*Corresponding Author:
Surendra Ugale,
Department of Advanced Laparoscopy, Bariatric & Metabolic Surgery, Kirloskar & Virinchi Hospitals, Hyderabad, India
Tel: +91- 9573200951
Email: surenugale@gmail.com
Abstract
Background: Type-2 Diabetes Mellitus (T2DM) keeps afflicting more people worldwide. Not having much success through medical treatment, we have been using the surgical option of Laparoscop- ic Duodenal Ileal Interposition (DII) with Sleeve Gastrectomy (SG) [D-IISG], since 2010, which offers good metabolic improvement and weight reduction without causing significant malabsorption. The ob- jective of this study was to evaluate the results of this procedure over 10 years, for control of type 2 diabetes along with any accompanying obesity, while maintaining nutritional stability.
Methods: Retrospective study and analysis of prospectively collect- ed data of 154 patients that underwent laparoscopic DII with BMI-ad- justed SG (DII+SG) was done.
The DII & SG was performed in 154 patients from March 2010 to December 2019 by a single surgeon and team. Participants had a mean age of 46.9 years (range 22-72), mean duration of diabetes was 11.64 years (range 1-40) and mean preoperative BMI was 30.4 kg/m2 (range 20-51). All patients had poorly controlled type 2 dia- betes mellitus [(mean HbA1c- 9.47% (range 6.2-14.4)] despite use of Oral Hypoglycemic Agents (OHA) and/or Insulin; or good control with fluctuations and very high doses of medication. Mean fasting C-peptide was 2.69ng/ml and 68.5% were on insulin. Remission of diabetes (HbA1c ≤ 6.5% without OHAs/Insulin) and weight mainte- nance were the main outcomes studied with nutritional status.
Results: With a follow up of 87% at 1 year, 57% and 45% at 7 and 8 years respectively, postoperative glycemic parameters (FBS, PLBS, HbA1C) improved in all patients (p<0.05) at all intervals.
With a mean follow up of 66 months (range 12-120 months), 70.9% had remission of diabetes at 1 year, 75 and 73% at 5 and 7 years respectively, which declined to 62.5% by end of 8 years.
Mean weight loss was 23.5% (18-28 %), (p<0.05). At 1 year, the mean fall in HbA1c(29.7%) was more than the reduction in BMI(23%) Percentage of total weight loss was 21.3% at 5 years with mean BMI of 25.6, whereas %TWL at 10 years was 16.5% with mean BMI of Patients exhibited good nutritional stability even at 10 years.
Conclusion: Duodenal Ileal Interposition with sleeve gastrectomy is a very effective option for long term control of diabetes and obesity with nutritional stability.
Keywords
Glycemic control; Ileal interposition; Low BMI; Nutritional stability, Type-2 Diabetes; 10 year results
Introduction
The global search for better medical, technological and surgical options, to combat Type-2 Diabetes Mellitus (T2DM), goes on. Medical options have had limited success and the morbidity and man-days lost, due to complications of DM, keep increasing year after year. Since 2010, we have been performing Laparoscopic Duodenal Ileal Interposition with BMI-adjusted Sleeve Gastrectomy (DII+SG), as presented by the pioneer, Aureo DePaula from Goiania, Brazil [1]. This has been considered by some as the “Ferrari of all Metabolic procedures” as it requires greater effort, to create a BMI-adjusted Sleeve with ileal interposition, with minimal (50 cms) bowel exclusion, to reduce any possibility of malabsorption [2].
Methods
154 patients underwent this procedure, after an ethical committee approval and written informed consent, since 2010. These were all di- abetics who underwent detailed history-taking, clinical examination and laboratory investigations to check all systems for fitness for anes- thesia and surgery.
Decision to perform a DII+SG was done after ensuring adequate pancreatic function with C-peptide and serum insulin in fasting state and 1 hour after glucose meal stimulation. GAD and Islet cell antibod- ies were checked when necessary, to rule out Type-1 diabetes or Latent Auto-Immune Diabetes of Adult (LADA). The baseline parameters of these patients are outlined in Table 1.
Most of the patients had severe, uncontrolled diabetes, with 68.5% on insulin treatment. 6.67% had fasting C-peptide<1, while majority of patients (68%) had<3ng/ml; duration was ≥ 10 years in nearly 60% and HbA1c ≥ 10% in 35%, all indicating severe disease. (Tables 1.a, 1.b).
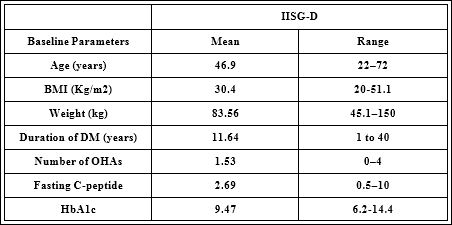
Table 1: Baseline parameters; Body Mass Index (BMI); Oral Hypoglycemic Agents (OHA); glycosylated hemoglobin (HbA1c).

Table 1.a
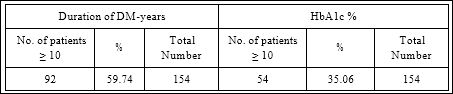
Table 1.b
This is a single surgeon experience with Indian diabetics; the se- verity of diabetes (DM) was also established using the DRS scoring system [3], which showed that only 14% were in mild category, with 86% having a greater severity of DM (69% moderate and 17% severe). Table 1.c

Table 1.c: DRS score indicating severity of diabetes in this cohort.
Remission of diabetes has been considered if HbA1c ≤ 6.5%, without any medication for 1 year, as physicians in clinical practice here use this benchmark. The result is considered as “good glycemic control” if HbA1c<7% without any medication; physicians usually prescribe medication only if HbA1c is>7%.
Inclusion criteria- Patients with T2DM>1 year duration; Age 20- 70 years usually, with rare exceptions in very fit individuals ; Stable weight for the last 3 months (variation in weight<3%); BMI ≥ 20kg/ m2; Inadequate glycemic control with HbA1c>7% on optimum dosage of insulin and/or OHA; stimulated C-peptide level>1ng/ml.
Exclusion Criteria- Type-1 DM; Undetectable fasting C-peptide; Positive urine ketones, pregnancy; Coexisting severe hepatic, pulmo- nary, renal, cardiovascular, neurological and psychiatric diseases and obesity due to organic illness; addiction to alcohol or illicit drugs.
Preoperative Evaluation- Subjects had mean age of 46.9 years (range 22-72), mean duration of diabetes 11.64 years (range 1 to 40) and mean preoperative BMI of 30.4 kg/m2 (range 20-51). All patients had poorly controlled T2DM with a mean HbA1c-9.47% (range 6.2- 14.4) despite use of OHA and/or Insulin.
Preoperative evaluation included assessment of serum insulin, basal and 1hr post meal C-peptide.
Outcomes
Primary outcome measure- Remission of T2DM, defined as HbA1c ≤ 6.5% without requiring oral or parenteral hypoglycemic agents, for 1 year.
Secondary outcomes measures- Improvement in glycemic pa- rameters (HbA1c, Fasting blood sugar [FBS], Post Lunch Blood Sugar [PLBS]), maintenance of weight and BMI, nutritional parameters.
Procedure Details
With a six-port laparoscopic technique, a BMI-adjusted sleeve gastrectomy was performed using a 36-50 French calibrator. The en- do-GIA stapler with 60-mm cartridges was used for gastric resection and the staple line was reinforced by imbricating 3-0 polydioxanone sutures. Non-obese patients were subjected to mainly fundectomy, leaving a good volume of residual stomach. The devascularization of the greater curvature of the stomach was continued onto the duode- num, 3-4 cm beyond the pylorus, as far as the gastro-duodenal artery. The duodenum was transected, distal stump was reinforced with 3-0 polydioxanone continuous suture, and the resulting gastro-duodenal tube was then passed into the inframesocolic space through an opening created at the root of mesocolon.
A distal ileal segment of 100-170 cm in length (depending on total small bowel length) was created by dividing the ileum at two points, 30 cm and usually 200 cm from the ileocecal valve preserving its mes- enteric pedicle. Continuity of small bowel was restored by a stapled side to side ileo-ileal anastomosis.
The gastro-duodenal tube was anastomosed to the proximal end of the ileal segment end to side in an iso-peristaltic manner in 1 or 2 lay- ers using intracorporeal hand suturing with 3-0 polydioxanone. The distal end of the ileal segment was anastomosed to the jejunum 50 cm from the ligament of Treitz with a stapled side to side anastomosis. All anastomoses were performed using 45-mm linear staplers with white cartridges, and 3-0 polydioxanone enterotomy suture closure [4].
The linear defect in the distal ileal mesentery, the circular defect in the transverse mesocolon and the two arched defects in ileo-jejunal mesentery and the gastro-ileal anastomosis are closed using 3-0 poly- propylene sutures to prevent internal herniation [5] (Figure 1). The 10 and 12 mm trocar openings were closed with 1-0 polydioxanone sutures using a suture-passer instrument, after removing the gastric specimen; if necessary, a flat Penrose drain was placed along the sleeve and the duodenal stump.
Postoperative follow up
Medication was adjusted according to the plasma glucose (measured 3 hourly, with insulin used according to sliding scale) and blood pressure levels. The patients were kept on a liquid diet, started 24-36 hrs after surgery, for 5-7 days, followed by semisolid diet for another 7 days, and finally a solid diet. The patients were discharged between 3-5th postoperative day with vitamin supplements. Follow up is encouraged every 3-monthly in 1st year, 6-monthly in 2nd and 3rd years, then annually for life, for clinical and laboratory evaluation.
Outcomes measures were recorded prospectively.

Figure 1: DII+SG (ref-Chapter “Metabolic Surgery for Diabetes and Hyperlipidemia”, 3rd Ed. 2019, Surgical Gastroenterology, Editor Sanjiv Haribhakti, Paras Medical Pub- lisher).
Results
We had 87% follow-up at 1 year, 52%, 57% and 45% at 5, 7 and 8 years respectively.
Mean follow up was 66 months (range 12-120 months) (Table 2).
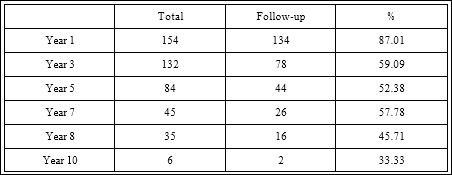
Table 2: Rates of follow-up.
Postoperative glycemic parameters (FBS, PLBS, HbA1c) improved in all patients (p<0.05) at all intervals (Table 3).
The mean FBS and PPBS were well controlled for 5 years; our data shows these worsening from 7-10 years.
#Levels of FBS / PPBS over 8/10 years
70.9% had remission of diabetes at 1 year, 75 and 73% at 5 and 7 years respectively, which declined to 62.5% at end of 8 years.
Excellent long term control of glycemia, in 82-84% of patients upto 8 years, with mean A1c <7% over 10 years, and >80% of those needing insulin initially, did not require insulin, at 8 years.
Reduction in BMI at 5 yrs is 19.7% while HbA1c reduction is
At 5 years mean fall in HbA1c (34.5%) was more than reduction in BMI (19.7%).
At 8 years, A1c reduction of 30.7% was again >>> than BMI 17.4% (Tables 4-6, Figure 2).

Table 3: Glucose control over 10 years; mean values of FBS=Fasting blood sugar, and PPBS= Post-prandial blood sugar.

Table 4: Remission rates for D-IISG upto 10 years with mean values of HbA1c.
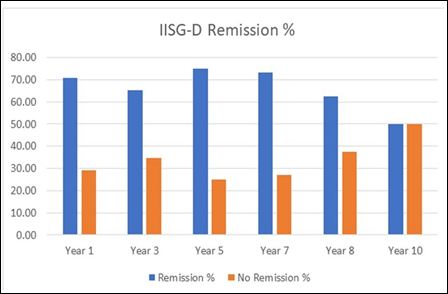
Figure 2: Remission rates upto 10 years.
Excellent long term control of glycemia, with A1c between 6.2- 6.56% over this 10 year period. This was accompanied by very effec- tive weight maintainance, with mean BMI between 22-25.8kg/m2 throughout the 10 year period, having 20% TWL at 5 and 8 years. This long term success was achieved with a negligible bowel exclusion of only 50cms of jejunum, as compared to BPD-DS, where 350-700cms of small bowel could be excluded (Tables 6.a-9).
Discussion
This procedure was favoured instead of the other bypass or sleeve plus procedures, as this has no bowel exclusion and no bypass, yet results in very good long term control of diabetes and weight, even at 10 years. This might prove to be a healthier way to lose weight and get diabetic control [6].

Table 5: Distribution of BMI groups, mean HbA1c and duration of diabetes, and their correlation with remission rates over 10 years.

Table 6: Efficacy of BMI and diabetes control over 10 years.
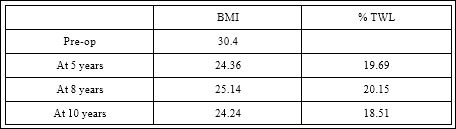
Table 6.a: Mean BMI and percentage of total weight loss at 5, 8 and 10 years.
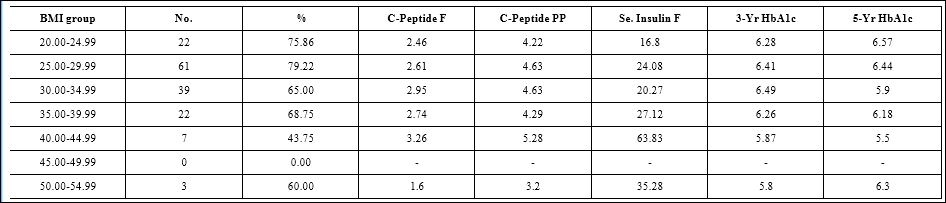
Table 7: Correlation of C-peptide and insulin levels, in different BMI groups, with HbA1c control at 3 and 5 years. [F=Fasting; PP=Postprandial].
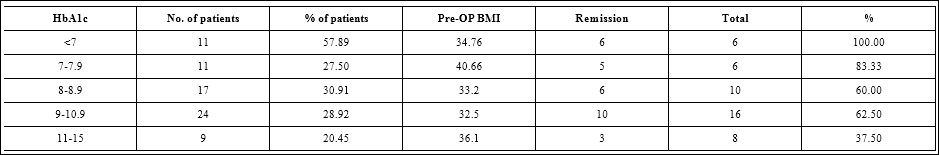
Table 8: The poorly controlled patients with high HbA1c, had poorer response, compared to the better controlled patients with A1C ≤ 8, and even upto 11%.
Reasonably good follow-up of 73% at 5 years and 63% at 10 years, probably offsets the disadvantage of the smaller total number of patients being 72.75% were moderate and severe diabetics as assessed by the DRS scoring system. Remission of 65.7% at 1 and 3 years, gradually declined to 57% at 5 years and 30% at 10 years, although 43% maintained A1c ≤ 7 even at 10 years. Even though 54% were on insulin preoperatively, nearly half of them had diabetic control without insulin at 10 years.
About 10% had BMI<25, 30.5% had BMI<30, with nearly 60% being<35kg/m2. Yet the results were comparable with those whose BMI>35, upto 10 years; such long term data could lay the grounds for establishing new guidelines, allowing surgical intervention, for poorly controlled diabetes, without any BMI restrictions [7,8].

Table 9: TThis shows that persons with BMI <35, responded nearly as well as those with >35 with good diabetic control which was maintained upto 10 years.

Table 10: Nutritional stability over 10 years as shown by mean values of different nutrients; Hb=Hemoglobin; Vit= Vitamin.
Since the majority were having BMI<35, it is not surprising that the %TWL was 21% at 5 years maintaining a good BMI of 25, and 16.5% at 10 years having BMI of 27kg/m2. Greater insulin resistance was seen in BMI<30, with higher fasting serum insulin levels, indicating sufficient insulin reserve; no insulinopenia seen at these levels, giving us further confidence to operate on such patients [9].
Better preoperative control and reduction of HbA1c, may favour good results and those with high A1c levels preop had poorer response to surgery. Since there is no bypass of any portion of the gastrointestinal (GI) tract in this procedure, there is no malabsorption expected, which is shown by the good nutritional stability upto 10 years (Table 10); supplements were used routinely for 1st year, and later only if any deficiency was found during follow-up checks [10].
The downside of not doing any bypass of the duodenum and proximal jejunum, is the reduced efficacy of the procedure, as the duodenal anti-incretin factor is not overcome, as seen in the diverted or duodenal ileal interposition [11].
Efficacy of this procedure has been shown by many studies [1218], along with its safety profile [19-21], its efficacy of comorbidity resolution [22-23] and very importantly, its safety in low BMI diabetics [24-27].
Conclusion
J-IISG is a very good option for surgical treatment of T2DM, especially with mild and moderate severity of DM and BMI>30, although its efficacy and safety even in low BMI diabetics has been shown here. Having no bowel exclusion is an attractive option especially for the lower BMI diabetics, who do not tolerate malabsorption well, using bypass procedures. These 5 and 10-year results should encourage surgeons to study this procedure in larger number of patients at multiple centers. Being a procedure requiring 3 transections, 3 anastomoses with closure of all mesenteric gaps, attention to details with good technical skills and initial proctoring of surgeons is important.
Conflict of Interest
None of the authors have any conflict of interest.
No funding was obtained for this study.
References
- Paula A, Macedo A, Prudente A, Queiroz L, Schraibman V, et al. (2006) Laparoscopic sleeve gastrectomy with ileal interposition (“neuroendocrine brake”)-pilot study of a new Surgery for obesity and related dis- eases 2: 464-467.
- Huang C, Katakwar A (2020) Sleeve plus procedures: Need of time. Surg Today 50: 419-422.
- Ugale S, Gupta N, Modi KD, Kota SK, Satwalekar V, et al. (2014) Prediction of remission after metabolic surgery using a novel scoring system in type 2 diabetes - a retrospective cohort J Diabetes Metab Disord 13: 89.
- Maljaars PW, Peters HP, Mela DJ, Masclee AA (2008) Ileal brake: A sen- sible food target for appetite control. A review. Physiology and Behavior 95: 271-281.
- Ugale SM, Celik A (2016) Ileal Interposition with Sleeve Gastrectomy for Type 2 Diabetes Mellitus and Metabolic Obesity, Bariatric and Metabolic Surgery 547-554.
- DePaula AL, Stival AR, Halpern A, Vencio S (2011) Surgical treatment of morbid obesity: mid-term outcomes of the laparoscopic ileal interposition associated to a sleeve gastrectomy in 120 Obes Surg 21: 668-675.
- Celik A, Ugale S, Ofluoglu H, Vural E, Cagiltay E, et (2015) Metabolic Outcomes of Laparoscopic Diverted Sleeve Gastrectomy with Ileal Trans- position (DSIT) in Obese Type 2 Diabetic Patients. Obes Surg 25: 2018- 2022.
- Schauer PR, Bhatt DL, Kirwan JP, Wolski K, Aminian A, et al. (2017) Bar- iatric Surgery versus Intensive Medical Therapy for Diabetes - 5-Year Out- N Engl J Med 376: 641-651.
- De Paula AL, Stival AR, Halpern A, DePaula CC, Mari A, et al. (2011) Improvement in insulin sensitivity and β-cell function following ileal in- terposition with sleeve gastrectomy in type 2 diabetic patients: Potential J Gastrointest Surg 15: 1344-1353.
- Foschi DA, Rizzi A, Tubazio I, Conti L, Vago T, et al. (2015) Duodenal diverted sleeve gastrectomy with ileal interposition does not cause biliary salt Surg Obes Relat Dis 11: 372-376.
- De Paula AL, Stival AR, Macedo A, Ribamar J, Mancini M, et al. (2010) Prospective randomized controlled trial comparing 2 versions of laparo- scopic ileal interposition associated with sleeve gastrectomy for patients with type 2 diabetes with BMI 21-34 kg/m(2). Surg Obes Relat Dis 6: 296-
- DePaula AL, Stival AR, DePaula CC, Halpern A, Vencio S (2012) Surgi- cal treatment of type 2 diabetes in patients with BMI below 35: Mid-term outcomes of the laparoscopic ileal interposition associated with a sleeve gastrectomy in 202 consecutive J Gastrointest Surg 16: 967-976.
- Ugale S, Agarwal D, Satwalekar V, Rao N, Ugale A (2016) Bariatric surgery as an option for diabetes mellitus prevention and treatment in obese per- Minerva Endocrinol 41: 469-476.
- Tinoco A, El-Kadre L, Aquiar L, Tinoco R, Savassi-Rocha P (2011) Short- term and mid-term control of type 2 diabetes mellitus by laparoscopic sleeve gastrectomy with ileal World J Surg 35: 2238-2244.
- Kota SK, Ugale S, Gupta N, Naik V, Kumar KV, et al. (2012) Ileal interpo- sition with sleeve gastrectomy for treatment of type 2 diabetes mellitus. Indian J Endocrinol Metab 16: 589-598.
- De Paula AL, Macedo ALV, Rassi N, Machado CA, Silva LQ, et al. (2008) Laparoscopic treatment of type 2 diabetes mellitus for 265 patients with a body mass index less than Surg Endosc 22: 706 -716.
- Goel R, Amin P, Goel M, Marik S (2011) Early Remission of Type-2 Dia- betes Mellitus by laparoscopic Ileal Transposition with Sleeve Gastrectomy Surgery in 23-35 BMI Int J Diabetes Dev Ctries 31: 91-96.
- De Paula AL, Macedo AL, Rassi N, Vencio S, Machado CA, et al. (2008) Laparoscopic treatment of metabolic syndrome in patients with type 2 di- abetes Surg Endosc 22: 2670-2678.
- DePaula AL, Stival A, Halpern A, Vencio S (2011) Thirty-day morbidity and mortality of the laparoscopic ileal interposition associated with sleeve gastrectomy for the treatment of type 2 diabetic patients with BMI <35: an analysis of 454 consecutive World J Surg 35: 102-108.
- Goel R, Nasta AM, Goel M, Prasad A, Jammu G, et al. (2020) Complica- tions after bariatric surgery: A multicentric study of 11,568 patients from Indian bariatric surgery outcomes reporting J Minim Access Surg.
- Celik A, Ugale S, Ofluoglu H, Asci M, Celik BO, et al. (2015) Technical fea- sibility and safety profile of laparoscopic diverted sleeve gastrectomy with ileal transposition (DSIT). Obes Surg 25: 1184-1190.
- DePaula AL, Stival AR, DePaula CC, Halpern A, Vêncio S (2010) Impact on dyslipidemia of the laparoscopic ileal interposition associated to sleeve gastrectomy in type 2 diabetic J Gastrointest Surg 14: 1319-1325.
- DePaula AL, Macedo AL, Schraibman V, Mota BR, Vencio S (2009) Hor- monal evaluation following laparoscopic treatment of type 2 diabetes mel- litus patients with BMI 20-34. Surg Endosc 23: 1724-1732.
- Frenken F, Cho EY, Karcz WK, Grueneberger J, Kuesters S (2011) Improve- ment of Type 2 Diabetes Mellitus in Obese and Non-Obese Patients after the Duodenal Switch Journal of Obesity 860169.
- Celik A, Cagiltay E, Ugale S, Asci M, Celik BO, et (2016) Diverted sleeve gastrectomy with ileal transposition in overweight, obese, and morbidly obese patients with type 2 diabetes: Results of 1-year follow-up. Surg Obes Relat Dis 12: 541-549.
- Baskota A, Li S, Dhakal N, Liu G, Tian H (2015) Bariatric Surgery for Type 2 Diabetes Mellitus in Patients with BMI<30 kg/m2: A Systematic Review and Meta-Analysis. PLoS One 10: e0132335.
- Huang ZP, Guo Y, Liu CQ, Qi L, Zou DJ, et al. (2018) The effect of meta- bolic surgery on non-obese patients (BMI<30 kg/m2) with type 2 diabetes mellitus: A systematic review, Surgery for Obesity and Related Diseases.
Citation: Ugale S, Ugale A, Ugale A, Ram T (2020) Diabetes and Obesity Control Following Duodenal Ileal Interposition with BMI-Adjusted Sleeve Gastrectomy-10years Data from a Single Surgeon Experience. J Diab Meta Syndro 3: 011.
Copyright: © 2020 Ugale S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.