*Corresponding Author:
Thiago Mamoru Sakae,
Anesthesiologist, PhD in Medical Sciences, Epidemiology professor - Universidade do Sul de Santa Catarina, Tubarão, Santa Catarina, Brazil
Email: thiagosakae@gmail.com
Abstract
Purpose: Laryngoscopy and orotracheal intubation are invasive procedures that can generate tachycardia, systemic arterial hypertension and arrhythmias. This study compares the effects of esmolol, magnesium sulfate and placebo on this potential hemodynamic response.
Methods: Randomized, double-blind clinical trial evaluating patients between 18 and 65 years, ASA I or II, requiring general anesthesia and orotracheal intubation for elective surgery. Subjects were divided into three groups: group E received 1.5 mg/kg of intravenous esmolol, group M 30 mg/kg intravenous magnesium sulfate, and group C receiving placebo prior to anesthetic induction. Blood pressure and heart rate values were recorded in five moments related to drug administration and intubation.
Results: 45 participants were included in the study. Group E was the only group that maintained stable heart rate in relation to baseline at all times. Group M had the highest mean systolic blood pressure after intubation between groups E and C (p=0.002 and p=0.003, respectively). The systolic blood pressure of the M group was higher than the group E at different times.
Conclusion: A bolus of 1.5 mg/kg esmolol three minutes before intubation was able to attenuate the hypertensive response to orotracheal intubation, being more effective than 30 mg/kg of magnesium sulfate infused ten minutes before anesthetic induction, but with more frequent hypotension.
Keywords
Laryngoscopy; Endotracheal intubation; Beta-adrenergic antagonists; Magnesium sulfate; Cardiovascular physiological phenomena
Introduction
Airway manipulation with laryngoscopy and Orotracheal Intubation (OTI) results in reflex sympathetic activity, characterized primarily by systemic arterial hypertension and tachycardia. This response is justified by the mechanical stimulation of the pharynx and larynx, leading to an increase in plasma levels of epinephrine and norepinephrine [1-4]. Such response is usually transient and varies in presentation, being unpredictable most of the time [1,5]. It is well tolerated by healthy individuals, but may be responsible for adverse events in others, such as: arrhythmias, myocardial ischemia, acute myocardial infarction and cerebral hemorrhage [4,5]. Patients with diabetes mellitus, cerebrovascular diseases, coronary artery disease, systemic arterial hypertension, heart failure and previous arrhythmias, in addition to the geriatric population, are at greater risk for these events [5,6].
In order to attenuate the hemodynamic response to the intubation process, the effects of medications such as esmolol and magnesium sulfate have been studied [5,7-11]. Esmolol is a cardio selective beta-blocker with the potential to prevent possible clinical sequelae related to increased hemodynamic parameters during OTI. Its use for this purpose is well established [5,7,8]. Magnesium sulfate inhibits release of catecholamines by the adrenal medulla and has a systemic and coronary vasodilator effect by antagonizing the calcium ion in vascular smooth muscle. It has a modulating effect on sodium and potassium channels, influencing cell membrane potential, and it also has a depressant effect on the central nervous system by antagonizing N-methyl-D-aspartate (NMDA) receptors [11,12].
The main objective of this study was to compare the effects of intravenous administration of esmolol, magnesium sulfate and placebo on the hemodynamic changes due to OTI.
Methods
This is a prospective randomized, parallel, double-blind clinical trial was patients undergoing to non-cardiac surgery with general anesthesia and orotracheal intubation. This study was approved by the Research Ethics Committee of the Universidade do Sul de Santa Catarina, (Protocol No. 2,205,064). It is included in the Brazilian Registry of Clinical Trials under the code RBR-8spKx9.
Were included patients submitted to elective surgeries under general anesthesia and endotracheal intubation in a teaching hospital between December 2016 and September 2017?
The minimum required sample of 30 patients was calculated using the OpenEpi 3.01 [13] software, considering the prevalence of non-exposed 40% positive, 90% positive exposed and 95% significance level. Randomization was performed by computer program, dividing patients into 3 groups: group E, those receiving 1.5 mg/kg esmolol; group M, those who would receive 30 mg/kg of magnesium sulfate and group C, who would not receive either drug. After randomization, sealed and numbered brown envelopes were prepared containing paper with the name of the group to which the patient belonged.
Patients included in the study were classified by the American Society of Anesthesiology (ASA) I and II, both genders, aged between 18 and 65 years, who underwent general anesthesia with OTI and agreed to participate in the study with consent of the Free Consent Term and Enlightened. The exclusion criteria were: patients with difficult predicted airway, Body Mass Index (BMI) ≥ 35 kg/m², previous use of beta-blockers or calcium channel blockers, cardiac arrhythmias, renal dysfunction, airway hyperactivity, hypersensitivity to drugs used, pregnancy, and those who presented any characteristics or situations that researchers believed the patients would be at risk or under discomfort.
As pre-anesthetic medication, all patients received midazolam 15 mg orally approximately one hour prior to surgery. When the patient met the inclusion criteria, a sealed envelope numbered according to the order of inclusion was taken to the operating room. For these patients, the same material was requested from the pharmacy: a 100 mL saline bag, a magnesium sulfate ampoule, two esmolol vials, a propofol ampoule, fentanyl and atracurium.
All the drugs involved in the study were prepared in a separate room by different anesthesiologist responsible to check the envelopes, hiding the vials of the study medication until the data collection was completed. Two other anesthesiologists were responsible to perform the induction of the anesthesia, OTI, data collection and were blinded according to the envelopes and drugs used.
Patient monitoring included cardioscope, non-invasive blood pressure, and pulse oximetry. The venoclysis was performed following the criteria of the anesthesiologist.
After venoclysis, infusion of a 100ml bag of saline solution, which may or may not contain 30 mg/kg of magnesium sulfate infused ten minutes prior to anesthetic induction, was started. About three minutes prior to intubation, the following were infused: 20 mL syringe which may or may not contain 1.5 mg/kg esmolol and standard anesthetic induction with 3 μg/kg fentanyl, 2 mg/kg propofol and 0.5 mg/kg of atracurium. Direct laryngoscopy and OTI were performed after three minutes of the neuromuscular blocker infusion.
A Macintosh® laryngoscope was used for OTI, with a blade selected according to the airway dimensions of each patient, at the discretion of the anesthesiologist. The size of the orotracheal tube was chosen in the same way. After OTI, capnography monitoring was initiated. All patients were ventilated in the first five minutes at a tidal volume of 6 mL/kg, 12 breaths per minute, 1 L/min oxygen flow, 1 L/min compressed air and 2.0% sevoflurane.
There were no external stimulations to the patients, such as a surgical incision or change of decubitus that could generate a confounding factor in the measurement of the hemodynamic response in the first five minutes.
The patient’s demographic data and Heart Rate (HR), Systolic Blood Pressure (SBP), Diastolic Blood Pressure (DBP) and Mean Arterial Pressure (MAP) were recorded in the research protocol, as follow: (T1) considering the baseline values of the patients; (T2) immediately prior to intubation. Following the data collection, BP and HR were still recorded one (T3), three (T4) and five (T5) minutes after intubation.
Protocols
Hypertension was considered when BP values were greater than 20% of the baseline values or SBP>140 mmHg. Hypotension was considered when BP values were lower than 20% of baseline or SBP<90 mmHg.
Tachycardia was considered when HR was greater than 20% of baseline or HR>100 bpm. Bradycardia was considered when HR values were lower than 50 bpm [11].
Statistics
The Epidata 3.1 program (EpiData Association, Odense, Denmark) was used to enter the data and the statistical analysis was conducted by SPSS software v.21.0 (IBM, Armonk, New York, USA). The descriptive analysis was performed with the presentation of mean, standard deviation and median for quantitative variables and absolute numbers and proportions for qualitative variables. The association tests and differences between the groups studied were verified by the post-hoc ANOVA test for numerical variables, and by chi-square or Fisher’s exact test, when appropriate, for the categorical variables. The paired t test was used to compare the HR, SBP, DBP and MAP parameters at T2, T3, T4 and T5 times in comparison to T1 baseline. The significance level considered was 95%.
Results
Patients included according to the criteria and the exclusion needed are shown in the Figure 1. Baseline characteristics are described in Table 1.
There was no statistical difference of HR between the groups between groups (Figure 2).
Systolic blood pressure of group M remained on the average of 33.012 mmHg higher than that of group E (p=0.002) and on the average of 29.610 mmHg higher than that of group C (p=0.003) in T3 (Figure 3). It was also higher in T4 and T5 compared to group E (p=0.014 and p=0.019).
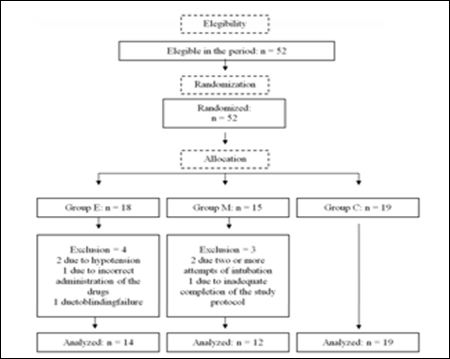
Figure 1: Fluxogram of randomization, eligibility and loss of follow-up.
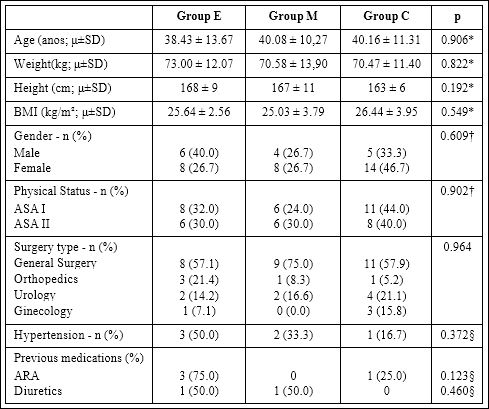
Table 1: Base line characteristics.
*ANOVA post hocTukey’s test; † Pearson’s chi square; §Fisher’s exact test.
E: Esmolol; M: Magnesium sulfate; C: Control; p: p value; μ: mean; SD: Standard Deviation; BMI: Body Mass Index; Kg: Kilograms; m2: metersquare; ASA: American Society of Anestesiology; ARA: angiotensin receptor antagonists
Diastolic blood pressure of group M was higher in relation to the group PAD at time T4 (p=0.019) (Figure 4). At other times there was no statistical difference in DBP between the groups.
The MAP of group M was higher compared to group MAP at T3 and T4 times (p=0.020 and p=0.021, respectively) (Figure 5).
Considering the intragroup variation, the changes in the parameters evaluated for the initial baseline value, in the E group, there was no statistical difference in the HR variation between the times. In the M group, there was a fall in the mean HR in T2 as compared to T1 (p=0.001). In group C, there was a decrease in HR compared to baseline at T2 (p<0.001), T3 (p=0.005) and T5 (p<0.001) times.
In groups E and C, SBP and DBP remained lower at all times when related to baseline (p<0.001). In group M this happened in T2 for SBP and DBP (p<0.001) and in T5 only for DBP (p=0.012).
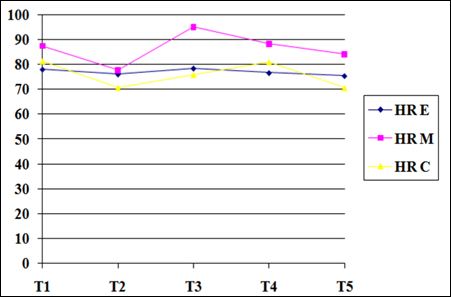
Figure 2: Mean Heart Rate (HR). There was no statistical difference between groups.
E: Esmolol; M: Magnesium sulfate; C: Control; T1: arrival in the operating room (basal); T2: just before Orotracheal Intubation (OTI); T3: 1 minute after OTI; T4: 3 minutes after OTI; T5: 5 minutes after OTI
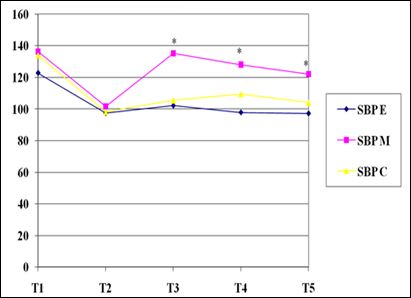
Figure 3: Mean Systolic Blood Pressure (SBP). There was a statistical difference between groups at times T3, T4 and T5 (*p<0.05).
E: Esmolol; M: Magnesium sulfate; C: Control; T1: arrival in the operating room (basal); T2: just before Orotracheal Intubation (OTI); T3: 1 minute after OTI; T4: 3 minutes after OTI; T5: 5 minutes after OTI.
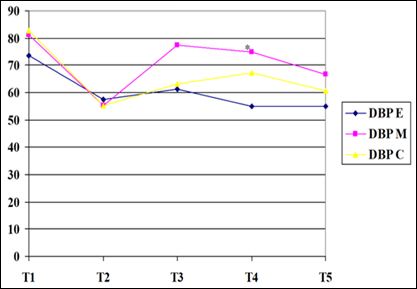
Figure 4: Mean Diastolic Blood Pressures (DBP). There was a difference between groups M and E at T4 (*p=0.019).
E: Esmolol; M: Magnesium sulfate; C: Control; T1: arrival in the operating room (basal); T2: just before Orotracheal Intubation (OTI); T3: 1 minute after OTI; T4: 3 minutes after OTI; T5: 5 minutes after OTI.
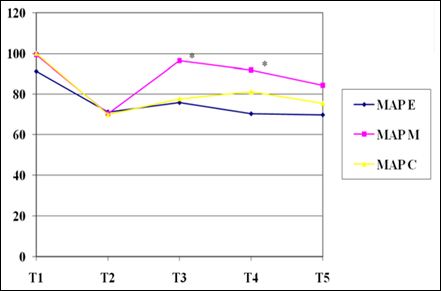
Figure 5: Mean Arterial Pressure (MAP). There was a difference between group M and E in T3 and T4 (*p<0.05).
E: Esmolol; M: Magnesium sulfate; C: Control; T1: arrival in the operating room (basal); T2: just before orotracheal intubation (OTI); T3: 1 minute after OTI; T4: 3 minutes after OTI; T5: 5 minutes after OTI.
MAP in groups E and C remained lower at all times when related to baseline, and in group M at times T2 and T5 (p<0.001 and p=0.023, respectively).
Comparing T3 with T1, episodes of tachycardia were recorded in two patients in group E (14.2%) and three patients in group M (25%). Only one patient in group C had bradycardia (5.2%).
Two patients in group M had hypertension (16.6%). Hypotension occurred in six patients in group E (42.8%), one patient in group M (8.3%) and ten patients in group C (52.6%).
Discussion
There was no statistical significance in the increase of HR, SBP, DBP and MAP in relation to baseline values after OTI in none of the groups in the present study. When compared to group E, group M presented higher SBP levels from one to five minutes after IOT and MAP from one to three minutes. Compared to group C, it had higher SBP one minute after OTI.
Mendonça et al. [11] used magnesium sulfate at a dose of 30 mg/kg and had an increase in SBP and DBP with statistical significance after intubation when compared to baseline values, different from what was observed in the present study. Hypertension and tachycardia were recorded11, but no hypotension was reported.
A similar study was conducted by Borah et al. [14], which were also observed a significant increase in SBP and DBP when compared to baseline values, in addition to an increase in HR and MAP in the first two minutes after OTI in patients who used magnesium sulfate. Kumar et al. [15] compared magnesium sulphate and esmolol, in which esmolol was superior controlling HR, a difference not observed in the present study. Both for Kumar [15] and our study, esmolol was superior to magnesium sulfate in the control of MAP increase after OTI.
The choice of the dose and method of the administration of magnesium sulfate was based on the study by Panda et al. [9] in hypertensive patients, which compared the efficacy of the drug in attenuating the hemodynamic response to laryngoscopy and OTI at doses of 30 mg/kg, 40 mg/kg and 50 mg/kg. Doses of 40 mg/kg and 50 mg/ kg were shown to increase the episodes of hypotension requiring intervention, whereas hemodynamic control was similar to a dose of 30 mg/kg, therefore, being an effective dose.
Bhalerao et al. [16] infused 50 mg/kg of magnesium sulfate for half an hour before induction in hypertensive patients, without a significant increase in SBP and HR after intubation, but they needed to intervene in the management of hypotension, which was already suggested by Panda et al. [9]. Khan et al. [17] achieved good results with the use of 60 mg/kg of magnesium sulfate. For Honarmand et al. [18], who compared different doses of magnesium sulfate in normotensive patients, 30mg/kg would be comparable to higher doses in preventing the increase of SBP, DBP and MAP up to five minutes after intubation.
The maximum increase in catecholamines, responsible for hemodynamic changes, occurs within five minutes after laryngoscopy and OTI, gradually decreasing after this time [18]. Acute myocardial infarction in the perioperative period is the main cause of postoperative morbidity and mortality due to hypertension and tachycardia [19].
Fentanyl used as adjuvant in standard anesthetic induction helps to attenuate the hemodynamic response to laryngoscopy and intubation [20]. Gogus et al. [20] compared the use of esmolol and fentanyl alone to reduce this response and found that esmolol at a dose of 2 mg/kg was more effective in decreasing SBP, DBP and MAP than 2 μg/kg fentanyl, butthere was no difference between both groups in relation to the prevention of HR increase. In the study by Bhalke et al. [21] the combination of fentanyl and esmolol was superior to esmolol alone in the control of HR, SBP, DBP and MAP after OTI.
The association of esmolol at 1.5 mg/kg to the combination of anesthetic induction medications showed no statistical difference between groups E and C at any of the times of the present study. There was a change in HR with a decrease in relation to baseline in group C, which did not occur in group E, which maintained a stable HR at all times. The doses of esmolol and fentanyl were sufficient to prevent the increase of mean HR, SBP, DBP and MBP after intubation, but at the expense of a higher frequency of hypotension.
Esmolol has the potential to reduce the requirement of opioids, such as fentanyl, in addition to reducing the incidence of nausea and vomiting in the postoperative period [22]. Bolus administration was chosen due to the practicality and rapid onset of the drug [23], directed to the transient cardiovascular response under study. Several doses and administration forms of esmolol have been used. Singhal et al. [24] concluded that a bolus of 1.5 mg/kg esmolol three minutes before intubation is safe and effective to attenuate hemodynamic changes.
Limitations of the Study
Among the limitations of the study, we highlight that outcomes such as arrhythmias and myocardial ischemia were not evaluated, as suggested by Khan et al [25]. The induction technique used resulted in a certain degree of hypotension in the patients, well tolerated in ASA I and II subjects. There was no vasopressor consumption for T2-weighted hypotension because intubation would be performed after vasopressor tone1-3. Two patients from the esmolol group were excluded due to hypotension (MAP<60 mmHg) verified at T3 and T4 times after intubation, requiring intervention. There was exclusion of these patients, who used different vasopressors. The laryngoscopy technique of the different physician involved may have influenced the results. The conduction of new studies with larger sample size could clarify disagreements hitherto presented in the literature.
Conclusions
Based on the data from the present study, it can be concluded that esmolol at a dose of 1.5 mg/kg bolus 3 minutes before intubation is superior to magnesium sulfate at the dose of 30 mg/kg infused within 10 minutes before anesthetic induction in the control of hypertensive response induced by manipulation of the airways. The association of propofol and fentanyl in standard anesthetic induction may justify the performance of the control group in the attenuation of the reflex studied.
References
- King BD, Harris LC, Greifenstein FE, Elder JD, Dripps RD (1951) Reflex circulatory responses to direct laryngoscopy and tracheal intubation performed during general anesthesia. Anesthesiology 12: 556-566.
- Hassan HG, el-Sharkawy TY, Renck H, Mansour G, Fouda A (1991) Hemodynamic and catecholamine responses to laryngoscopy with without endotracheal intubation. Acta Anaesthesiol Scand 35: 442-447.
- Kayhan Z, Aldemir D, Mutlu H, Oğüş E (2005) Which is responsible for the haemodynamic response due to laryngoscopy and endotracheal intubation? Catecholamines, vasopressin or angiotensin? Eur J Anaesthesiol 22: 780-785.
- Marulasiddappa V, Nethra HN (2017) A Comparative Study of Clonidine and Lignocaine for Attenuating Pressor Responses to Laryngoscopy and Endotracheal Intubation in Neurosurgical Cases. Anesth Essays Res 11: 401-405.
- Khan F, Ullah H (2013) Pharmacological agents for preventing morbidity associated with the haemodynamic response to tracheal Pharmacological agents for preventing morbidity associated with the haemodynamic response to tracheal intubation 3: CD004087.
- Arora S, Kulkarni A, Bhargava AK (2015) Attenuation of hemodynamic response to laryngoscopy and orotracheal intubation using intravenous J Anaesthesiol Clin Pharmacol. 31: 110-114.
- Çakirgöz MY, Tasdögen A, Olguner Ç, Korkmaz H, Öğün E, et al. (2014) Efeito de diferentes doses de esmolol sobre a resposta hemodinâmica, BIS e resposta de movimento durante a intubação orotraqueal: estudo prospectivo, randômico e duplo‐cego. Rev Bras Anestesiol 64: 425-432.
- Harless M, Depp C, Collins S, Hewer I (2015) Role of Esmolol in Perioperative Analgesia and Anesthesia: A Literature AANA J 83: 167-177.
- Panda NB, Bharti N, Prasad S (2013) Minimal effective dose of magnesium sulfate for attenuation of intubation response in hypertensive J Clin Anesth 25: 92-97.
- Marashi SM, Soltani-Mohammadi S, Azimaraghi O, Moradi N, Movafegh A (2015) The Effect of Premedication by Remifentanil and Magnesium Sulfate in Hemodynamic Responses to Tracheal Intubation in Cesarean Section Delivery: 1 A Randomized Double-Blinded Controlled Acad J Surg 2: 57-61.
- Mendonça FT, Queiroz LMGM, Guimarães CCR, Xavier ACD (2017) Os efeitos da lidocaína e do sulfato de magnésio na atenuação da resposta hemodinâmica à intubação orotraqueal: estudo unicêntrico, prospectivo, duplamente encoberto e aleatorizado. Rev Bras Anestesiol 67: 50-56.
- Herroeder S, Schönherr MR, Hert S, Hollmann MW (2011) Magnesium--essentials for Anesthesiologists. Anesthesiology 114: 971-
- Dean AG, Sullivan KM, Soe MM (2013) OpenEpi: Open Source Epidemiologic Statistics for Public Health, Versão.
- Borah B, Shukla MI, Joshi NK, Parasmani (2017) A comparative study between dexmedetomidine, clonidine and magnesium sulfate in attenuating hemodynamic response to laryngoscopy and intubation a randomised Indian J Clin Anesth 4: 30-36.
- Kumar D, Singh P, Wani Z (2017) To compare the role of i.v clonidine, MgSO4 and esmolol in attenuating hemodynamic responses following laryngoscopy and intubation and on blood loss in patients undergoing endoscopic sinus Indian J Res 6: 19-22.
- Bhalerao NS, Modak A, Belekar V (2017) Comparison between magnesium sulfate (50 mg/kg) and lignocaine (2 mg/kg) for attenuation of intubation response in hypertensive patients. J Datta Meghe Inst Med Sci Univ 12:118-120.
- Khan BA, Mahtalath, Sirajuddin MD (2017) Attenuation of cardiovascular responses to laryngoscopy and intubation dexmedetomidine magnesium sulfate. J Evid Based Med Healthc 4: 495-498.
- Honarmand A, Safavi M, Badiei S, Daftari-Fard N (2015) Different doses of intravenous magnesium sulfate on cardiovascular changes following the laryngoscopy and tracheal intubation: A double-blind randomized controlled trial. J Res Pharm Pract 4: 79-84.
- Sarkar J, Anand T, Kamra SK (2015) Hemodynamic response to endotracheal intubation using C-Trach assembly and direct larynSaudi J Anaesth 9: 343-347.
- Singh S, Laing EF, Owiredu WKBA, Singh A (2013) Comparison of esmolol and lidocaine for attenuation of cardiovascular stress response to laryngoscopy and endotracheal intubation in a Ghanaian Anesth Essays Res 7: 83-88.
- Gogus N, Akan B, Serger N, Baydar M (2014) Comparação entre os efeitos de dexmedetomidina, fentanil e esmolol na prevenção da resposta hemodinâmica à intubação. Rev Bras Anestesiol 64: 314-319.
- Bhalke R, Karale MS, Deshmukh U (2017) Comparison of esmolol versus combination of esmolol and fentanyl in preventing cardiovascular stress response to Int J Clin Trials 4: 49-57.
- Watts R, Thiruvenkatarajan V, Calvert M, Newcombe G, Wijk RM (2017) The effect of perioperative esmolol on early postoperative pain: A systematic review and meta-analysis. J Anaesth Clin Pharmacol 33: 28-39.
- Hatti R, Patil V (2016) Suppression of pressor response during laryngoscopy and endotracheal intubation by esmolol administered in doses of 1.5 mg/kg, 2.25 mg/kg: A comparative clinical study. J Evolution Med Dent Sci 24: 1281-1284.
- Singhal SK, Malhotra N, Kaur K, Dhaiya D (2010) Efficacy of esmolol administration at different time intervals in attenuating hemodynamic response to tracheal intubation. Indian J Med Sci. 64: 468-475.
Citation: : Machado LS, Silva AS, Fonseca EV, Rezende RV, Oliveira BH, et al. (2020) Comparative Study of the Efficacy of Esmolol and Magnesium Sulfate in Attenuating Hemodynamic Response to Laryngoscopy and Endotracheal Intubation. J Anes Perio Manag 4: 006
Copyright: © 2020 Machado LS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.