*Corresponding Author:
Thuc Dinh Van,
Department of Pediatrics, Haiphong Medical and Pharmaceutical University, Haiphong, Vietnam
Tel: +84 2253731907
E-mail: dvthuc@hpmu.edu.vn
Summary
Anemia in preterm neonates in Haiphong was studied by a retrospective, descriptive analysis including 113 eligible patients recruited between January 2015 and December 2016. Data on the clinical, laboratorial characteristics and treatment result of anemia was assessed. The sexual ratio (male/female) was 1.3/1. Most of patients were born in rural areas (60.2%) with mild anemia (56.6%). The most common causes of hospitalization were cyanosis (38.1%) and rapid breathing or apnea (56.6%). The clinical symptoms frequently presented in the preterm infants with anemia were pallor (75.2%), rapid breathing or apnea (57.5%) and low weight (50.4%). These patients had high risk of comorbidities such as respiratory diseases and other infections. RBC count result was mostly at the level of 2-3 x 1012/L, with the average value was 2.58±0.595 x 1012/L. The average value of Hb concentration was 99.81±10.406 g/L. Blood transfusions were applied in most of patients (97.3%) with the average number of transfusions was 1.66±0.167 times and the average of volume of transfusions was 21.55±8.71 ml/kg. The treatment outcome was: 67.3% of patients acquired stable status; 18.5% were unresponsive and transferred to the Vietnam National Children’s Hospital for further treatment; 14.2% of the preterm infants were died.
Keywords
Anemia; Blood transfusion; Preterm infant
Abbreviations
NICU: Neonatal Intensive Care Unit; WHO: World Health Organization; RBC: Red Blood Cell; Hb: Hemoglobin; Hct: Hematocrit
Introduction
Following WHO’s report, globally, anemia affects 1.62 billion people (95% CI: 1.50-1.74 billion), which corresponds to 24.8% of the population (95% CI: 22.9-26.7%), with the highest prevalence is in preschool-age children (47.4%, 95% CI: 45.7-49.1) [1]. Among this group, neonatal anemia, including anemia in preterm neonates, defined as a Hemoglobin (Hb) or Hematocrit (Hct) concentration of >2 standard deviations below the mean for postnatal age, is a major problem encountered in neonatal intensive care units. Moreover, long- term anemia has been reported to potentially affect both brain growth and other components of chronic disease on the premature infant [2]. Up to now, there isn’t any published research on anemia in preterm neonates in Haiphong- the third largest city in Vietnam. Therefore, we proceed with this topic with two goals:
- Describe the clinical and laboratory characteristics of anemia in preterm neonates at Haiphong Children’s Hospital in 2015-2016
- Comment on the results of treatment of anemia in the above subjects
Materials and Methods
A retrospective, descriptive analysis was conducted at the Neonatal Intensive Care Unit (NICU) in Haiphong Children’s Hospital. The NICU received the out-born infants transported from all the hospitals and medical centers in Haiphong and nearby areas. The diagnosis of anemia was based on clinical manifestations: pallor, cyanosis, signs of acute anemia (tachycardia, cardiac failure, respiratory distress, etc.). The infants were evaluated for a complete blood count and red cell indices to establish a diagnosis of anemia with the main criteria: Hb<110g/l. This criteria is applied for the diagnosis of anemia in children less than 5 years old in Haiphong Children’s Hospital, following the WHO recommendation [1,3].
A total of 113 eligible patients were recruited between January 2015 and December 2016. According to gestational age, the subjects were classified into three groups as follows: group 1: 21 week’s≤gestational age <28 weeks (n=5); group 2: 28 week’s≤gestational age <32 weeks (n=51); group 3: 32 week’s≤gestational age <38 weeks (n=57).
According to the Hb concentration, the subjects were classified into four groups as follow: group 1- mild anemia: 90 g/l≤Hb< 110 g/l; group 2 - moderate anemia: 70 g/l ≤Hb< 90 g/l; severe anemia: 30 g/ l≤Hb< 70 g/l; group 4 - decompensated anemia: Hb< 30 g/l.
Depending on each patients, the infants were received the treatment of anemia by whole blood and/or RBC transfusion. The treatment outcome was evaluated as: stable, unresponsive or death. All the unresponsive cases of anemia were transferred to the Vietnam National Children’s Hospital.
This study has been approved by the Research Ethics Committee of Haiphong Medical and Pharmaceutical University.
Statistical analysis: The Statistical Package for the Social Sciences (SPSS) program (16.0 for Windows software, LEAD Technology, Inc.) was used for analysis.
Results
General characteristics of the infants
The prevalence of anemia in preterm newborns is higher in male than that of females (56.6% vs. 43,4%, respectively). Most children are born in rural areas and have a gestational age of 28-37 week’s (Table 1). Most preterm neonates at gestational age group 3 had mild anemia, while most of patient at gestational age group 2 had moderate anemia (Table 2).

Table 1: General characteristics of the infants in all groups.

Table 2: Severity of anemia according to the gestational age group.
Clinical characteristics of anemia in preterm infants
The most common causes of hospitalization were cyanosis (38.1%) and rapid breathing or apnea (56.6%) (Table 3). The clinical symptoms frequently presented in the preterm infants with anemia were pallor (75.2%), rapid breathing or apnea (57.5%) and low weight (50.4%) (Table 4). These patients had high risk of comorbidities such as respiratory diseases and other infections (Table 5).
Laboratorial characteristics of anemia in preterm infants
Erythrocytes count result was mostly at the level of 2-3 x 1012/L (Table 6). The average value of the whole research population was 2.58±0.595 x 1012/L. The average value of Hb concentration was 99.81±10.406 g/L (Table 7).
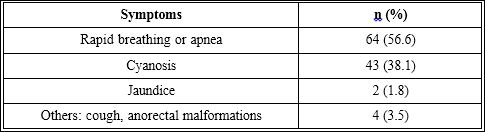
Table 3: Table of causes for hospitalization.
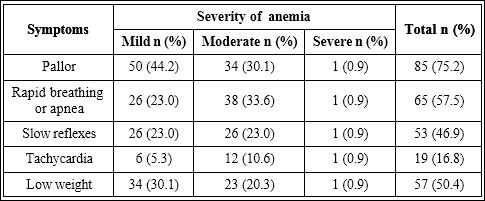
Table 4: Distribution of clinical symptoms according to the severity of anemia.
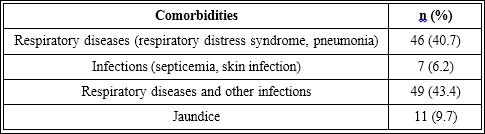
Table 5: Distribution of patients according to the comorbidities.
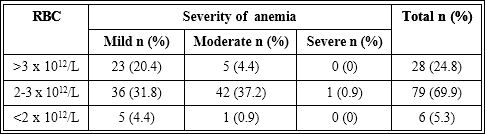
Table 6: Distribution of the level of anemia according to the result of RBC count.
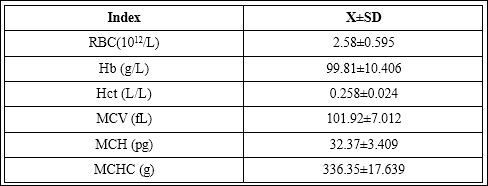
Table 7: The average value of the RBC count and red cell indices.
Treatment of anemia
Blood transfusions were applied in most of patients (97.3%) with the average number of transfusions was 1.66±0.167 times and the average of volume of transfusions was 21.55±8.71 ml/kg. Patients were treated by whole blood and/or packed-cell transfusions (Table 8 and Table 9). The treatment outcome was: 67.3% of patients acquired stable status; 18.5% were unresponsive and transferred to the Viet- nam National Children’s Hospital for further treatment; 14.2% of the preterm infants were died (Figure 1).

Table 8: Treatment of anemia by transfusion.
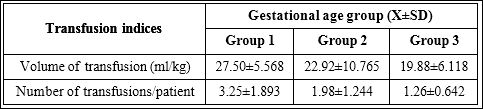
Table 9: Volume and number of transfusions according to the age of infants.
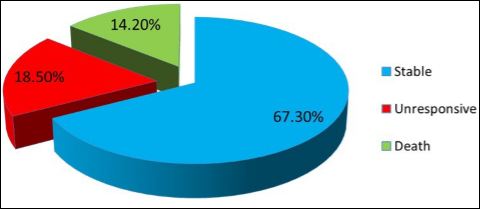
Figure 1: Treatment outcome of anemia in preterm infants.
Discussions
General characteristics of the infants
In our research, almost of patients were from the rural areas (60.2%). In both of the 2 groups of patients from rural and urban areas, mild anemia is the most frequent. A study by Khoi HH et al., also reported consistent results with our study, showing that the anemia in neonates was more recurrent in the rural than in the urban regions [4]. Anemia was more frequently observed in male patients than in female, which is possibly related to the increasingly imbalanced sex ratios at birth occurring in this region of Viet Nam [5,6]. According to the gestational age of the preterm infants, anemia was most seen in the group 3: 32 weeks≤ gestational age <38 weeks (50.4%). At the 32nd week of gestation, plasma volume increases by about 50% while the red cell volume also increases, but the increase is moderate (about 20%) and delayed [7]. Consequently, the total blood volume increases with hemodilution, leading to the higher risk of anemia in the preterm neonates of group 3.
Even that Haiphong is in Southeast Asia one of the thalassemia endemic regions, unfortunately, we couldn’t access the rate of thalassemia among the groups of patients due to the lack of a routine hemoglobin electrophoresis for anemia cases in Haiphong Children’s Hospital [8].
Clinical characteristics of the patients
The leading causes for hospitalization in this study were respiratory stress and cyanosis. Pallor is the most common clinical manifestation in our research (75.2%), followed by respiratory stress (rapid breathing or apnea: 57.5%) and delayed reflexes (46.9%). A study of Wardrop CA. et al., showed that 50% of the preterm neonates have abnormal clinical signs related to anemia such as pallor, tachycardia, rapid breathing and delayed reflexes [9]. This abnormality is due to the function of Hb the main oxygen-carrying protein in blood. Lacking of Hb could lead to the insufficient support of oxygen delivery to tissue, pallor, respiratory stress and tachycardia [10].
In our study, 50.4% of preterm neonates with anemia also have low body weight. This data is supportive for the fact that anemia is significantly associated with being born small [11]. In Anemia Of Prematurity (AOP), mean Hb concentration reportedly falls to approximately 8 g/dL in infants with a birth weight of 1000-1500 g and to 7 g/ dL for infants weighing less than 1000 g [12].
We noticed that infants with anemia have high risk of comorbidities such as respiratory diseases (respiratory distress syndrome, pneumonia) or respiratory diseases combined with other infections (sepsis, skin infection) (40.7% and 43.4%, respectively). Due to the prematurity of respiratory and immunity system in preterm infants, it is comprehensive that the associated diseases mentioned above appeared frequently in this study [13]. It has been reported that the correction of infant anemia is associated with a reduction in the increased morbidity (fever, respiratory tract infections and diarrhea) [14,15].
Laboratorial characteristics on the patients
The complete blood count returned that the average amount of RBC was 2.58±0.6 x 1012/L, and almost of the infants with anemia at mild or moderate level. 69.95% infants with moderate anemia have moderate reduction level of RBC (2-3 x1012/L). The average values of important RBC indices were as following: Hb: 99.81±10.41 g/l; MCV: 101.92±7.01 fL; MCH: 32.57±3.41 pg; MCHC: 336.35±17.64g. Our data is consistent with the data reported by a research of Hasanbegovic et al., in Bosnia and Herzegovina: the group of infants≤ 32 gestational weeks has average amount of RBC: 2.6±0.62 x1012/L and Hb: 96±12g/l [16].
Treatment outcome
All the infants included in this study received the treatment of anemia according to the Pediatric treatment guideline of Haiphong Children’s Hospital. As a result, 97.3% of the patients were given transfusion of whole blood and/or RBC. Whole blood transfusion was more frequently applied than packed red blood cell transfusion (73.5% vs. 44.2%, respectively), because many preterm neonates were lack of not only RBC but also of coagulation factors (reduction of fibrin, plasminogen or prothrombin up to 15-20%, data not shown). Some infants needed more than one transfusion and finally received both whole blood and RBC supply. As this study was carried out in the principal pediatric hospital of the city which has stable blood products supply, almost of the anemia cases were treated by a reasonable transfusion following the general guideline of the hospital. According to the gestational age of the infants, blood transfusion was applied to all the patient of group 1 (21-28 GW), 98% of group 2 (28-32 GW) and 96.5% of group 3 (32-37 GW).
The global view of treatment outcome in our research is reported as following: 67.3% of patients were stable; 18.65% was unresponsive to the treatment and needed to be transferred to the Vietnam National Children’s Hospital; the percentage of death cases was 14.2%. Almost of patients in the gestational age group 2 and 3 became stable after the treatment (64.3% and 81.6%, respectively). Among the group 1 (under 28 GW), 60% of infants were unresponsive and transferred while 40% were death. Trung LN. et al., also reported consistent data: 48.3% of anemia cases in infants at 26-28 GW were death and this number in the group 29-31 GW was 8.1% [17]. It is also noticed that the percentage of mild anemia is higher in the infants with older gestational age, and the responsiveness to the treatment is better in the group with older age than in the younger age group.
Conclusion
Our study provides details on clinical, laboratorial characteristics and treatment outcome of anemia in preterm neonates of a big city in Vietnam. Anemia in preterm infant still appears as a major challenge for public health. Anemia is often associated with other comorbidities, leading to a worse prognostic and high death rate in the preterm neonate. The mortality rate remained fairly high despite the availability of active treatment and carein a big city of the country. This reality highlights the importance of preventing anemia during pregnancy, especially in the rural area of a developing country like Vietnam.
References
- de Benoist B, McLean E, Egli E, Cogswell M (2008) Worldwide prevalence of anaemia 1993-2005: WHO Global Database on Anaemia. World Health Organization, Geneva, Switzerland.
- Colombatti R, Sainati L, Trevisanuto D (2016) Anemia and transfusion in the Semin Fetal Neonatal Med 21: 2-9.
- NC K (2012) Textbook of pediatrics. Hanoi, Medical Publishing House, Hanoi,
- Khoi HH GT (1994) Proper nutrition and health. Hanoi, Medical Publishing Hanoi, Vietnam.
- Guilmoto CZ, Hoang X, Van TN (2009) Recent increase in sex ratio at birth in Viet Nam. PloS one 4: 4624.
- Duong DTT (2015) Sex Ratio at Birth and the Ideal Family in Chi Linh District, Tap chi y te cong cong 3: 29-38.
- Costantine MM (2014) Physiologic and pharmacokinetic changes in pregnancy. Front Pharmacol 5: 65.
- Svasti S, Hieu TM, Munkongdee T, Winichagoon P, Van Be T, et al. (2002) Molecular analysis of beta-thalassemia in South Vietnam. American journal of hematology 71: 85-88.
- Wardrop CA, Holland BM, Veale KE, Jones JG, Gray OP (1978) Nonphysiological anaemia of prematurity. Arch Dis Child 53: 855-860.
- Tsai AG, Hofmann A, Cabrales P, Intaglietta M (2010) Perfusion vs. oxygen delivery in transfusion with “fresh” and “old” red blood cells: the experimental Transfusion and apheresis science : official journal of the World Apheresis Association : official journal of the European Society for Haema- pheresis 43: 69-78.
- Ferri C, Procianoy RS, Silveira RC (2014) Prevalence and risk factors for iron-deficiency anemia in very-low-birth-weight preterm infants at 1 year of corrected age. J Trop Pediatr 60: 53-60.
- Jeon GW, Sin JB (2013) Risk factors of transfusion in anemia of very low birth weight infants. Yonsei Med J 54: 366-373.
- Melville JM, Moss TJ (2013) The immune consequences of preterm birth. Front Neurosci 7: 79.
- Angeles IT, Schultink WJ, Matulessi P, Gross R, Sastroamidjojo S (1993) Decreased rate of stunting among anemic Indonesian preschool children through iron supplementation. Am J Clin Nutr 58: 339-342.
- Soliman AT, De Sanctis V, Kalra S (2014) Anemia and growth. Indian J Endocrinol Metab 18: 1-5.
- Hasanbegovic E, Cengic N, Hasanbegovic S, Heljic J, Lutolli I,et al. (2016) Evaluation and Treatment of Anemia in Premature Infants. Med Arch 70: 408-412.
- https://www.nestlenutrition-institute.org
Citation: Duong TAD, Van TD (2018) Clinical, Laboratorial Char- acteristics and Treatment Result of Anemia in Preterm Neonates in Haiphong Children’s Hospital In 2015-2016. J Hematol Hemother 3: 005.
Copyright: © 2018 Van TD. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and re- production in any medium, provided the original author and source are credited.