*Corresponding Author:
Chen-Jei Tai,
Department of Traditional Chinese Medicine, Taipei Medical University Hospital, No.252, Wuxing St., Xinyi Dist., Taipei City 110, Taiwan
Tel: +886 2273721813102
Email: chenjtai@tmu.edu.tw
Abstract
Bell’s palsy is the appellation commonly used to describe an acute peripheral facial palsy of unknown cause. It is the most common disorder which affects the facial nerves and results in weakness or paralysis on one side of the face. The main pharmacologic therapy for acute Bell’s palsy is early short-term oral glucocorticoid treatment. Acupuncture is part of Traditional Chinese Medicine (TCM) and has been used for thousands of years. It involves inserting fine needles into specific acupuncture points on the skin or applying various other techniques to the acupuncture points to bring about treatment. A number of published research articles have suggested acupuncture is beneficial for patients with Bell’s palsy. Even thought more studies and clinical evidence are appreciated, current researches and results suggest that acupuncture plays a crucial role in the Bell’s palsy treatment. In addition, acupuncture does relieve Bell’s palsy sequelae and improve life-quality outcome of these patients.
Keywords
Acupuncture; Bell’s palsy; Idiopathic facial palsy; Traditional chinese medicine
Abbreviations
TCM = Traditional chinese medicine
Introduction
Bell’s palsy is the appellation commonly used to describe an acute peripheral facial palsy of unknown cause. It is the most common disorder which affects the facial nerves and results in weakness or paralysis on one side of the face [1]. It represents nearly half of all cases of facial nerve palsy [2]. The annual incidence rate is between 13 and 34 cases per 100,000 population [3]. More than 60,000 people were affected by this disease each year in the United States alone [4]. The peak age when Bell’s palsy occurred was in the fourth decade of life and 55.1% of patients were male [5]. The highest incidence of Bell’s palsy has been observed in the warm seasons; spring and summer. Diabetes Mellitus is the most common comorbid condition associated with Bell’s Palsy. In addition, a recurrence was more likely to occur in the first 1.5 years after its first onset [5]. The paralysis causes distortion of facial features and interferes with normal functions, such as closing the eye and eating. Most patients with Bell’s palsy will recover within 3 weeks, with or without medical intervention [3]. But about 30% of patients have sequelae [6]. Since facial symmetry frequently determines an individual’s appearance or influences interpersonal attraction [7], the asymmetry will affect psychological and social behaviors, and aggravate quality of life [8]. A study found a bidirectional temporal association between Bell’s palsy and anxiety disorders. After one of these two conditions develops, the morbidity rate for the other will significantly increase [9].
The main pharmacologic therapy for acute Bell’s palsy or facial nerve palsy of suspected viral etiology is early short-term oral glucocorticoid treatment. And in severe acute cases, it will combine antiviral therapy with glucocorticoids, which may improve outcomes [10]. Eye care is also important for patients with incomplete eye closure [11].
Some surgeons suggest for early phase Bell’s palsy patient surgical decompression of the nerve as a possible surgical intervention. But according to recent research, there is only very low quality evidence from randomised controlled trials, and this is insufficient to decide if surgical intervention is beneficial or harmful in the management of Bell’s palsy [12].
Current Research
Acupuncture has become an safe alternative therapy for Bell’s palsy [13], and no evidence of harm has been reported [14,15]. A research showed that there was cortical reorganization in the brain of patients recovered from Bell’s palsy after acupuncture treatment, which also suggested the relationship between the hand motor areas and facial motor areas of Bell’s palsy patients [16]. Another research showed that effects of the acupuncture on functional connectivity were closely related to clinical duration in patients with Bell’s palsy, which suggested that brain response to acupuncture was closely connected with the status of brain functional connectivity and implied that acupuncture plays a homeostatic role in the Bell’s palsy treatment [17]. A Cochrane review on the efficacy of acupuncture for Bell’s palsy was unable to draw conclusions successfully, owing to defects in experimental design and reports of the included studies [1]. A recent systematic review and meta-analysis of randomized controlled trials involved 14 trials and 1541 cases, treatment with acupuncture was carried out recently. The results showed that the total effective response rates in the acupuncture and control groups were 95.48% and 82.81%, respectively. Acupuncture therapy was associated with an increased total effective response rate (RR 1.14, 95% CI: 1.04-1.25, P = 0.005) with significant heterogeneity among the included studies (I2 = 87%). However, the review claimed that the current available evidence is insufficient to support that acupuncture is an effective therapy for Bell’s palsy due to the poor quality of included researches [15].
Patients with incomplete recovery of facial function following Bell’s palsy can have varying degrees of facial weakness, hypertonia, and synkinesis, with functional problems related to incomplete eye closure, brow ptosis, and nasal valve collapse [18]. No treatment has been demonstrated to be effective in the sequelae stage of Bell’s palsy except mime therapy, the clinical effectiveness of which has been demonstrated in a randomized controlled trial [19,20]. A recent randomized trial has established the effectiveness of acupuncture treatment for the patients with sequlea of Bell’s palsy whose onsets were longer than six months [20].
Discussion
According to Traditional Chinese Medicine (TCM) facial paralysis or Bell’s palsy is known as ‘deviated mouth’. It was because of the ‘wind’ by past dynasties. And ‘qi’ refers to the vital materials comprising the human body and the physiological works of viscera and bowels, channels and collaterals. It maintains the life activities and associates with the resistance of the human body. ‘Qi’ deficiency may contribute to the invasion of exogenous pathogenic wind. Acupuncture is part of TCM and has been used for thousands of years. It involves inserting fine needles into specific acupuncture points on the skin or applying various other techniques to the acupuncture points to bring about treatment. In Bell’s palsy, acupuncture treatment is to regulate channels and balance, harmonize qi and blood, strengthen the human body’s resistance to pathogenic elements, increase the excitability of the nerve, promote regeneration of the nerve fibers and formation of its collateral branches, enhance muscle contraction and blood circulation, and accelerate metabolism and recovery of body functions [1,21,22].
Recent researches also confirmed that acupuncture can result in functional connectivity modulation, which is specific and consistent with the tendency of recovery, in the patients with Bell’s palsy [23,24]. The effect of acupuncture stimulation may be part of the reason curing this kind of patients.
According to our experience and TCM theory, the proper duration for acupuncture treatment should be about 20 minute a time, and the frequency should be 2 to 3 times a week. Comparing to other pharmacologic therapy or surgical intervention, acupuncture has some advantages. The main advantages are that this is a simple and not expensive procedure. Besides, acupuncture is considered a relatively safe method of treatment with few side effects. Even though the odds are not high, the most possible side effects are bleeding, hematoma or feeling faint [25].
Based on TCM theory, there are nine meridian channel courses circulate through the whole face area. Bladder meridian runs from BL1 at the medial canthus of the eye, ascends the forehead to the vertex and then enters the brain and exits at the nape of the neck. Triple energizer meridian runs from TE1 at the ulnar side of the ring finger, travels along the midline of the posterior side of the arm and through the regions of the shoulder, neck, ear and eye, and terminates at TE23 at the lateral aspect of canthus. Gallbladder meridian runs from GB1 at the lateral canthus of the eye, through the regions of the temple, ear, neck, shoulder, flank, and the outer side of the lower limb, terminating at GB44 on the lateral side of the tip of the 4th toe. Large intestine meridian ascends the anterior lateral neck and the mandible, connects internally with the lower teeth, encircles the lips and terminates at the opposite LI20. Small intestine meridian ascends superficially along the lateral side of the neck, past the cheek to the lateral corner of the eye, and terminates at SI19. Stomach meridian originates internally at the lateral edge of the nose, then continues to ST1 at the inferior border of the orbit, descends to the upper gum, courses around the mouth, and travels up to ST8 at the hairline of the temple. Liver meridian ascends past the diaphragm along the trachea, larynx, sinus cavity, connecting with the eye, and then ascends to the vertex where it meets the governor vessel at GV20. Conception vessel is one of the eight extra meridians which originates in the lower abdomen, exists at CV1, a point in the center of perineum, and ascends the midline of the abdominal wall and chest to CV24, midpoint of the mentolabial sulcus. Governor vessel is also one of the eight extra meridians. The main portion of the meridian ascends along the midline of the back to the top of the head and then descends along the midline of the face down to GV28, a point between the upper lip and the upper gum in the labia frenum [26]. The most commonly used acupuncture points are shown in Table 1 and Figure 1.
|
Acupuncture point |
Location |
Direction |
|
GB20:Fengchi |
In the anterior region of the neck, inferior to the occipital bone, in the depression between the origins of sternocleidomas- toid and the trapezius muscles. |
Obliquely toward the other side eye |
|
TE17:Yifeng |
In the anterior region of the neck, Posterior to the ear lobe, in the depression anterior to the inferior end of the mastoid process. |
Obliquely toward the anterior mandible |
|
ST7:Xiaguan |
On the face, in the depression be- tween the midpoint of the inferi- or border of the zygomatic arch and the mandibular notch. |
Perpendicular to skin |
|
GB14:Yangbai |
On the head, 1B-cun superior to the eye-brow, directly superior to the centre of the pupil. |
Transversely toward the mid eyebrow |
|
BL2:Cuanzhu |
On the head, in the depression at the medial end of the eyebrow. |
Transversely toward TE23 |
|
TE23:Sizhukong |
On the head, in the depression at the lateral end of the eyebrow. |
Transversely toward BL2 |
|
ST4:Dicang |
On the face, 0.4 F-cun lateral to the angle of the mouth. |
Transversely toward ST6 |
|
ST6:Jiache |
On the face, one fingerbreadth (middle finger) anterosuperior to the angle of the mandible. |
Transversely toward ST4 |
|
LI20:Yingxiang |
On the face, in the nasolabial su- cus, at the same level as the mid- point of the lateral border of the ala of the nose. |
Obliquely along the nasolabial |
|
Sulcus toward the root of the nose |
||
|
GV26:Shuigou |
On the face, at the junction of the upper one third and lower two thirds of the philtrum mid- line. |
Perpendicular to skin |
|
CV24:Chengjiang |
On the face, in the depression in the centre of the mentolabial sulcus. |
Perpendicular to skin |
|
LI4:Hegu |
On the dorsum of the hand, ra- dial to the midpoint of the sec- ond metacarpal. |
Perpendicular to skin |
|
LI11:Quchi |
On the lateral aspect of the el- bow, at the midpoint of the line connecting LU5 with the later- al epicondyle of the humerus. When the elbow is fully flexed, LI11 is located in the depression on the lateral end of the cubital crease. |
Perpendicular to skin |
|
TE5:Waiguan |
On the posterior aspect of the forearm, midpoint of the inter- osseous space between the radius and the ulna, 2 B-cun proximal to the dorsal wrist crease. |
Perpendicular to skin |
|
ST40:Fenglong |
On the anterolateral aspect of the leg, lateral border of the tib- ialis anterior muscle, 8 B-cun su- perior to the prominence of the lateral malleolus. |
Perpendicular to skin |
Table 1: VAS Numeric Pain Distress Scale (NPRS) was used to evaluate the patient’s pain. The NPRS is an 11-point scale from 0-10 with 0 being no pain and 10 being the most intense pain imaginable.
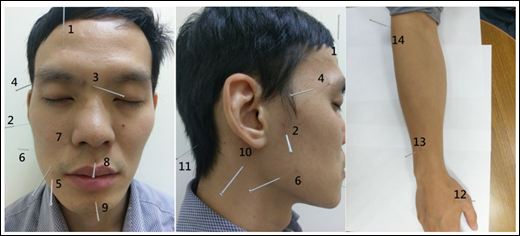
Figure 1: 1.GB14:Yangbai, 2. ST7:Xiaguan, 3. BL2:Cuanzhu, 4. TE23:Sizhukong, 5. ST4:Dicang, 6. ST6:Jiache, 7. LI20:Yingxiang, 8. GV26:Shuigou, 9. CV24:Chengjiang, 10. TE17:Yifeng, 11. GB20:Fengchi, 12. LI4:Hegu, 13. TE5:Waiguan, 14. LI11:Quchi.
According to our clinical observation, the time point of acupuncture intervention after the onset of Bell’s palsy is also a critical factor affecting the severity of sequelae and the length of treatment till a satisfactory extent. It is highly expected more sophisticated researches are executed to elaborate these clinical findings in the future.
Conclusion
Even thought high quality RCTs and clinical evidence are appreciated, current researches and results suggest that acupuncture plays a crucial role in the Bell’s palsy treatment. In addition, acupuncture does relieve Bell’s palsy sequelae and improve outcome of these patients.
References
- Chen N, Zhou M, He L, Zhou D, Li N (2010) Acupuncture for Bell’s palsy. Cochrane.
- May M, Klein SR (1991) Differential diagnosis of facial nerve palsy. Otolaryn- gol Clin North Am 24: 613-645.
- Peitersen E (1982) The natural history of Bell’s Am J Otol 4: 107-111.
- Morris AM, Deeks SL, Hill MD, Midroni G, Goldstein WC, et al. (2002) An- nualized incidence and spectrum of illness from an outbreak investigation of Bell’s Neuroepidemiology 21: 255-261.
- Zhao H, Zhang X, Tang YD, Zhu J, Wang XH, et al. (2017) Bell’s Palsy: Clinical Analysis of 372 Cases and Review of Related Literature. Eur Neurol 77:168-172.
- Peitersen E (2002) Bell’s palsy: the spontaneous course of 2,500 peripheral facial nerve palsies of different Acta Otolaryngol Suppl 549: 4-30.
- Beurskens CH, Heymans PG (2006) Mime therapy improves facial symmetry in people with long-term facial nerve paresis: a randomised controlled trial. Aust J Physiother 52: 177-183.
- Devriese PP (1998) Treatment of sequelae after facial paralysis: a global J Laryngol Otol 112: 429-431.
- Tseng CC, Hu LY, Liu ME, Yang AC, Shen CC, et al. (2017) Bidirectional association between Bell’s palsy and anxiety disorders: A nationwide popula- tion-based retrospective cohort J Affect Disord 215: 269-273.
- Gronseth GS, Paduga R American Academy of Neurology (2012) Evi- dence-based guideline update: steroids and antivirals for Bell palsy: report of the Guideline Development Subcommittee of the American Academy of Neurology 79: 2209-2213.
- de Almeida JR, Guyatt GH, Sud S, Dorion J, Hill MD, et al. (2014) Manage- ment of Bell palsy: clinical practice CMAJ 186: 917-922.
- McAllister K, Walker D, Donnan PT, Swan I (2013) Surgical interventions for the early management of Bell’s Cochrane Database Syst.
- Cayir Y, Set T, Akturk Z (2013) The Effect of Acupuncture in a Patient with Bell’s Palsy: A Case Report. Eurepean Journal of Oriental Medicine 7: 46-47.
- MacPherson H, Thomas K, Walters S, Fitter M (2001) A prospective survey of adverse events and treatment reactions following 34,000 consultations with professional Acupunct Med 19: 93-102.
- Li P, Qiu T, Qin C (2015) Efficacy of Acupuncture for Bell’s Palsy: A System- atic Review and Meta-Analysis of Randomized Controlled Trials. PLoS One 10:0121880.
- Lee J, Yang J, Li C, Yuan A, Wu H, et al. (2016) Cortical Reorganization in Patients Recovered from Bell’s Palsy: An Orofacial and Finger Movements Task-State fMRI Neural Plasticity 2016:8231726.
- Wu H, Kan H, Li C, Park K, Zhu Y, et al. (2015) Effect of Acupuncture on Functional Connectivity of Anterior Cingulate Cortex for Bell’s Palsy Patients with Different Clinical Duration. Evidence-Based Complementary and Alter- native Medicine 2015:646872.
- Eviston TJ, Croxson GR, Kennedy PG, Hadlock T, Krishnan AV (2015) Bell’s palsy: aetiology, clinical features and multidisciplinary care. J Neurol Neuro- surg Psychiatry 86:1356-1361.
- Beurskens CH, Heymans PG (2003) Positive effects of mime therapy on sequelae of facial paralysis: stiffness, lip mobility, and social and physical aspects of facial Otol Neurotol 24: 677-681.
- Kwon HJ, Choi JY, Lee MS, Kim YS, Shin BC, (2015) Acupuncture for the sequelae of Bell’s palsy: a randomized controlled Trials 16:246.
- He S, Zhang H, Liu R, (1995) Review on acupuncture treatment of peripheral facial paralysis during the past J Tradit Chin Med 15: 63-67.
- Ren X, (1994) A survey of acupuncture treatment for peripheral facial paral- J Tradit Chin Med 14: 139-146.
- Bian Y, He X, Hu S, Li C, Xu C, et al. (206) Functional Connectivity Modulation by Acupuncture in Patients with Bell’s Palsy. Evidence-Based Complementary and Alternative Medicine 2016:5928758.
- He X, Zhu Y, Li C, Park K, Mohamed AZ, et al. (2014) Acupuncture-induced changes in functional connectivity of the primary somatosensory cortex varied with pathological stages of Bell’s Neuroreport 25: 1162-1168.
- Odsberg A, Schill U, Haker E, (2001) Acupuncture treatment: side effects and complications reported by Swedish physiotherapists. Complement Ther Med 9:17-20.
- Organization WH, (2007) WHO international standard terminologies on traditional medicine in the western pacific region. WHO Regional Office for the Western Pacific, Manila.
Citation: Wu SH, Tai CJ (2017) Current Research in Acupuncture Treatment for Bell’s Palsy. J Acupun Tradit Med 1: 001.
Copyright: © 2017 Tai CJ. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.