*Corresponding Author:
Jingping Wang,
Department of Anesthesia, Cancer Hospital Chinese Academy of Medical Sciences 17 Panjiayuannanli, Chaoyang District, Beijing, China
Email: Jwang23@MGH.Harvard.edu
Abstract
Pain management has always been a very important medical service, improving the quality of life of patients with acute or chronic pain. Opioids, which are one of the most important medicines in pain management, have now been widespread used. Meanwhile, opioid crisis emerged, becoming a serious social problem in many countries. The COVD-19 pandemic is another crisis for all human being. The panic, social isolation and economic problems caused by COVID-19 can cause people a lot of suffer, especially patients with pain problem and opioid abusers, leading to an increase in the demand for opioids. COVID-19 itself can cause myalgia and hyperalgesia, and the current controversy over the negative effects of NSAIDs on COVID-19 has made many doctors prefer to use opioids for pain management. Various medical restrictions during the pandemic led to insufficient instruction on opioid management for patients. Various reasons have made the opioid crisis worse during the COVID-19 pandemic. On the other hand, people who live in the opioid crisis, due to their own basic body condition and living habits, are more likely to get infected, and the impact of long-term opioid use on their body can worsen the prognosis. The immunosuppressive effect of some opioids also makes the treatment of COVID-19 more difficult. In 2020, these two crises are intertwined and aggravate each other. In this review we discuss this status and some possible countermeasures hoping to help solve those problems to some extent.
Keywords
Immunosuppression; Nonsteroidal Anti-inflammatory Drugs (NSAIDs); Novel Coronavirus Disease 2019 (COVID-19); Opioids Crisis; Pandemic
Introduction
The concept of “pain as the fifth vital sign” was once widely popular, and doctors have an obligation to alleviate patients’ pain to the greatest extent. Gradually, indications of opioids have expanded from cancer and palliative care to other areas, such as postoperative acute/ chronic pain and other non-cancer pain [1]. About 128 people die because of opioids overdose every day in the United States [2]. Taking 2018 as an example, opioids related deaths accounted for about 70% of all drug overdose deaths (n=46,802) [3]. Moreover, it has been reported that among patients with high-dose opioids or opioid use disorders there may be potentially increased morbidity and mortality [3,4], with approximately 21% to 29% of patients being prescribed opioids for chronic pain and misusing them and 8% to 12% of patients showing an opioid use disorder [2]. Over the past 20 years, multiple modalities in pain management have shown a significant increase in the use of opioids, with opioid epidemic aggravated and opioid-related deaths escalated [3-5]. The current public health crisis, the COVID-19 pandemic, may further aggravate the opioid crisis.
Coronavirus disease 2019 (COVID-19) is an outbreaking infectious disease caused by a newly discovered coronavirus, has now spread globally. World Health Organization (WHO) has declared the novel coronavirus (COVID-19) outbreak a global pandemic on March 11, 2020 [6]. Until November 12, 2020, 51,547,733 confirmed cases, 1,275,979 death and 220 countries, areas or territories of novel coronavirus (COVID-19) have been reported by WHO [7]. Both of infection and death numbers are expected to continue to rise. As winter is approaching, COVID-19 pandemic may aggravate, considering the virus stays more stable and longer at low temperatures in dry air, while the host’s immunity system is weaker [8].
Research works on the COVID-19 vaccine have been started and it was predicted before that it would take 1.5-2 years to develop an effective vaccine [9]. However, on November 9, 2020, Pfizer and BioNTech announced that the mRNA-based vaccine candidate, BNT162b2, against COVID-19 succussed in first interim analysis from Phase 3 study. It was said that 94 cases of COVID-19 were identified among 43,538 trial participants and suggested that the vaccine was more than 90% effective at preventing disease. The Clinical trial will continue collect further data until 164 cases were confirmed [10]. Although more detail information is needed, for example, the nature of the target infections, the lasting vaccine effectiveness, it is still a great achievement [11].
The COVID-19 pandemic has not only brought many epidemiological and medical problems, but also a series of social and economic challenges. Quarantine and financial crisis have led to a series of mental and psychological problems [12], such as anxiety, sleep disorders, panic and pessimism [12,13]. Patients with opioid dependence and addicted patients may feel more distressed [13] that worsen the existing opioid crisis.
This review discusses that the current COVID-19 pandemic and opioid crisis are impacting and worsening each other in different ways, meanwhile, provides further understanding to face the great worldwide challenge and explores the possible solutions.
COVID-19
Novel Coronavirus Disease 2019 (COVID-19) is a human b-coronavirus that has been renamed as Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). COVID-19 has become a global pandemic. The main early symptoms of COVID-19 patients are fever and cough. On admission chest CT examination, 86.2% showed abnormal results and the most common patterns were ground-glass opacity (56.4%) and bilateral patchy shadowing (51.8%) [14]. A large proportion of patients suffer from Acute Respiratory Distress Syndrome (ARDS) [15]. In addition to viral pneumonia, COVID-19 is also associated with extrapulmonary manifestations and complications. There were 83.2% patients with lymphopenia, 36.2% with thrombocytopenia, and 33.7% with leukopenia at admission [14]. Laboratory abnormalities including lymphopenia and leukopenia in severe patients are more prominent than in non-critically ill patients [14], suggesting significant changes in immune function of COVID-19 patients in addition to respiratory system changes, and cardiovascular damage. Gastrointestinal symptoms of patients with COVID-19, such as acute abdominal pain [16], are also receiving increasing attention. In addition, some COVID-19 patients experience mild to moderate physical pain, which may be related to long-term bed rest and psychological stress. It has been shown that dozens of patients in the pain clinic complain of physical pain without respiratory symptoms while their COVID-19 test is positive [17], indicating that physical pain may be one of the early symptoms of COVID-19 infection.
Opioids
Pain management services still need to run during the epidemic, although many adjustments need to be made in the deployment of health care workers, transmission protection and protocol of medical procedures. Opioids remain one of the most important and commonly used drugs in pain management.
Some side effects of opioids are well known, such as dose-related respiratory depression, nausea and vomiting. In addition, it is necessary to consider the impact of opioids on the immune system for COVID-19 patients [18]. A series of in vitro/in vivo tests have shown that opioids, such as morphine, can affect the innate and acquired immune functions negatively. Opioid receptors are widely distributed in the peripheral and central nervous system and include the classic naloxone-sensitive receptors, µ Opioid Receptor (MOR), ∂ Opioid Receptor (DOR), κ Opioid Receptor (KOR), and non-classic naloxone-insensitive receptors (NORs) [19]. All receptors play an analgesic role, and only MORs is believed to be associated with respiratory depression, opioid tolerance, and immunosuppression [19-22]. Opioids regulate the immune system in several aspects.
Cellular immunity: The activation of opioid receptors leads to a reduction in the number of macrophages, a decrease in phagocytic activity, and accelerated apoptosis. Leukocyte migration and the adhesion of leukocytes to endothelial cells are reduced. The functions of mast cells, dendritic cells and natural killer cells are also down regulated [19]. At the same time, opioids increase the apoptosis of Th1 cells in T helper cell (Th), increase the differentiation of Th2 cells, and decrease the ratio of Th1 to Th2.
Humoral immunity: The concentration of IL-ß, IL-2, TNF-α and IFNγ is decreased. Antibody production by B cells is reduced, as is the expression of tissue compatibility factors and proliferation [19]. Opioids activate Toll-like receptors on the surface of the intestinal ep- ithelium, then impair the intestinal barrier function and lead to risk of systemic infection [19]. By activating the neuroendocrine axis of the thalamus-Pituitary-Adrenal (HPA) axis and stimulating the production of glucocorticoids, opioids indirectly inhibit the NK cell cytotoxicity and lymphatic proliferation [19]. Another mechanism of opioid-induced immunosuppression is related to oxidative stress and Reactive Oxygen Species (ROS) function [19].
Not all opioids have the same immunosuppressive effect. Codeine, methadone, morphine, fentanyl, sufentanil and remifentanil have strong regulatory effects [19], while oxycodone, tramadol and hydromorphone are weaker. Buprenorphine has the least immunosuppressive effect [19]. Moreover, in a surgical stress model [22], buprenorphine can prevent biochemical and immune changes caused by pain. Buprenorphine may be used as a first-line analgesic in patients who need special attention to their immune system [19,23].
The immunosuppressive effect of opioids is clinically evident. Compared with total intravenous anesthesia using propofol and paravertebral anesthesia with bupivacaine, combined general anesthesia with opioids increased MOR expression in breast tumor tissues [19,24]. In another study, the total daily dose of opioids was an independent factor which affected infection risks in cancer patients receiving opioid monotherapy [19,25].
Pain is a comprehensive reflection of physiology and psychology, and it adversely affects the immune system. The state of the immune system is equilibrium of the combined effects of pain and drugs. Generally, patients in good condition can tolerate a mild degree of immunosuppression. However, in some cases, patients may have severe infections or immune disorders, such as elderly and COVID-19 patients, and immunosuppression due to opioids can be dangerous. Therefore, it is advisable to avoid opioids having a clear immunosuppressive effect (such as morphine and fentanyl) and choose those having no or little effect on the immune system (such as tramadol and buprenorphine).
Opioid Crisis on COVID-19 Pandemic
Opioid crisis aggravates COVID-19 infection in several ways. Patients with acute or chronic pain that need opioids for pain management often suffer from a series of basic medical condition, such as immunocompromised or elderly patients, cardiopulmonary disease, metabolic disease, arthritis or undergoing surgeries, that makes them more susceptible to infection and an increased mortality. Further, people who are treated with opioids for a long period are more likely to develop cardiopulmonary and neurological complications, which worsen the prognosis of COVID-19 [26,27]. As mentioned above, some opioids were immunosuppressive to varying degrees [28,29], and this also makes patients use opioids in a long term, with a large dose or with disorders, an increased risk of infection. Moreover, an overdose of opioids can cause respiratory depression and hypoxemia, which makes problems even worse. People with opioid problems are more likely to gather or have parties for their common demand and lead a wandering life with housing instability, that also facilitate the infection and spread of pneumonia [26,30]. Recent reports have shown that COVID-19 infection is associated with myalgias, referred pain, and widespread hyperalgesia [31]. For opioid-dependent patients infected with COVID-19, they are more likely to use opioids when they get the above symptoms, masking the symptoms of COVID-19. Postponed or cancelled medical consultation due to the purpose of limiting the spread of infection may further because delayed diagnosis and treatment, worsening the prognosis.
COVID-19 Pandemic on Opioid Crisis
Social and psychological problems: the COVID-19 pandemic has had a huge impact on people’s work, life, and physical and mental health in 2020. The increasing number of infections and deaths, and all kinds of news about the disease inevitably caused people to worry, fear and panic. Many countries and regions have implemented a series of policies of quarantine to limit the spread of infection. Longterm social isolation, alienation, and loneliness have all led to a series of psychological symptoms, including but not limited to depression and anxiety [26]. Working at home, lower incomes, fear of unemployment and uncertainty about the future-economic pressure is another source of psychological problems [26]. People may be more likely to seek opioids not for pain management but to help reduce stress and escape reality. For people with opioid disorders, psychological problems may be more serious, which in turn makes the opioid disorders even worse.
Patients: some COVID-19 patients, in addition to symptoms of the respiratory, circulatory and immune system abnormalities, may have acute abdominal pain or physical pain of varying degrees, and pain service is necessary [16]. Medical comorbidities, like cardiopulmonary disease and depression, can increase the risk of postoperative long-term opioid use [32]. Furthermore, the hospital stay of COVID-19 patients may be long, and as the duration of opioids treatment increases, the incidence of long-term opioid dependence may be higher. Patients undergoing opioids for over 90 days are more likely to receive chronic opioid therapy [33]. For non-COVID-19 patients, pain itself limits daily activities and reduces the quality of life. The pandemic aggravates these negative effects, as the quarantine, tremendous changes in living and working conditions, and may worsen the opioid abuse.
Controversy on non-opioids: NSAIDs are often used as the first-line multimodal postoperative pain medicine for patients. For COVID-19 patients, the safety of using NSAIDs is controversial. It has been reported that there were cases of COVID-19 patients getting worse after using ibuprofen and the anti-inflammatory properties of ibuprofen may make pneumonia worse [34]. Patients may be more susceptible to adverse effects of NSAIDs on severe infection, but there was no specific evidence [35]. It is assumed that NSAIDs may be associated with upregulation of the ACE2 receptors, presumptively via which the SARS-CoV-2 virus invades human cells [36,37]. Moreover, some NSIADs, such as ibuprofen may associated with immune suppression in COVID-19 patients [36,38]. On the other hand, it is reported that cytokine storm seems plays an important role in adverse outcomes of severely ill patients, while the NSAIDs’ anti-inflammatory property may be beneficial in preventing body’s system form the overwhelm of inflammation system [36,39]. Currently, insufficient evidence exists to support whether NSAIDs should be used on patients with or without COVID-19 [31,40]. However, it is commonly accepted that NSAIDs may delay the diagnosis management of COVD-19 infection by cover the symptom of fever and myalgia because of its antipyretic property [31,41]. Until there is a clear conclusion, doctors may tend to be cautious or avoid using NSAIDs as the first choice for pain management, and that makes opioids a priority and increases the consumption of opioids.
Medical protocol changes: Timely medical consultation and treatment are essential to accurately suspend and instruct the use of opioids, which may be difficult during the COVID-19 epidemic. Nearly all the medical systems are focusing on limiting the spread of infection. Elected outpatient clinics and medical procedures, including pain management, have to be postponed or cancelled. Many patients have complex analgesia needs and require comprehensive medical interventions [31]. The interruption or cancellation of pain management services may result in huge changes in patients’ medications. Patients may suffer from more pronounced cravings and withdrawal effects, which may be life-threatening [26]. As a result, patients may seek drugs on their own via varies non-medical ways and tend to be uncontrollable. For transmission control reasons, communicating with patients through telephone, video and electronic systems have become the choice of clinic and following-up. Lack of full communication and physical examination, the accuracy of assessment, the education of the patient and efficiency monitoring will be affected. Some temporary policies including permission of prescribing opioid prescriptions via telemedicine and prolonging the validity of prescriptions [42] may facilitate to obtain extra opioids. Although most of the guidelines were aimed at proper opioid use, the recommended doses in the guidelines may be excessive and promote opioid abuse due to the opioid industry’s interest reasons [3,43]. With the COVID-19 pandemic, doctors may tend to allow patients do self-administration at home and adjust the dosage by themselves, and remain the original prescriptions, of initial dose based on guidelines, resulting in lengthy prescriptions and high doses whereas the reduction and withdrawal of opioids may be delayed. The impact of the epidemic on medical procedures and protocols makes it worrisome resulting in increased consumption and death rates.
Some Countermeasures
Acetaminophen may be a non-opioid option, safer than ibuprofen [34]. It has analgesic and antipyretic effects and also inhibits production of prostaglandins without anti-inflammatory effects [44,45]. Acetaminophen is a prime choice for patients who cannot use NSAIDs, such as those with asthma, peptic ulcer disease, hemophilia, or salicylate-sensitivity [44]. With appropriate dose (maximum dose 4g/24h), no serious side effects have been found except for allergic skin rash [44,46]. Therefore, in most patients, who may include COVID-19 patients without severe liver function abnormality, the recommended dose of acetaminophen is less likely to cause serious adverse reactions than NSAIDs.
With proper personal protective equipment, regional blockade including peripheral nerve block and neuraxial anesthesia is still a better choice to reduce opioid consumption. Efficacy as well as cost utility of interventional techniques in general and facet joint interventions in particular have been proven by plenty of studies [5].
It has many benefits, including less impact on respiratory function and reduced postoperative pulmonary complications, which is important for COVID-19 patients. Regional anesthesia can also reduce postoperative nausea and vomiting and postoperative cognitive dysfunction [47], thereby reducing possible infectious aerosol production. It induces little inhibition on the cardiovascular system and little influence on the immune system. By reducing intraoperative and postoperative pain [48], it can also reduce the dose of potentially deleterious opioids. In addition, for intraoperative opioids may affect the diagnostic validity of facet joint nerve blocks, it is even moderately recommended to avoid opioids [3]. Evidence showed that in terms of the diagnostic effectiveness of the controlled comparative local anesthetics, there was no correlation with previous and current opioid use [3,49] and using opioids may even cause failure of the treatment of lumbar radiofrequency neurotomy [3,50]. It is worth noting that, given the fact that the Covid-19 patient may experience significant coagulopathy, coagulation tests may be needed for regional anesthesia [51].
Telemedicine is widely used in both outpatient and inpatient clinic follow-up during pandemics. Improving electronic systems, forms and plans may help standardize opioid managements including selection, dosage, duration, follow-up and withdrawal. Appropriately increasing the frequency of follow-up by telephone or the web may help in educating and guiding patients to use analgesics properly.
It is worth noting that in addition to direct treatment and medical procedures, mental and psychological consultation, sleep quality, nutritional support and excise also play a role in pain relief and avoidance of opioid abuses. During COVID-19 period, cooperation and multidiscipline care is very important for satisfactory pain control without aggravating the opioid crisis.
Conclusion
COVID-19 pandemic is a public health problem and, due to medical and patient reasons, the opioid crisis may be worsened. However, whether for the COVID-19 or other patients, pain treatment services are still necessary. Some adjustments can be made to minimize the dosage of opioids or avoid their use (Table 1). More efforts should be made to control the opioid crisis as much as possible while preventing the epidemic.
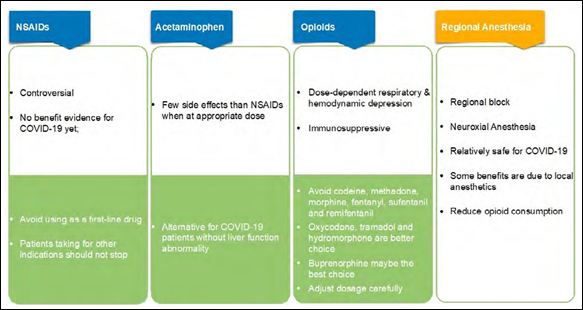
Table 1: Considerations and advices for pain managements during COVID-19.
References
- Vadivelu N, Kai AM, Kodumudi V, Sramcik J, Kaye AD (2018) The opioid crisis: A comprehensive Curr Pain Headache Rep 22: 16.
- NIDA (2018) Opioid overdose crisis. National Institute on Drug Abuse, Maryland, USA.
- Manchikanti L, Kaye AD, Soin A, Albers SL, Beall D, et al. (2020) Com- prehensive evidence-based guidelines for facet joint interventions in the management of chronic spinal pain: American Society of Interventional Pain Physicians (ASIPP) guidelines facet joint interventions 2020 guide- Pain Physician 23: 1-127.
- Alexander GC, Stoller KB, Haffajee RL, Saloner B (2020) An epidemic in the midst of a pandemic: Opioid use disorder and COVID-19. Ann Intern Med.
- Manchikanti L, Pampati V, Soin A, Vanaparthy R, Sanapati MR, et al. (2020) Trends of expenditures and utilization of facet joint interventions in Fee-For-Service (FFS) Medicare population from 2009-2018. Pain Phy- sician 23: 129-147.
- Cucinotta D, Vanelli M (2020) WHO declares COVID-19 a pandemic. Acta Biomed 91: 157-160.
- World Health Organization (2020) Coronavirus disease (COVID-19) pan- World Health Organization, Geneva, Switzerland.
- Kundu A, Basu S, Shetti NP, Malik AK, Aminabhavi TM (2020) The COVID-19 paradox: Impact on India and developed nations of the world. Sensors International 1: 100026.
- Shetti NP, Srivastava RK, Sharma S, Basu S, Aminabhavi TM (2020) Inva- sion of novel corona virus (COVID-19) in Indian territory. Sensors Inter- national 100012.
- Pfizer (2020) Pfizer and biontech announce vaccine candidate against COVID-19 achieved success in first interim analysis from phase 3 study. Pfizer, New York, USA.
- Nature (2020) What Pfizer’s landmark COVID vaccine results mean for the pandemic.
- Sharma S, Basu S, Shetti NP, Aminabhavi TM (2020) Current treatment protocol for COVID-19 in Sensors International 1: 100013.
- Sharma S, Kundu A, Basu S, Shetti NP, Aminabhavi TM (2020) Indians vs. COVID-19: The scenario of mental Sensors International 1: 100038.
- Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, et al. (2020) China medical treatment expert group for clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 382: 1708-1720.
- Madjid M, Safavi-Naeini P, Solomon SD, Vardeny O (2020) Potential effects of coronaviruses on the cardiovascular system: A JAMA Cardiol 5: 831-840.
- Poggiali E, Ramos PM, Bastoni D, Vercelli A, Magnacavallo A (2020) Ab- dominal pain: A real challenge in novel COVID-19 infection. Eur J Case Rep Intern Med 7: 001632.
- Song XJ, Xiong DL, Wang ZY, Yang D, Zhou L, et al. (2020) Pain man- agement during the COVID-19 pandemic in China: Lessons learned. Pain Med 21: 1319-1323.
- Guo YR, Cao QD, Hong ZS, Tan YY, Chen SD, et (2020) The origin, trans- mission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak-an update on the status. Military Medical Research 7: 11.
- Kosciuczuk U, Knapp P, Lotowska-Cwiklewska AM (2020) Opioid-in- duced immunosuppression and carcinogenesis promotion theories create the newest trend in acute and chronic pain pharmacotherapy. Clinics (Sao Paulo) 75:1554.
- Machelska H, Stein C (2002) Immune mechanisms in pain Anesth Analg 95: 1002-1008.
- Kwiatkowski K, Mika J (2018) The importance of chemokines in neuro- pathic pain development and opioid analgesic Pharmacol Rep 70: 821-830.
- Sacerdote P (2008) Opioid-induced immunosuppression. Curr Opin Sup- port Palliat Care 2: 14-18.
- Davis MP (2012) Twelve reasons for considering buprenorphine as a front- line analgesic in the management of J Support Oncol 10: 209-219.
- Levins KJ, Prendeville S, Conlon S, Buggy DJ (2018) The effect of anesthetic technique on micro-opioid receptor expression and immune cell infiltra- tion in breast J Anesth 32: 792-796.
- Shao YJ, Liu WS, Guan BQ, Hao JL, Ji K, et (2017) Contribution of opiate analgesics to the development of infections in advanced cancer patients. Clin J Pain 33: 295-299.
- Dubey MJ, Ghosh R, Chatterjee S, Biswas P, Chatterjee S, et al. (2020) COVID-19 and Diabetes Metab Syndr 14: 817-823.
- Becker WC, Fiellin DA (2020) When epidemics collide: Coronavirus dis- ease 2019 (COVID-19) and the opioid Ann Intern Med 173: 59-60.
- Tindle HA, Newhouse PA, Freiberg MS (2020) Beyond smoking cessation: Investigating medicinal nicotine to prevent and treat COVID-19. Nicotine Tob Res 22: 1669-1670.
- Leung JM, Yang CX, Sin DD (2020) Current smoking is not associated with COVID-19. Eur Respir J 55: 2001290.
- Schulte MT, Hser YI (2014) Substance use and associated health conditions throughout the Public Health Rev 35.
- El-Tallawy SN, Nalamasu R, Pergolizzi JV, Gharibo C (2020) Pain manage- ment during the COVID-19 Pain Ther 9: 453-466.
- Hah JM, Bateman BT, Ratliff J, Curtin C, Sun E (2017) Chronic opioid use after surgery: Implications for perioperative management in the face of the opioid Anesth Analg 125: 1733-1740.
- Martin BC, Fan MY, Edlund MJ, Devries A, Braden JB, et al. (2011) Long- term chronic opioid therapy discontinuation rates from the TROUP study. J Gen Intern Med 26: 1450-1457.
- Day M (2020) Covid-19: Ibuprofen should not be used for managing symp- toms, say doctors and BMJ 368: 1086.
- FitzGerald GA (2020) Misguided drug advice for COVID-19. Science 367:1434.
- Pergolizzi JV, Varrassi G, Magnusson P, LeQuang JA, Paladini A, et al. (2020) COVID-19 and NSAIDS: A narrative review of knowns and un- Pain Ther 9: 353-358.
- Zou X, Chen K, Zou J, Han P, Hao J, Han Z (2020) Single-cell RNA-seq data analysis on the receptor ACE2 expression reveals the potential risk of different human organs vulnerable to 2019-nCoV infection. Front Med 14: 185-192.
- Fang L, Karakiulakis G, Roth M (2020) Antihypertensive drugs and risk of COVID-19? - Authors’ Lancet Respir Med 8: 32-33.
- Zhang W, Zhao Y, Zhang F, Wang Q, et (2020) The use of anti-inflamma- tory drugs in the treatment of people with severe coronavirus disease 2019 (COVID-19): The Perspectives of clinical immunologists from China. Clin Immunol 214: 108393.
- Day M (2020) Covid-19: European drugs agency to review safety of ibu- BMJ 368: 1168.
- Favalli EG, Ingegnoli F, De Lucia O, Cincinelli G, Cimaz R, et al. (2020) COVID-19 infection and rheumatoid arthritis: Faraway, so close! Autoim- mun Rev 19:102523.
- Shanthanna H, Strand NH, Provenzano DA, Lobo CA, Eldabe S, et al. (2020) Caring for patients with pain during the COVID-19 pandemic: con- sensus recommendations from an international expert panel. Anaesthesia 75: 935-944.
- Manchikanti L, Sanapati J, Benyamin RM, Atluri S, Kaye AD, et (2018) Reframing the prevention strategies of the opioid crisis: Focusing on pre- scription opioids, fentanyl, and heroin epidemic. Pain Physician 21: 309- 326.
- Jozwiak-Bebenista M, Nowak JZ (2014) Paracetamol: mechanism of ac- tion, applications and safety Acta Pol Pharm 71: 11-23.
- Mattia A, Coluzzi F (2009) What anesthesiologists should know about paracetamol (acetaminophen). Minerva Anestesiol 75: 644-653.
- Graham GG, Scott KF, Day RO (2005) Tolerability of paracetamol. Drug Safety 28: 227-240.
- Lie SA, Wong SW, Wong LT, Wong TGL, Chong SY (2020) Practical con- siderations for performing regional anesthesia: Lessons learned from the COVID-19 Can J Anaesth 24: 1-8.
- Lirk P, Hollmann MW (2014) Outcome after regional anesthesia: Weighing risks and Minerva Anestesiol 80: 610-618.
- Manchikanti L, Boswell MV, Manchukonda R, Cash KA, Giordano J (2008) Influence of prior opioid exposure on diagnostic facet joint nerve J Opioid Manag 4: 351-360.
- Cohen SP, Moon JY, Brummett CM, White RL, Larkin TM (2015) Medial branch blocks or intra-articular injections as a prognostic tool before lum- bar facet radiofrequency denervation: A multicenter, case-control study. Reg Anesth Pain Med 40: 376-383.
- Yang Y, Soh HY, Cai ZG, Peng X, Zhang Y, et al. (2020) Experience of di- agnosing and managing patients in oral maxillofacial surgery during the prevention and control period of the new coronavirus pneumonia. Chin J Dent Res 23: 57-62.
Citation: Zhang M, Zheng H, Wang J (2020) Considerations When COVID-19 Pan- demic Collides Opioid Crisis: What We Should Know? J Anes Perio Manag 4: 009.
Copyright: © 2020 Zhang M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.