*Corresponding Author:
Teresa Deinlein,
Department of Dermatology, Medical University of Graz, Auenbruggerplatz 8, 8036 Graz, Austria
Tel: 031638531006
E-mail: teresa.deinlein@medunigraz.at
Abstract
Introduction: A few reports dealing with the preventive application and “peeling function” of Imiquimod are available to date describing the skin to be smoother and to show less pigment irregularities after application of Imiquimod.The aim of this study was to determine whether the topical use of Imiquimod improves the texture of the skin both structurally and aesthetically.
Material and Methods: 15 female patients were included in our study and guided to apply one sachet of Imiquimod 3.75%-Creme (Zyclara®) once daily on the décolleté over a period of 14 days. Imaging procedure (clinical and dermoscopic and images with a reflectance confocalmicroscope) was performed before, during and two weeks after application. Images were evaluated based on distinct parameters indicating sun-damaged skin. Statistical analysis was done by a repeated measures analysis of variance with a 2 by 4 measures design using the latest SPSS version (SPSS 23).
Results: Although 13 of the patients (86.6%) showed slight to marked signs of skin inflammation, neither clinically nor with confocal microscopy significant changes could be proven. Additionally, eight patients noticed an improvement of the skin texture in the treated area, however, neither structurally nor aesthetically marked alterations could be proven clinically, dermoscopically nor in RCM.
Discussion: We did not find any significant improvements in physi cian assessed clinical, dermoscopic and RCM parameters, however, most of the patients noticed subjective improvement.
Key Message
Imiquimod can slightly reduce UV-induced skin alterations, however, not reaching statistical significance.
Keywords
Actinic keratosis; Ageing; Confocal microscope; Dermoscopy
Introduction
Imiquimod is an immune response modifier (TL-7 agonist), which exact mechanism of action is still largely unkown. However, it is known to stimulate the innate and adaptive immune responses and to induce cytokine production. For this reason, Imiquimod is a favored therapeutic option in both benign and malignant skin disorders due to its antiviral, antitumor and immunoregulatory potential. Initially, Imiquimod was approved for the therapy of anogenital warts and subsequently received approval for the treatment of actinic keratoses and superficial basal cell carcinoma [1-4]. Besides aforementioned indications, Imiquimod is nowadays also used as an off-label therapy in a wide range of infectious, neoplastic and inflammatory skin diseases [1]. The term “photoaging” refers to cutaneous changes from a clinical and histological point of view leading to a premature aging process. This effect is due to cumulative exposure to ultraviolet (UV) radiation. of note, photoaging is not only a cosmetical problem, since chronic UV-damaged skin is the basis for the development of precancerous and cancerous skin lesions [1-4]. To date, a few case reports and small case series dealing with the preventive application and “peeling function” of Imiquimod are available [1-4]. The results suggest Imiquimod to be an effective agent regarding skin rejuvenation. In detail, the authors describe the skin to be smootherand to show less pigment irregularities after application of Imiquimod. Currently, Imiquimod is available as a 3.75% and 5% cream (Zyclara® and Aldara®). Hence, the aim of our study was to ascertain, whether chronic UV-damaged skin improves after topical treatment with Imiquimod both structurally and aesthetically.
Material and Methods
Patients´ characteristics
18 healthy female, caucasian volunteers (Fitzpatrick phototype IIIII), aged between 45 and 71 years (mean 57.4 years), with clinical signs of photo damage on the décolleté but without any clinical sign of a skin tumour or potential precursors were recruited within six months. Clinical investigations were conducted according to the principles of the Declaration of Helsinki and consent was given prior to enrollment, approval of the local ethical committee was also obtained (EK24-180ex11/12). Three participants interrupted the study for time reasons and data of 15 participants were included in theanalysis.
Schedule of application
Two weeks beforeenrollment, the participants were instructed not to apply any sunscreen, moisturizingcrème or topical medication at the décolleté. Baseline imaging procedureof the décolleté was performed and the participants were guided to apply the content of one sachet ofImiquimod 3.75%-Creme (Zyclara®) once daily on the décolletéover a period of 14days.
Imaging procedure
Baseline clinical images were obtained using a 10,2-megapixel digital camera (D200, Nikon Corporation®, Tokyo, Japan) and baseline dermoscopic pictures were done with a 4-megapixel digital camera (Nion Coolpix 4500®, Nikon, New York, USA) equipped with a contact polarized dermatoscope (DermLite® Photo 3Gen, California, USA). Reflectance confocal microscopy (RCM) images were acquired using the VivaScope1500® (Mavig, Munich, Germany). RCM-images (block, 4 x 4 mm) were taken at the level of stratum corneum and 3 more blocks, each 25µm deeper than the previous block, at the spinous layer, the level of DEJ (dermoepidermal junction) and the upper dermis. Dermoscopic and RCM-images were taken from the décolleté, exact 5 centimetres below the suprasternal notch. Imaging procedure was performed before, during (between day 10 and 14) and two weeks after the application-period of Imiquimod. After the last imaging procedure the volunteers received a questionnaire, which asked the following: Did you notice any changes/improvements concerning texture of the skin in the treated area after therapy with Imiquimod? If yes, please indicate in which way (several answers possible):
- Skin is firmer
- skin is smoother
- skin is softer
- skin shows less pigment inhomogeneity
- skin shows less wrinkles
Imaging evaluation
Clinical images were evaluated by two dermatologists, dermoscopic images by onedermatologist, respectively. Two dermatologists, experienced in RCM, performed RCM-evaluation consensually.The six criteria for clinical evaluations were based on the skin ageing score SCINEXA [5]. Due to its applicability for facial skin, we adapted it to our needs for the skin onthe décolleté (fine wrinkles, uneven pigmentation, lax appearance, pseudo scars, coarse wrinkles, and telangiectasia). The evaluated dermoscopic criteria (n=7) included hyperand hypopigmentation, poikilodermatic skin, telangiectasia, scales, red background and crusts. The presence of all aforementioned clinical anddermoscopic criteria were evaluated using a scoring system (0=absent, 1=mild, 2=moderate, 3=severe).
In RCM 17 criteria were evaluated. They were chosen following previously published RCM-criteria of sun-damaged skin and actinic keratosis [6-10]. The presence of the following criteria was assessed (0=absent, 1=present): Large rhomboidal furrows, disarranged rhomboidal furrow pattern, linear furrow pattern, hyperkeratotic areas, apoptotic cells, round nucleated cells and inflammatory cells. The presence of atypical honeycomb pattern, disarray of honeycomb pattern, mottled pigmentation, irregular rings, polycyclic rings, absence of rings, coarse collagen, huddled collagen, curled fibres and longitudinal vessels were graded from 0 to 3, according to previous clinical and dermoscopic evaluation.
Statistical calculations
Statistical data analysis was done by a repeated measures analysis of variance with a 2 (type of ratings, i.e., clinical and RCM criteria) by 4 (time, i.e., ratings at 4 different time points) measures design using the latest SPSS version (SPSS 23).
Results
15 participants with clinical photo-damaged skin on the décolleté were included in our study.During application period, 13 of the patients (86.6%) showed slight to marked signs of skin inflammation. In detail, reddish, partially ulcerated, papules were evident clinically. In some cases they were reminiscent of herpes-simplex lesions (Figure 1 A-F). Of note, in cases of an extensive inflammatory reaction a discreet cicatrization was observed. In dermoscopy signs of inflammation, namely erosions as well as dotted and linear vessels on a reddish background, were evident. However, results of the analysis of variance of the abovementioned six clinical criteria showed no statistical significant changes over time (F=0.90; p>0.39). Using reflectance confocal microscopy, signs of UV-damaged skin could be proven in all 15 cases. Nevertheless, statistical analysis of variance also revealed no significant changes before and after treatment (F=0.90; p>0.39).
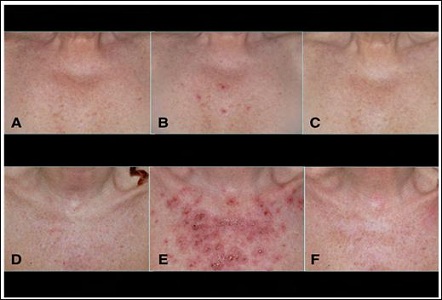
Figure 1: (A) Upper line: Baseline images of the décolleté, (B) Smooth inflammation during treatment, (C) Result two weeks after last application. (D) Lower line: Baseline image of the décolleté, (E) Intense inflammation during treatment and (F) Result after two weeks last application.
Evaluation of patients questionnaire
Based on aforementioned questionnaire, eight of the patients (53.33%) noticed changes/improvement of the skin texture in the treated area. These changes scattered as follows (several answers were possible – see also material and methods):
- Skin is firmer (one patient)
- Skin is smoother (one patient)
- Skin is softer (three patients)
- Skin shows less pigment inhomogeneity (two patients)
- Skin shows less wrinkles (three patients)
Discussion
Chronically UV-damaged skin on the one hand leads to a premature aging process and on the other hand causes a wide range of different skin tumors (e.g. actinic keratoses, squamous cell carcinoma, and basal cell carcinoma). Several studies were conducted showing theses UV-radiation induced changes clinically, histologically and by using reflectance confocal microscopy [11] There is growing evidence that there are subclinical cancerous precursors in chronically sun-damaged skin, which may constitute a base for new neoplastic lesions [12,13]. Furthermore, it is well known that the surrounding skin of visible UV-induced skin tumors (e.g. actinic Kerasotes) is commonly affected by subclinical changes (i.e. field cancerization).
Topical treatment of both apparent and invisible lesions may lead to reduced development of new lesions. In addition, preclinical studies suggest the “field therapy” to be very effective in preventing or delaying the recurrence of non melanoma skin cancer [13-17]. As already described in literature [7-10,13] and as our results also clearly show, reflectance confocal microscopy can be used as a valuable diagnostic imaging tool to evaluate signs of skin aging and UV-induced changes since microanatomical structures and individual cells can be depicted. Furthermore it can be considered worthy for the non-invasive monitoring of alterations during and after topical treatment. We did not find any significant improvement in UV-induced skin changes in our case series using Imiquimod over abovementioned period of time. Neither structurally nor aesthetically marked alterations could be proven clinically, dermoscopically or in RCM. There are a fewpossibilities for this phenomenon: i) small number of patients; ii) short application ofImiquimod; iii) no effect. Our results are in line with previous reported observations, as no significant effect regarding reduction of UV-induced skin alterations could be proven [2,3]. Some authors furthermore attribute Imiquimod some kind of “peeling effect” of the skin without leading to a marked and durable improvement regarding skin rejuvenation [3]. However, this “peeling effect” was not observed in our study. Notably, in 13 patients inflammatory reactions in various degrees of severity were observed during therapy. This might be explained by the hypothesis that even in chronically UV-damaged skin subclinical alterations are evident and therefore reacting with Imiquimod. To what extent these reactions are reducible to UV-induced mutations is still a matter of debate. Our study has some limitations. First, we have a small number of patients and therefore cannot provide significant statements. Second, clinical assessment was only based on images and we do not have any histopathological report.
We did not find any significant improvements in physician assessed clinical, dermoscopic and RCM parameters, however, most of the patients noticed subjective improvement.
Ethics
Reviewed and approved by the ethic committee of the Medical University of Graz (Approval number 24-180 ex 11/12)
Conflicts of Interest
The authors have no conflicts of interest to declare.
Funding Sources
There was no funding.
References
- Hanna E, Abadi R, Abbas O (2016) Imiquimod in dermatology: an Int J Dermatol 55: 831-844. Metcalf S, Crowson AN, Naylor M, Haque R, Cornelison R (2007) Imiquim-
- Prado A, Andrades P, Benitez S (2005) Preliminary results aftHanna E, Abadi R, Abbas O (2016) Imiquimod in dermatology: an Int J Dermatol 55: 831-844.
- Metcalf S, Crowson AN, Naylor M, Haque R, Cornelison R (2007) Imiquim-er face peels using Aldara cream 5% (imiquimod). Plast Reconstr Surg 116: 1563-1568.
- Kopera D, Kerl H (2010) Detection and treatment of preclinical aktinic keratoses (PAK). J Dtsch Dermatol Ges 8: 693-694.
- Vierkötter A, Ranft U, Krämer U, Sugiri D, Reimann V, et al. (2009) The SCINEXA: a novel, validated score to simultaneously assess and differentiate between intrinsic and extrinsic skin J Dermatol Sci 53: 207-211.
- Wurm EM, Curchin CE, Lambie D, Longo C, Pellacani G, et (2012) Confocal features of equivocal facial lesions on severly sun-damaged skin: four case studies with dermatoscopic, confocal, and histopathologic correlation. J Am Acad Dermatol 66: 463-473
- Longo C, Casari A, De Pace B, Simonazzi S, Mazzaglia G, et al. (2013) Proposal for an in vivo histopathologic scoring for skin aging by means of confocal Skin Res Technol 19: 167-173.
- Borsari S, Pampena R, Lallas A, Kyrgidis A, Moscarella E, et (2016) Clinical indications for use of reflectance confocal microscopy for skin cancer diagnosis. JAMA Dermatol 152: 1093-1098.
- Ulrich M, Maltusch A, Rius-Diaz F, Röwert-Huber J, González S, et al. (2008) Clinical applicability of in vivo reflectance confocal microscopy for the diagnosis of actinic Dermatol Surg 34: 610-619.
- Ulrich M, Rüter C, Astner S, Sterry W, Lange-Asschenfeldt B, et al. (2009) Comparison of UV-induced skin changes in sun-exposed sun-protected skin preliminary evaluation by reflectance confocal microscopy. Br J Dermatol 161 Suppl 3: 46-53.
- Stockfleth E (2017) The importance of treating the field in actinic J Eur Acad Dermatol Venereol Suppl 2: 8-11.
- Reygagne P, Rostain G (2018) Beyond actinic keratoses: Field cancerization of the Ann Dermatol Venereol 145: 587-592.
- Koller S, Inzinger M, Rothmund M, Ahlgrimm-Siess V, Massone C, et al. (2014) UV-induced alterations of the skin evaluated over time by reflectance confocal J Eur Acad Dermatol Venereol 28: 1061-1068.
- Hruza LL, Pentland AP (1993) Mechanisms of UV-induced inflammation. J Invest Dermatol 100: 35-41.
- Gilchrest BA, Soter NA, Stoff JS, Mihm MC 1981) The human suburn reaction: histologic and biochemical J Am Acad Dermatol 5: 411-422.
- Van Laethem A, Claerhout S, Garmyn M, Agostinis P (2005) The sunburn cell: regulation of death and survival of the keratinocyte. Int J Biochem Cell Biol 37: 1548-1553.
- Gilchrest BA, Soter NA, Hawk JL, Barr RM, Black AK, et al. (1983) Histological changes associated with ultraviolet A-induced erythema in normal human J AM Acad Dermatol 9: 213-219.
Citation: Arzberger E, Deinlein T, Schulter G, Hofmann-Wellenhof R, Kopera D (2019) Does the Use of Imiquimod Enhance Sun-Damaged Skin? – A Case Series of 15 Patients. J Clinic Exper Cosme Derma 2: 004.
Copyright: © 2019 Arzberger E, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.


