sensitivity among type 2 diabetic persons, (vii) Physical activity performance by diabetic patients, (viii) Foods with a zero glycemic index that should be eaten sparingly (ix) Meal planning using food servings for type 2 diabetics in addition to calculation of the glycemic load. The nutrition education was also based on the nutritional recommendations of the world health organization and American Diabetes Association (ADA) [12]. The intervention consisted of two educational sessions, each 30 minutes twice a week. Data were collected using a questionnaire with 22 questions in four sections including demographic data, nutritional knowledge. Anthropometric data (height, weight and BMI) were also determined and recorded on the similar questionnaire. The questionnaire was completed before and after intervention by both groups.
Sample size determination
The endocrine unit receives about 500 clients in one month. The statistical equation by Dell [14] was modified and used to calculate the number of patients who were recruited in the study.
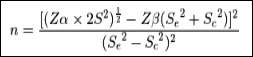
Where:
n=Sample size for each group
Zα=Z-value for type I error (e.g.1.96 at 5% level)
Zβ=Z-value for type II error (e.g. 0.84 at 20% level)
Se=Variance estimate of outcome for intervention group receiving nu- trition education to promote dietary diversity in addition to the usual care given in the endocrine unit.
Sc=Variance estimate of outcome for control group having only the usual care given in the endocrine unit without the nutrition edu- cation promoting dietary diversity.
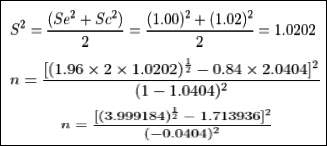
That is n=50 participants
Total population size that was included in the study was 2n=2x50=100 participants/ patients.
That is 50 patients were randomly recruited as controls while 50 were also randomly recruited as intervention group. The participants who completed the study were 34 of the 50 patients in the intervention group and 18 of the 50 patients in the control group.
Determination of nutrition knowledge level of type 2 diabetic patients
Baseline nutrition knowledge of the type 2 diabetic patients
Assessment of baseline nutrition knowledge level regarding their diet and lifestyle was performed by administering an oral nutrition examination for nutrition knowledge. This was done to each of the participants in the control and intervention group and scores at base- line were recorded and computed as percentages. Aspects asked in the examination included whether patients knew preferred foods for di- abetics, non-preferred foods, foods that should be frequently eaten, foods with nutraceutical values, frequency of physical exercises per week. Mean values of nutrition knowledge score were calculated by adding each individual’s nutrition knowledge score divided by total number of patients in the group.
Nutrition knowledge after nutrition education intervention through participatory learning
Only patients in the inclusion group received the nutrition education intervention. A conversation map for type 2 diabetic patients by Healthy interactions [15] was used to help patients get to know of risk factors for diabetes, management of the disease, feeding practices, healthy foods and non-healthy foods and best lifestyle practices and learnt to share information amongst themselves. Nutrition education was also performed using a food pyramid, face to face power point presentations, food preparation videos and live cooking and physical activity demonstrations. During the nutrition education sessions, information collected from key informant interview regarding foods eaten at baseline was classified into the following categories: low glycemic index foods, medium glycemic index foods, high glycemic index foods, and low fat foods, medium fat foods and high fat foods.
Oral examination of knowledge grasp at end of study period, scor- ing and analysis of results
An oral examination was administered at the end of the study period and percentages scores for each of the participants in the control and intervention group were computed as percentages. The oral examination was administered to one individual at a time to avoid any confusion. Mean values of nutrition knowledge score were calculated by adding each individual’s nutrition knowledge score divided by total number of patients in the group.
Nutrition education theories used in this study
The nutrition education that helped to change the knowledge, attitude and behavior of diabetic patients towards dietary diversity, lifestyle and feeding practices was based on one theory, the Health Belief Model (HBM) by Naghashpour [16] which hypothesizes that health-related action depends on sufficient motivation (benefits) to make health issue relevant to consumer, belief that one is susceptible to the health issue (perceived threat), belief that following a specified health recommendation would be useful in reducing or eliminating the perceived threat at an agreeable cost. This theory was used to inform type 2 diabetic patients that following all the nutrition recommendations like diverse diet, observing the glycemic load limit of 50 per day for diabetics, taking in water abundantly, performing physical activity would help reduce complications of diabetes.
Quality control of collected data and ethical approval
Quality control of collected data
Patients were asked similar questions many times to check for consistency when it came to the key informant interviews. Abrupt community visits were performed to check the filling of dietary diversity score sheets versus real food eaten and following of recommended lifestyle.
Ethical approval and informed consent
The research was approved by the Research and Ethics committee of Mulago Hospital and Institutional Review Board of Mulago hospital (Protocol MREC 113). Written informed consent was obtained from all study participants.
Statistical analysis
Data were analyzed using SPSS (version 21). Student’s t test was used to compare the values between the two groups before and after intervention. The mean differences of variables were compared by paired t-test and p-values less than 0.05 were considered significant.
Results
Social demographic characteristics of type 2 diabetic patients
Table 1 shows results of socio-demographic characteristics of type 2 diabetic who participated in the study. The average age of patients was 48 (40-51) years. Most of the patients were females (65.39%), compared to males (34.01%). On average, 22.88% of the patients were married. Findings also showed that 48.37% of patients were self- employed while only 8.50% were unemployed. In addition, 28.60% of patients had tertiary education while 4.25% had pre-primary education.
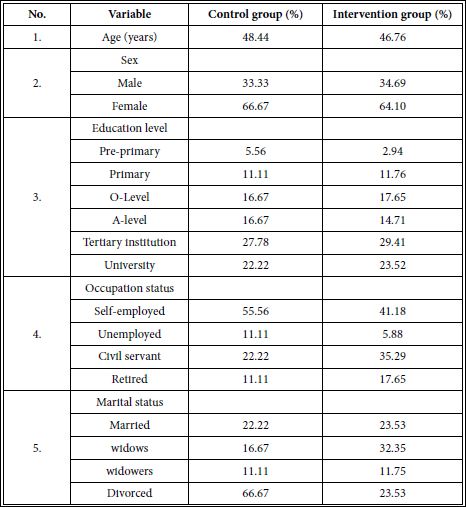
Table 1: Demographic characteristics of diabetic patients in the intervention (n=34) and control groups (n=18).
Risk factor profile of diabetic patients in the case and control groups
Results of risk factor profile of diabetic patients are presented in Table 2. Exactly 40.83% of patients had knowledge regarding diabetes. Results further revealed that 41.34% of the patients’ duration of diabe- tes was between 5-10 years; around one third of the patients (32.84%) had diabetes less than 5 years, and only 18.63% had diabetes 11-15 years while 7.19% had diabetes for more than 15 years. The family his- tory of diabetes was positive in 19.44% of the patients. The majority of patients were non-smokers (94.45%) while smokers were 5.56%. The average BMI of patients was 27.50 kgm-2.
Nutrition knowledge among type 2 diabetes before and after intervention in the intervention and control groups
Percentages of correct answers for each knowledge category are presented in Table 3. Results indicated that; at baseline, half (50%) of the patients were able to identify the kind of spices that must be put in food daily for patients with diabetes. On the other hand, only 45% of patients were able to identify the type of fruits which must be eaten per day by diabetic patients and the method of preparation. At baseline, none (0%) of the patients were able to answer correctly the type of vegetables with a nutraceutical value that must not miss on their daily menus and the frequency of their meals. However, at the end of the intervention, the intervention group showed a significant improvement (P <0.001) from 41.26 to 84.02% in their knowledge regarding foods and food preparation compared to the control group which had no significant change (P= 0.311) that is from 40.72% and 41.26 %.
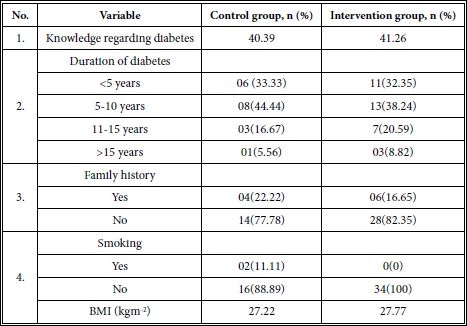
Table 2: Risk factor profile of diabetic patients in the case (n=34) and control (n=18) groups.
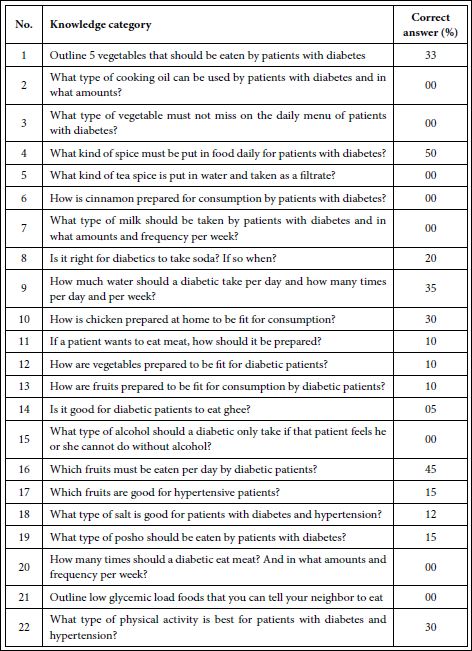
Table 3: Correct responses for dietary knowledge of type 2 diabetic patients per knowl- edge category by 52 patients at baseline.
Scores for nutrition knowledge and physical exercises among type 2 diabetes patients
The scores for nutrition knowledge among type 2 diabetes patients before and after intervention in the intervention and control groups are presented in Table 4. Findings indicated that nutrition knowledge at baseline was 40.72% and 41.26 % for control and intervention groups respectively. Results further revealed that there was a significant increase in diabetes knowledge score among the intervention group patients from 41.26 to 84.02%. On the other hand, the physical activity duration significantly increased from 1.7 to 10 minutes per day in the control group and 0.03 to 17.20 minutes in the intervention group.
Discussion
The average age of patients was 48 years and 28.60% of patients had tertiary education while 4.25% had pre-primary education. Therefore, level of formal education of patients with type 2 diabetes strongly influenced the assimilation of information provided in this study. Age was also strongly associated with how much information patient was able to grasp and remember. Continuous education on recommended dietary practices was noted as important.
The results of this study showed that nutrition education significantly increased the nutrition knowledge and duration physical exercises among type 2 diabetes patients. The intervention group showed a significantly higher (p<0.001) level of nutrition knowledge and improvement in the time spent doing physical exercises than the control group at the end of the study. Since the importance of education depends upon its behavioral impact [16], the Health Belief Model (HBM) was used for increasing the impact of nutrition education in this study. Thus following the nutrition recommendations that were employed in this study helped improve the outcomes which would also eventually result in improved treatment outcomes of type 2 diabetes. Similar studies by Kumari [17] in India; Oosthuizen [18] also revealed that nutrition counseling improved significantly the mean score of nutrition knowledge among diabetic patients. There is no study that has reported results different from the above studies. Therefore, equipping patients with nutrition knowledge is important in diabetes management because patients have a major role in self- control and treatment of type 2 diabetes, so knowledge of different aspects of the disease especially diet therapy is very important.
Findings from this study indicated that type 2 diabetics had poor dietary knowledge and knowledge related to diabetic diet (<50%) as reported in Table 3. A study conducted in Iran [19] reported that type 2 diabetics had average knowledge regarding dietary management while that reported by Sami [20] in Kingdom of Saudi Arabia (28.57%) is as poor as that observed in this study.
In addition, nutrition education significantly increased the level of physical activity. Physical activity in this study it included all movements that increased energy use, whereas exercise was planned, structured physical activity. In this study walking 30 minutes daily was considered as the only acceptable physical activity and if any one decided to go to gym that was not counted as physical activity fit for patients with type 2 diabetes. Walking was considered because it relied on the principal that when one walks he or she burns the fat and when somebody runs, glucose and phosphocreatine are burnt in the muscles and joints [21] and yet these highly need the glucose and phosphocreatine in their muscles and joints in order to be active and flexible given the fact that these patients have insulin resistance.
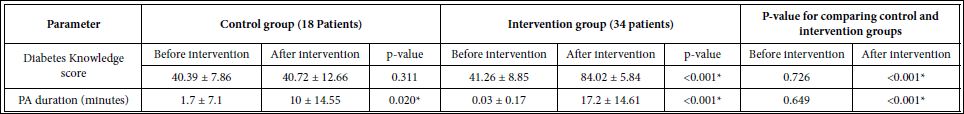
Table 4: Mean ± standard deviations of the nutrition knowledge score (%) and physical activity (PA) duration in type 2 diabetes before and after intervention in the intervention and control groups.
*Significantly different between intervention and control group at p<0.05.
Among diabetics, fat accumulation is a more serious problem than high blood sugar because it causes atherosclerosis resulting in escalating blood pressures, more fatty degeneration of organs like the liver to worsen insulin resistance so when a patient walks the fat is burnt to help control the above complications of type 2 diabetes. In this study, the intervention group that received the nutrition education understood it clearly that physical activity is done regularly and that nutrition is incomplete without physical activity. Fat tissue reduction is an essential component of the successful management of type 2 diabetes. Studies have shown that people who exercise have a higher reduction in fatty tissue than those who only follow a diet. Among Type 2 diabetes patients whose insulin is resistant, walking makes their insulin more effective because the beta cells become active and use the glucose more effectively. Exercise improves blood glucose control in type 2 diabetes, reduces cardiovascular risk factors, contributes to weight loss, and improves well-being. Exercising can also help people with type 2 diabetes to avoid long-term complications, especially heart problems by burning visceral fat. The significant (p<0.001) increase in the physical activity levels among the intervention group was probably due to understanding the benefits of exercise. The effort of adequate intensity - low or moderate - promotes fat burning and weight loss [22]. Also, glucose control is improved, tissue insulin sensitivity is increased, and HbA1c levels in the blood is decreased Due to glucose metabolism, more glucose was increasingly pumped into the muscle cells and joints as a result of reduction in insulin resistance following burning of fats during walking. A study done in Hathras City, India [23] showed that nutrition education significantly increased physical activity performance by obese females.
Conclusions
Type 2 diabetics patients have an overall inadequate dietary knowledge filled with superstitions and perform less physical activity. The results of this study showed that a nutrition education program based on HBM had positive impact on the knowledge level and physical activity duration of type 2 diabetes patients. Therefore, a proper diet and increased physical activity are effective in the prevention and treatment of insulin resistance and pre-diabetes, which usually prevents the development of the disease. HBM-based strategies can be recommended as effective communication channels to improve dietary knowledge and physical activity among diabetes patients.
Source of Funding
This study was funded by Carnegie Corporation of New York.
Acknowledgement
The authors extend their heartfelt appreciation to the diabetes patients who visited Endocrine unit of Mulago hospital for their participation in this study and the staff for their support.
References
- Demilew YM, Firew BS (2019) Factors associated with non-communicable disease among adults in Mecha district, Ethiopia: A case control study. PloS one 14.
- Kimutai SC (2020) Association between Nutrition Knowledge on Diabetes and Dietary Practice of People Living with Diabetes Mellitus in Nandi County. Acta Scientific Nutritional Health 47: 18-27.
- Saeedi P, Salpea P, Karuranga S, Petersohn I, Malanda B, et al. (2020) Mortality attributable to diabetes in 20-79 years old adults, 2019 estimates: Results from the International Diabetes Federation Diabetes Atlas. Diabetes research and clinical practice 108086.
- Kyokunzire C, Matovu N (2018) Factors associated with adherence to diabetes care recommendations among children and adolescents with type 1 diabetes: A facility-based study in two urban diabetes clinics in Diabetes metabolic syndrome and obesity 11: 93-104.
- Ojo TT, Hawley NL, Desai MM, Akiteng AR, Guwatudde D, et al. (2017) Exploring knowledge and attitudes toward non-communicable diseases among village health teams in Eastern Uganda: A cross-sectional study. BMC public health 17: 947.
- Udogadi NS, Onyenibe NS, Abdullahi MK (2019) Dietary Management of Diabetes Mellitus with Focus on International Journal of Diabetes Research 2: 26-32.
- Karakurt P, Aşılar RH, Yıldırım A, Sevinç H (2017) Knowledge levels and attitudes of diabetic patients about their European Journal of Therapeutics 23: 165-172.
- Herath HM, Weerasinghe NP, Dias H, Weerarathna TP (2017) Knowledge, attitude and practice related to diabetes mellitus among the general public in Galle district in Southern Sri Lanka: A pilot BMC public health 17: 535.
- Forouhi NG, Misra A, Mohan V, Taylor R, Yancy W (2018) Dietary and nutritional approaches for prevention and management of type 2 diabetes. BMJ 361:
- Gray A, Threlkeld RJ (2019) Nutritional recommendations for individuals with diabetes. In Endotext [Internet]. MDText com, Inc.
- Asdaq SMB (2018) Knowledge, Attitude, and Practice Regarding Diabetes Mellitus among General Public and Diabetic Patients in Riyadh, Saudi Arabia. Asian Journal of Pharmaceutics 12.
- American Diabetes Association (2019) Diabetes Supplement 1: S46-S60.
- Bano A, Afzal M, Sarwar H, Waqas A, Kousar S, et al. (2017) Dietary knowledge, attitude and practices of diabetes patients at Services Hospital Lahore. International Journal of Applied Sciences and Biotechnology 5: 227-236.
- Dell R, Holleran S, Ramakrishnan R (2002) Sample size determination, ILAR J 43: 207-213.
- Defeudis G, Khazrai YM, Di Rosa C, Secchi C, Montedoro A, et al. (2018) Conversation Maps™, an effective tool for the management of males and females with type 2 diabetes and mildly impaired glycemic control. Hormones 17: 113-117.
- Naghashpour M, Shakerinejad G, Lourizadeh MR, Hajinajaf S, Jarvandi F (2014) Nutrition education based on health belief model improves dietary calcium intake among female students of junior high schools. J Health Popul Nutr 32: 420-429.
- Kumari JD (2012) Effect of Nutrition Education on Anthropometric and Blood Glucose Levels of Niddm in Guntur City. Int J Med Med Sci 2: 095-099.
- Oosthuizen, D (2010) Impact of a nutrition education programme on nutrition knowledge and dietary intake practices of primary school children in Boipatong (Doctoral dissertation).
- Mohammadi S, Karim NA, Talib R (2015) Knowledge, attitude and practices on diabetes among type 2 diabetic patients in Iran: A cross-sectional study. Science 3: 520-524.
- Sami W, Alabdulwahhab KM, Ab Hamid MR, Alasbali TA, Alwadani FA, et al. (2020) Dietary Knowledge among Adults with Type 2 Di- abetes-Kingdom of Saudi Arabia. International journal of environ- mental research and public health 17: 858.
- Butcher E (2014) The Big Fat Lie About Burning Fat. Journal of Interdisciplinary Science Topics 3: 54.
- Klimek M, Knap J, Masternak M, Reda M (2019) Physical activity in prevention and treatment of type 2 diabetes mellitus. Journal of Education Health and Sport 9: 1175-1181.
- Yadav S, Singh A (2010) Contribution of nutrition education in dietary habits of overweight and obese females in Hathras City (UP). Pakistan Journal of Nutrition 9: 1047-1051.
Citation:Mutagwanya R, Nyago CM, Nakwagala FN (2020) Effect of Diabetes Nutrition Education on Diabetes Nutrition Knowledge and Physical Activity Duration among Patients with Type 2 Diabetes Mellitus: A Longitudinal Cohort Intervention Study. J Nutr Food Sci 3: 020.
Copyright: © 2020 Mutagwanya R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.