*Corresponding Author:
Juan Farak Gómez,
Rafael Núñez University Corporation, Cartagena de India, Colombia
Tel: +57 3113163611
Email: jfarakg10@curnvirtual. edu.co
Abstract
Objective
To describe the case of a school patient with cutaneous leishmaniasis, given that it is a pathology that the World Health Organization (WHO) classifies as an emerging and uncontrolled disease.
Case report
A 15-year-old female patient with a history of recent travel to an endemic area, with a one-month history consisting of a lesion on the right cheek that began as a carbuncle, with subsequent ulceration that increased in size. On physical examination, there is evidence of a rounded ulcer of about 2x2 cm in diameter with sharp, raised edges and a relatively clean bottom. Adenomegaly is palpated in the ipsilateral maxillary subangle region. Direct smear examination for leishmania identifies and diagnoses cutaneous leishmaniasis. Management with ammonia was performed and the patient recovered satisfactorily.
Conclusion
Cutaneous leishmaniasis is a disease that, despite having a high incidence at a global level, continues to be an uncontrollable disease that can cause great repercussions on public health, so this report should be considered as an alert to the system epidemiological surveillance for this clinical presentation to be considered as a possible diagnostic alternative in endemic areas.
Keywords
Cutaneous leishmaniasis; Leishmania; School
Introduction
Leishmaniasis is a global public health problem. Every year around 2 million new cases are reported, distributed in 88 countries, in which the disease is considered endemic, of these, 1.5 million correspond to cutaneous leishmaniasis and only 15% occur in pediatric age [1].
In this pathology, the lesions appear mainly in the exposed areas, such as the face, upper and lower extremities. It usually manifests as a small painless nodule of chronic evolution that subsequently ulcerates, painlessly, with raised and indurated edges. Leishmaniasis cases are usually confirmed through microbiological analysis as lesion scrapings (smears) on Giemsa-stained slides [2].
Presentation of the Case
A 15-year-old female patient from a rural area, with a clinical evolution of approximately 1 month, characterized by a lesion on the right cheekbone that begins as an abscess which drains purulent material, associated with feverish symptoms. The parents reported that approximately 3 months ago he was in the rural area of the municipality of Tierralta, El Loro village for 15 days. Upon admission, he was in fair general condition, an ulcerated and rounded lesion of more or less 2x2 cm in diameter with sharp and raised edges and a relatively clean bottom was observed (Figure 1). Adenomegaly is palpated in the ipsilateral maxillary subangle region. He was admitted for pediatrics on suspicion of cutaneous leishmaniasis. In general, the laboratory studies were normal, a direct smear was made for Leishmania, giving a positive result (Figure 2). Therefore, the diagnosis of cutaneous leishmaniasis was confirmed and management was started with meglumine antimoniate (glucantime®) 20 mg/kg/day, discharge was given a week after starting the pharmacological management given the positive response of the condition and continued on an outpatient basis. He is currently under outpatient follow-up, and improvement has been observed, with a great decrease in the ulcerative lesion, without signs of reactivation or the presence of new lesions.
Discussion
Cutaneous leishmaniasis is a disease with a high prevalence in tropical and subtropical areas of the world. The WHO classifies leish- maniasis as an emerging and uncontrolled disease, as it is endemic in 88 countries on four continents and around two million new cases are reported each year. This disease constitutes a great problem for public health due to the high costs it generates [3].
The localized form of cutaneous leishmaniasis is the most com- mon in both children and adults. Manifesting especially in exposed areas such as the face and extremities, generally. About 70% of the cases present as solitary lesions, with an erythematous, slow-growing and asymptomatic papule, which subsequently ulcerates and remains chronically, to later resolve, leaving a residual scar. At other times a warty growth plate may develop [4].
In the case of the patient discussed here, the condition was local- ized, ulcerative and with the presence of enlarged lymph nodes, thus ruling out the possibility of systemic leishmaniasis. The latter taking into account that it has been documented that, from 5 to 10% of pa- tients with localized cutaneous leishmaniasis, may have adenomegaly, and that given this finding, the possibility of suffering from a systemic condition must be ruled out [5].
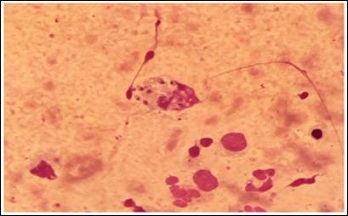
Figure 1: Cutaneous leishmaniasis lesión.

Figure 2: Direct test for Leishmaniasis.
Diagnostic alternatives for parasite detection are specific, but not very sensitive, however, they are accessible and must be applied in all clinical forms of the disease. These include microscopic examination of smears, scrapes, or aspirates, taken from the edge of the lesions [6].
Currently, the first treatment choice for cases of cutaneous leish- maniasis in our region is pentavalent antimony: N-methylglucamine antimoniate or sodium stibogluconate. Other pharmacological mea- sures that have been used are miltefosine and amphotericin B, as sec- ond-line drugs. In general, the dose of pentavalent antimony for all forms of leishmaniasis is 20 mg / kg per day [7].
Treatment of localized cutaneous leishmaniasis not only reduces scars, but also prevents both dissemination and relapse and is indicat- ed in persistent lesions of six months of evolution, or more, in multi- ple, large lesions, located in face, hands, or over joints, or if there is a risk of mucous membranes [8].
In conclusion, the report of this case should be considered as an alert to the epidemiological surveillance system so that this clinical presentation is considered as a possible diagnostic alternative in en- demic areas [9].
References
- Alvar J, Vélez I, Bern C, Herrero M, Desjeux P, et (2012) The WHO lesh- maniasis control team. leishmaniasis worldwide and global estimates of its incidence. PLoS ONE 7: 35671.
- Harper J, Oranje A, Prose N (2006) Leishmaniasis. Textbook of pediatric dermatology (2nd edn). Wiley, Boston, USA.
- Álvarez AMM (2010) Aspectos de interés sobre un parasit- ismo exótico para Cuba. Revista Cubana de Higiene y Epidemiología 48: 77-91.
- Burstein Alva, Z, Guillén A (2002) Leishmaniasis cutánea y mucocutánea (CIE-10 B55 1-B55-2) en el Perú. Rev Peru Med Exp Salud Publica 19: 215-218.
- Mondolfi AEP, Duffey GB, Horton LE, Tirado M, Jaimes OR, et (2013) Tropical medicine rounds intermediate/borderline disseminated cutane- ous leishmaniasis. Int J Dermatol 52: 446-455.
- Eiras DP, Kirkman LA, Murray HW (2015) Cutaneous leishmaniasis: Cur- rent treatment practices in the USA for returning Curr Treat Op- tions Infect Dis 7: 52-62.
- Ampudia G, Alejandra M (2013) Prevalencia de leishmaniasis cutánea en el Cantón de pedro vicente maldonado en el periodo de tiempo 2012 y USFQ, Ecuador, USA.
- Garcia AL, Parrado R, De Doncker S, Bermudez H, Dujardin JC (2007) American tegumentary leishmaniasis: Direct species identification of Leishmania in non-invasive clinical Trans R Soc Trop Med Hyg 101: 368-371.
- Rincón MY, Silva SY, Dueñas RE, López-Jaramillo P (2009) Leishmaniasis cutánea diseminada: Reporte de dos casos en Santander, Colombia. Rev Salud Pública 11: 145-150.
Citation:Delgado JT, Ortiz MM, Contreras FM, Herrera MH, Olivares AV, et al. (2021) Cutaneous Leishmaniasis in Hospital San Jeronimo De Monteria: A Case Report. J Perina Ped 5: 012.
Copyright: © 2021 Delgado JT, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.