*Corresponding Author:
Zakaria Qechchar,
Department of Cardiology, University Hospital Center Ibn Rochd-Casablanca, Casablanca, Morocco
Tel: +212 645744262
Email: Dr.qechchar@outlook.fr
Abstract
Congenitally corrected transposition of the great arteries CCTGA is an uncommon congenital heart defect, often coupled to numerous cardiac morphological abnormalities and conduction defects.
We report the case of a 45 years old male who spent most of his life asymptomatic until feeling weak and dizzy what led to the finding of a complete AV Block on a CCTGA with a large VSD, a pulmonary stenosis and a tricuspid valve insufficiency. The complete AV Block has been treated by pacing, with good results. The follow up showed a significant improvement in clinical sign and quality of life.
Keywords
AV block; CCTGA; Chronic asthenia
Introduction
Congenitally corrected transposition of the great arteries CCTGA is an uncommon congenital heart defect, often coupled to numerous cardiac morphological abnormalities and conduction de- fects.
CCTGA is encountered in 0.5% to 1.4% of patients with congenital heart disease; nevertheless, the real prevalence of the malformation is yet to be determined [1]. It is also known as a double discordance: The core of the lesion is the association of discordant atrioventricular and ventriculo-arterial [2].
Ventricular Septal Defect (VSD), pulmonary stenosis, and abnor- malities of the systemic atrioventricular (tricuspid) valve are the main abnormalities met in CCTGA [3].
Heart rhythm and conduction disorders such as bradyarrhythmias (1st, 2nd and 3rd degree AV blocks; sinus node dysfunction) and su- praventricular tachycardias (WPW syndrome, focal atrial tachycar- dia, atypical AV nodal re-entry, atrial fibrillation, and atrial flutter) have been reported [1]. Patients with those defects often present early symptoms of such disorders leading to the CCTGA diagnosis.
We report the case of a 45 years old male who spent most of his life asymptomatic until feeling weak and dizzy what led to the finding of a complete AV Block on a CCTGA with a large VSD, a pulmonary stenosis and a tricuspid valve insufficiency. The complete AV Block has been treated by pacing.
Case Report
The patient was a 45-year-old man who presented to the emergen- cy department with asthenia and dizziness for 2 weeks and worsening for two days. He had no significant medical history and no cardiovas- cular risk factors. He was conscious, afebrile and reported no chest pain. His blood pressure was 128/77 mmHg, heart rate was 32 Beats per minutes (bpm). Respiratory rate was 17/min and oxygen satura- tion was 98% on ambient air. The remainder of the examination was unremarkable except a low Body Mass Index (B.M.I) 17 with 169 cm and 50 kilos.
Admission EKG showed complete AV block with a ventricular rate of 28 bpm (Figure 1). The full blood count and biochemical param- eters were within normal ranges. High sensitive troponin levels were normal.
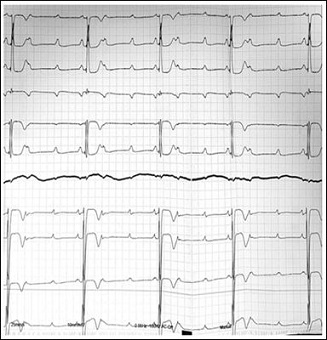
Figure 1: Admission EKG showed complete AV block with a ventricular rate of 28 bpm
A bedside transthoracic echocardiography showed: A Situs Solitus, a CCTGA (right ventricle (RV) is the systolic ventricle) and preserved right ventricular systolic function (ejection fraction (EF) 50-55%),large VSD (a 22 mm interventricular communication), a pulmonary stenosis, a mild tricuspid valve insufficiency in systemic position (Fig- ures 2A and 2B).
Duplex venous imaging showed extensive acute DVT of the left common femoral, femoral, popliteal, gastrocnemius, posterior tibi- al, peroneal, and great saphenous veins. The left External Iliac Vein (EIV) close to the junction with the Common Femoral Vein (CFV) showed evidence of thrombosis. However, the left Common Iliac Vein (CIV) could not be evaluated with duplex venous imaging. Computed Tomography (CT) pulmonary embolism protocol showed right lower lobe segmental and subsegmental emboli. CT venogram of abdomen and pelvis showed a large heterogenous mass which measured 18.6 x 15.5 x 9.9cm (Figure 2). Mass effect was noted on the Inferior Venacava (IVC) and left CIV with evidence of thrombus in the left EIV, Internal iliac vein, and CIV. Ankle-brachial indices were not obtained. She was started on intravenous heparin.
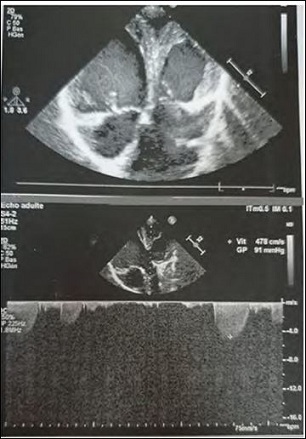
Figure 2A: Transthoracic echocardiograph (CCTGA): Pulmonary stenosis, a mild tri- cuspid valve insufficiency in systemic position.
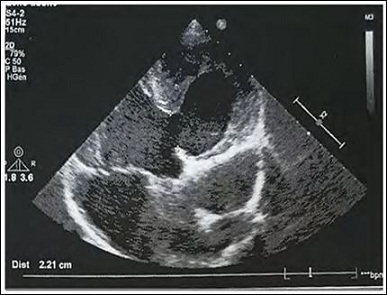
Figure 2B: Transthoracic echocardiography (CCTGA) and preserved right ventricular systolic function, large VSD (22 mm).
The patient was taken to the electrophysiology lab with implanta- tion of a temporary pacemaker. He was ventricular paced at 90 bpm and stayed hemodynamically stable overnight.
The next day he received a dual-chamber pacemaker (XL DR 5826, St. Jude Medical, USA). The atrial and ventricular leads were fixed correctly. The per-pacing imaging showing the leads positions and the pace maker position (Figures 3A, 3B and 3C). His paced ECG was shown in (Figure 4). His direct post-pacing interrogation demonstrat- ed atrial sensing and ventricular pacing rhythm without ventricular tachyarrhythmia. Atrial sensing was 4.4 mV, threshold was 0.5 V at 0.5 ms, and impedance was 538 ohms. Ventricular sensing was 6.8 mV, threshold was 0.5 V at 0.5 ms, and impedance was 326 ohms. The chest X-rays after pacemaker implantation made the day after shown no procedural complication. The patient was totally discharged and went home the day after with a fist follow up meeting in a month.
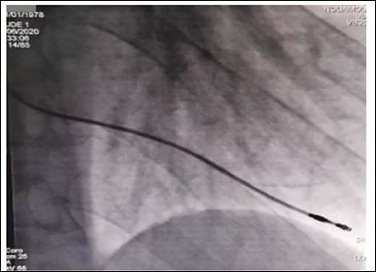
Figure 3A: The per-pacing imaging showing the ventricular lead position.
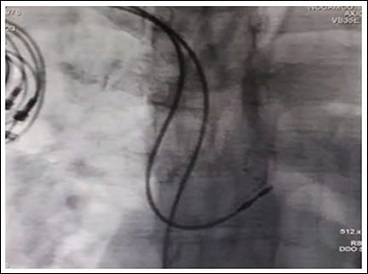
Figure 3B: The per-pacing imaging showing the atrial lead position.
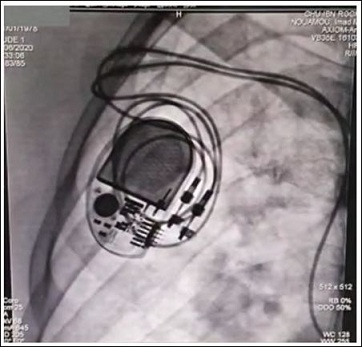
Figure 3C: The per-pacing imaging showing the pacemaker position after implantation.
Discussion
CCTGA is a singular congenital heart defect, often coupled to nu- merous cardiac morphological anomalies and conduction defects. The Baron Rokitansky, in his atlas of 1875, was the first to describe the entity we now know as congenitally corrected transposition [4].
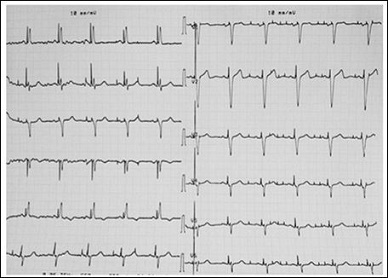
Figure 4: EKG after successful pacemaker inplantation.
CCTGA is met in 0.5% to 1.4% of patients with congenital heart disease; nevertheless, the real prevalence of the malformation is yet to be determined [1]. It is also known as a double discordance: the core of the lesion is the association of discordant atrioventricular and ventriculo-arterial [2].
Without accompanying defects, the patient will normally be as- ymptomatic early in life. Our patient, even with the associated defects such as large VSD (a 22 mm interventricular communication), a pul- monary stenosis, a mild tricuspid valve insufficiency in systemic position, has managed to live a normal life and have stayed asymptomatic for many decades.
Those defects are frequently described in literature. Friedberg and al. in 1970 studied theclinical profile of 60 patients with congenital corrected transposition of the great arteries. More than 50% presented VSD, 45% had pulmonary stenosis [5].
The symptoms he suffered from were more likely related to the complete AV block he had. It is known that CCTGA has increased risk of AV blocks, one third of the patients can present disturbances of AV conduction. Some studies have shown that the AV blocks can be present before birth and acquired at a rate of 2% per year [2,3,6]. In our case we don’t know if the AV block was present at birth or was acquired with time.
A review of contemporary management and outcomes in congen- itally corrected transposition of the great arteries led by Kutty and al. have shown that anatomic repairs have better short and medium-term outcomes, but the late incidence of reoperation, ventricular dysfunction, transplant and death are concerning. Patients needing LV retraining are particularly vulnerable to late LV failure. Even when relatively homogeneous subsets of CCTGA are considered, debates persist regarding best management options [7]. In our case the patient refused to undergo any kind of surgical repair of his heart anomalies.
Pacing was a reliable and viable option to correct his conduction defect but challenging due to the anatomical heart malformation.
Indeed, pacemaker implantation can be challenging in patients with CCTGA due to the intricate anomalies. The positioning of the ventricular lead with VSD was very challenging. Data about complete anatomy and coexisting abnormality can be obtained by contrast-en- hanced CT or magnetic resonance imaging before the procedure [2,3,8].
Follow up is preferably performed in a center with a program for adult congenital heart disease run by pediatric cardiologists, or by an adult congenital cardiologist who has had special training and experi- ence caring forpatients with congenital heart disease. The assessment of the systolic ventricular function and the degree of atrioventricu- lar valvar regurgitation is also primordial given that the majority of patients with CCTGA develop progressive congestive cardiac failure. The follow up and interrogation of the pace maker have to be very cautious and made by an experimented electrophysiologist.
There have been some reports of patients with congenitally cor- rected transposition living into late adulthood without heart failure in the absence of associated lesions, but this is not the norm [9].
Conclusion
CCTGA is a singular congenital heart defect, often coupled to numerous cardiac morphological anomalies and conduction defects. We report the case of a 45 years old male with a complete AV Block on a CCTGA with a large VSD, a pulmonary stenosis and a tricuspid valve insufficiency. The complete AV Block has been successfully treated by dual chamber pacing.
Competing Interests
The authors declare no competing interest.
Authors’ Contributions
All the authors contributed equally in drafting of the manuscript. All the authors read and agreed to the final manuscript.
References
- 1.Presbitero P, Somerville J, Rabajoli F, Stone S, Conte MR (1995) Corrected transposition of the great arteries without associated defects in adult patients: Clinical profile and follow Br Heart J 74: 57-59.
- 2.Wallis GA, Debich-Spicer D, Anderson RH (2011) Congenitally corrected transposition. Orphanet J Rare Dis 6.
- 3.Zhang L, Liu H, Wan Q, Han X (2019) Ventricular fibrillation in congenitally corrected transposition of great arteries treated with pacing: A case report. Eur Heart J Case Rep 3: 1-6.
- 4.Rokitansky C von (1875) Die Defecte der Scheidewände des Herzens: Patholog-anatomische Braumüller, Munich, Germany.
- 5.Friedberg DZ, Nadas AS (1970) Clinical profile of patients with congenital corrected transposition of the great arteries. A study of 60 cases. N Engl J Med 282: 1053-1059.
- 6.Paladini D, Volpe P, Marasini M, Russo MG, Vassallo V, et (2006) Diagno- sis, characterization and outcome of congenitally corrected transposition of the great arteries in the fetus: A multicenter series of 30 cases. Ultrasound Obstet Gynecol 27: 281-285.
- 7.Kutty S, Danford DA, Diller G-P, Tutarel O (2018) Contemporary management and outcomes in congenitally corrected transposition of the great arteries. Heart 104: 1148-1155.
- 8.Warnes CA (2006) Transposition of the Great Arteries. Circulation 114: 2699-2709
- 9.Cumming GR (1962) Congenital corrected transposition of the great vessels without associated intracardiac anomalies. A clinical, hemodynamic and an- giographic Am J Cardiol 10: 605-614.
Citation:Qechchar Z, Ammouri Z, Nouamou I, Drighil A, Habbal R (2020) Chronic Asthenia Revealing a Complete AV Block on a Congenitally Corrected Transposition of Great vessels: A Case Report and Brief Literature Review. J Case Repo Imag 4: 023.
Copyright: © 2020 Qechchar Z, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.


