*Corresponding Author:
E-Jian Lee,
Department of Surgery, National Cheng Kung University Hospital, Sheng-Li Road, Tainan, Taiwan,
Tel: +886-62353535-5203
Email: ejian@mail.ncku.edu.tw
Abstract
Most cavernous hemangiomas occur in the supratentorial compartment, the incidence of cavernous hemangiomas in the Internal Auditory Meatus (IAM) is very low in adults. Herein we present a 53-year-old male suffering from left side hearing loss and subsequent ipsilateral facial paresis was also noted. Magnetic Resonance Image (MRI) revealed a 7 millimeter tumor in the left internal auditory meatus. The tumor was totally removed via the suboccipital retrosigmoid approach and the pathological diagnosis was cavernous hemangioma. Although Computed Tomography (CT) scan and MRI can establish the presence of IAM lesions, there are no radiological diagnostic criteria to differentiate cavernous hemangiomas from other common lesions such as vestibular schwannomas. The tiny space-occupying lesion with profound cranial nerve dysfunction is the most distinguishable clinical feature from other neoplasms. Early surgical resection is recommended in the majority of published literature.
Keywords
Differential diagnosis; Facial paresis; Hearing loss; Hemangioma; Internal auditory meatus
Abbreviations
IAM = Internal Auditory Meatus; CT = Computed Tomography; MRI = Magnetic Resonance Image; CPA = Cerebello- pontine Angle; CNS = Central Nervous System; SRS = Stereotactic Radiosurgery
Introduction
Intracranial cavernous hemangiomas account for 10 to 20% vascular malformation in the Central Nervous System (CNS) [1]. But extra-axial lesions taking place in the Internal Auditory Meatus (IAM) are very rare, there are only 66 cases were reported in available English literatures [2]. The most common clinical manifestations are hearing impairment and facial paresis [2], just as the vestibular schwannomas. Neurosurgeons may have difficulty in distinguishing cavernous hemangiomas from other IAM tumors by images due to infrequency and relative small size during medical consultation. In this report, we present a patient with left side hearing loss and facial paresis due to a cavernous hemangioma in the IAM. Clinical history, radiological features, current treatment choice and neurological outcomes are discussed.
Case Report
This 53-year-old male was previously generally healthy. He came to our outpatient department due to an acute deterioration of facial paralysis in the past one month. House-Brackmann Grade IV left facial paralysis was determined. He also had progressive left hearing deficit for 3 years. The pure tone audiometry revealed left profound sensorineural hearing loss across all frequencies. Magnetic Resonance Image (MRI) showed a 7 millimeter mass in the left Internal Auditory Meatus (IAM). Tumor was isointense in T2-weight images and hypointense in T1-weight images with heterogenous contrast enhancement. It compressed the left facial nerve and vestibulocochlear nerve inside the meatus but did not exhibit Cerebellopontine Angle (CPA) extension (Figure 1). Under the impression of vestibular schwannoma with IAM involvement, due to no available Stereotactic Radiosurgery (SRS) equipment at our hospital, we arranged surgical excision of the tumor (retrosigmoid approach).

Figure 1: Axial T2-weight images revealed mild dilated left Internal Auditory Meatus (IAM). An isointensity mass (arrow) which compressed facial nerve (arrowhead) and vestibulocochlear nerve (asterisk) in the meatus.
Intraoperatively, the internal auditory meatus was exposed by high-speed drill. A well-circumscribed, reddish, raspberry-like tumor was found beneath the vestibulocochlear nerve (Figure 2). The tumor was piecemeal totally removed under the microscope. The facial nerve and vestibulocochlear nerve were preserved throughout the operation. Histological study demonstrated numerous large dilated thin-walled vessels lined by flattened endothelial cells without intervening neural parenchyma (Figure 3). Cavernous hemangioma was confirmed.

Figure 2: Internal auditory meatus was drilled by diamond burr for tumor mobilization. The Tumor (T) was beneath the vestibulocochlear nerve (VIII) and cause compression to it.
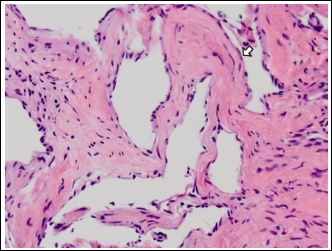
Figure 3: Histological study demonstrated numerous large dilated thin-walled vessels lined by flattened endothelial cells (arrow) without intervening neural parenchyma.
There were no complications post-operatively. The heat therapy, electrical stimulation was arranged and oral motor exercise was also taught to patient for facial rehabilitation by our physiatrist. After one year follow-up, facial paralysis had recovered slightly to House-Brack- mann Grade III. He refused try hearing aid because he got accus- tomed to monaural audition, however, there was no improvement in left hearing function (Figure 4).
Discussion
Cavernous hemangiomas, also known as cavernomas or cavernous malformations, are angiographically occult, low-flow vascular lesions composed of thin-walled, dilated capillary spaces without intervening neural parenchyma [3,4]. Intracranial cavernous hemangiomas account for 10 to 20% vascular malformation in the Central Nervous System (CNS) [1], but most occur in the supratentorial compartment (70~90%), with some found in the infratentorial region (15%) and spinal cord compartments (5%) [2,5]. Cavernous hemangiomas taking place in the IAM are very rare. Sundaresan et al., reported the first two cases in 1976 [6], and only 66 cases were reported in available English literature [2]. These tumors are thought to arise from the capillary plexus surrounding Scarpa’s ganglion and can either compress or infiltrate the cranial nerve [1,7-9]. Depending on this specific anatomic location, Mastronardi et al., documented the most common manifestation as hearing impairment (95.2%) which may be insidious, rapidly progressive, or suddenly developing. The second most common manifestation during diagnosis is facial paresis (37.1%).Other symptoms such as hemifacial spasm, gait disturbance or dysphagia are less common [2].
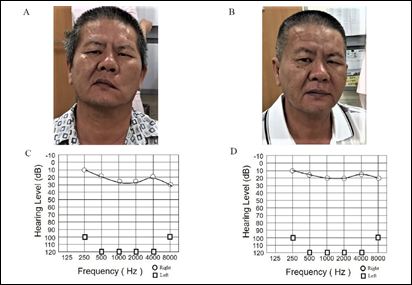
Figure 4: The facial paralysis had recovered slightly after operation. From House-Brackmann grade IV before operation (A) to grade III after a year follow-up (B). But the pre-operative (C) and post-operative (D) pure tone audiometry both re- vealed profound left hearing loss. There was no improvement in hearing function.
Compared to vestibular schwannoma or Cerebellopontine Angle (CPA) meningioma, cavernous hemangioma of IAM can cause significant cranial nerve deficit with a relative small tumor size. The tumor size of our case was even smaller than 10 millimeter. The vascular steal mechanism may explain these phenomena [8], the tumor takes away the blood supply of the nerve trunk which leads to severe nerve dysfunction despite the small tumor size. And intra-canal hemorrhage by the tumor can cause sudden onset severe facial paresis or hearing loss.
Contrast enhanced MRI is the most sensitive and specific diagnostic tool for cavernous hemangioma in the internal acoustic meatus [1]. Most reported cases demonstrate isointense to brain parenchyma in T1-weighted images and is 0 to hyper intense in T2-weighted images [2,3,5]. Heterogenous enhancement with contrast on T1-weighted images makes a possible differential diagnosis with the homogenous enhancement usually noted in vestibular schwannoma or CPA meningioma [1]. Hypointensity due to hemosiderin deposition in gradient-echo sequences also provides diagnostic information about cavernous hemangiomas [5]. CT scan may show dilated IAM or stippled patterns of calcification [10]. However, relatively small tumor size, usually less than 10 millimeters, during medical consultation for severe clinical presentation makes these radiological characteristics obscure. Therefore, preoperative differential diagnosis between a cavernous hemangioma in IAM and vestibular schwannoma is usually infeasible in the previously reported cases [2]. Besides cavernous hemangioma, other rare lesions of the IAM including non-vestibular schwannomas, lipomas, neurofibromas, meningiomas, lymphomas, arachnoid cysts and lipochoristomas, the reported incidence of these rare IAM lesions was 4.3~5.2%, only images are also insufficient to distinguish them from vestibular schwannoma preoperatively [11,12]. A combination of clinical features and radiological characteristics is very necessary to make an adequate tentative diagnosis.
Microsurgical resection is the preferred treatment for cavernous hemangioma in the IAM. Although some authors agree observation in patient with minor symptoms [13], however, most reported cases in the literatures showed either significant hearing or facial problem as initial diagnosis [2]. According to tumor size and residual functional hearing, middle fossa and retrosigmoid approach is appropriate for hearing preservation. Translabyrinthine approach offers early identification of the facial nerve in the IAM and is chosen for patients with no functional hearing [7,14]. In our case, although the patient had profound left hearing loss, we chose retrosigmoid approach because it was the most familiar method to the operator. Early surgical intervention gives a higher possibility of facial nerve functional improvement, but only one reported case had hearing acuity recovery after surgery [2,3,9,15]. No documented tumor local recurrence in the literature after microsurgical resection [1-3,8,16]. Despite the use of Stereotactic Radiosurgery (SRS) for cavernous hemangioma in the basal ganglion, thalamus or brainstem having sufficient supportive evidence [17], there have been no case reports or series about SRS treatment for cavernous hemangiomas in IAM.
Conclusion
Cavernous hemangiomas in IAM are rare lesions and clinically usually have difficulty distinguishing from vestibular schwannomas based on preoperatively radiological studies. However, cranial nerve deficit disproportionate to their small size may be the most important clinical feature and should be kept in mind. Early recognition and total microsurgical resection may improve the chance of functional recovery, especially for facial paresis.
References
- Magliulo G, Iannella G, Alessi S, Massimo R (2014) Meatal segment of facial nerve and cavernous Ann Otolaryngol Rhinol 1: 1004.
- Mastronardi L, Carpineta E, Cacciotti G, Scipio ED, Roperto R (2016) Cav- ernous hemangioma of the internal auditory canal encasing the VII and VIII cranial nerve complex: case report and review of the literature. Neurosurg Rev 39: 349-354.
- Samii M, Nakamura M, Mirzai S, Vorkapic P, Cervio A (2006) Cavernous angi- omas within the internal auditory J Neurosurg. 105: 581-587.
- Jain R, Robertson PL, Gandhi D, Gujar SK, Muraszko KM, et al. (2005) Ra- diation-induced cavernomas of the brain. AJNR Am J Neuroradiol 26: 1158-1162.
- Safronova MM, Vaz AR, Resende M, Pereira JR, Honavar M, et al. (2009) Cavernous malformation of the internal auditory canal: a diagnostic chal- Otology & Neurotology 30: 1015-1017.
- Sundaresan N, Eller T, Ciric I (1976) Hemangiomas of the internal auditory Surg Neurol 6: 119-121.
- Lenarz M, Durisin M, Kamenetzki P, Becker H, Kreipe HH, et al. (2007) Cav- ernous hemangioma of the internal auditory canal. Eur Arch Otorhinolaryngol 264: 569-571.
- Feng SY, Fan YP, Chen SL, Hong HY, Zhang ZG (2012) Cavernous haeman- gioma of the internal auditory canal: a case Int. Adv. Otol. 8: 470-474.
- Cotton CA, Beall DP, Winter BJ, Fortman BJ, Kirby AB, et al. (2006) Cav- ernous angioma of the cerebellopontine angle. Curr Probl Diagn Radiol 35: 120-123.
- Lo WW, Shelton C, Waluch V, Solti-Bohman LG, Carberry JN et al. (1989) Intratemporal vascular tumors: detection with CT and MR Radiology 171: 445-458.
- Dazert S, Aletsee C, Brors D, Mlynski R, Sudhoff H, et (2005) Rare tumors of the internal auditory canal. Eur Arch Otorhinolaryngo 262: 550-554.
- Watanabe K, Cobb MIH, Zomorodi AR, Cunningham CD, Nonaka Y, et al. (2017) Rare Lesions of the Internal Auditory Canal. World Neurosurg 99: 200-209.
- Capelle HH, Nakamura M, Lenarz T, Brandis A, Haubitz B, et al. (2008) Cav- ernous angioma of the geniculate J Neurosurg 109: 893-896.
- Chamoun R, MacDonald J, Shelton C, Couldwell WT (2012) Surgical ap- proaches for resection of vestibular schwannomas: translabyrinthine, retros- igmoid, and middle fossa Neurosurg Focus 33: 9.
- Jacobson J, Reams C (1991) Neurotologic disease in four patients with nor-mal audiometric findings. Am J Otol 12: 114-118.
- Pappas DG, Schneiderman TS, Brackmann OF, Simpson SC, Chandra Sekar B, et al. (1989) Cavernous hemangiomas of the internal auditory canal. Oto- laryngol Head Neck Surg 101: 27-32.
- Nagy G, Kemeny AA (2013) Stereotactic radiosurgery of intracranial cavern- ous Neurosurg Clin N Am 24: 575-589.
Citation:Huang CC, Chen YN, Lin YW, Tai SH, Chang CC, et al. (2018) Cavernous Hemangioma within the Internal Auditory Meatus: a Small Lesion Makes Severe Neurological Deficit. J Case Repo Imag 2: 006.
Copyright: © 2018 Huang CC, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.


