*Corresponding Author:
Bebiana Faria,
Department of Cardiology, Hospital Da Senhora Da Oliveira-Guimarães, Guimarães, Portugal
Tel: +351 934899908
Email: anafaria@gmail.com
Abstract
In a peripheral hospital without primary angioplasty or invasive mechanical circulatory support, therapeutic options in patients with myocardial infarction complicated with cardiogenic shock or refractory cardiopulmonary resuscitation are very limited.
We report a case of a 59-year-old man with acute myocardial infarction with ST-segment elevation complicated of cardiogenic shock and refractory cardiac arrest, transported with ongoing fibrinolysis to another hospital for rescue percutaneous coronary intervention in cardiopulmonary resuscitation with automated mechanical chest compression. This case highlights the difficulty in managing these critically ill patients in peripheral hospitals without advanced resources and discusses some therapeutic options.
Keywords
Acute coronary syndrome; Cardiac arrest; Cardiogenic shock
Abbreviations
ALS: Advanced Life Support
AMCC: Automated Mechanical Chest Compression
CA: Cardiorespiratory Arrest
CPR: Cardiopulmonary Resuscitation
CS: Cardiogenic Shock
eCPR: Extracorporeal Cardio Pulmonary Resuscitation
PCI: Percutaneous Coronary Intervention
PEA: Pulseless Electrical Activity
STEMI: Acute Myocardial Infarction with ST segment Elevation
Introduction
The acute coronary syndrome is the most common cause of Cardiogenic Shock (CS), mainly through a large zone of myocardial ischemia or a mechanical complication [1]. CS complicates 6-10% of all acute Myocardial Infarction with ST-segment Elevation (STEMI) cases and remains a leading cause of death, within-hospital mortality rates 50% [2,3].
In a peripheral hospital without hemodynamic laboratory or invasive mechanical circulatory support, therapeutic options in patients with myocardial infarction complicated with cardiogenic shock or refractory Cardiorespiratory Arrest (CA) are very limited and not consensual.
Case Report
A 59-year-old man was admitted to the emergency department of a peripheral hospital (without primary angioplasty or mechanical circulatory support capacity) due to oppressive chest pain, breathlessness, associated with an altered state of consciousness, with one hour of symptoms. Physical examination showed non-measurable blood pressure, symmetrical filiform peripheral pulses with a regular frequency of 100 ppm, signs of peripheral poor perfusion with reticular livedo, Glasgow Coma Scale of 10 (E3V2M5), cardiac auscultation without murmurs and pulmonary auscultation with diffuse crackles.
The patient had a personal history of hypertension, obesity, smoking and epilepsy. Medicated with antiepileptics.
A 12-lead electrocardiogram (Figure 1) revealed sinus rhythm with a heart rate of 106bpm, with diffuse ST-segment elevation, more marked in the anterolateral wall. Transthoracic echocardiogram showed severely left ventricular dysfunction with only contraction of the basal segment of the interventricular septum, without evidence of pericardial effusion, flap or mechanical complications.
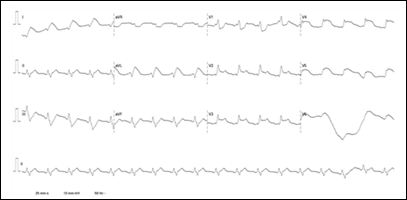
Table 1: Admission 12-lead electrocardiogram revealed sinus rhythm with a heart rate of 106bpm, with diffuse ST-segment elevation, more marked in the anterolateral wall.
Towards these findings, the diagnosis STEMI complicated CS was considered. He received anti-thrombotic loading doses, initiated with noradrenaline and invasive ventilatory support.
During the preparation for transfer the patient to the hospital with primary angioplasty capability, CA was observed in Pulseless Electrical Activity (PEA). Advanced Life Support (ALS) was immediately initiated. Four cycles were performed with no return of spontaneous circulation. At this time, it was decided to do fibrinolysis with tenecteplase, ALS was maintained for about 20 minutes without return of the circulation, always with a PEA. It was placed Automated Mechanical Chest Compression (AMCC) and started transport to the hospital with primary angioplasty capability. After 20 minutes of transport, the patient was admitted to the hemodynamic lab in Cardiopulmonary Resuscitation (CPR) under AMCC, with total CPR time of about 50 minutes and40 minutes after fibrinolysis.
Coronary angiography showed thrombotic occlusion of the left main (Figure 2A), and angioplasty was performed by stent implantation from the left main to the anterior descending artery (Figure 2B). After angioplasty, spontaneous circulation returned. Echocardiogram revealed very severe left ventricular dysfunction and vasopressor support was restarted with increasing doses. Two hours after angioplasty, asystole was verified, which could not be reversed.

Figure 2A: Coronary angiography showed thrombotic occlusion of the left main.
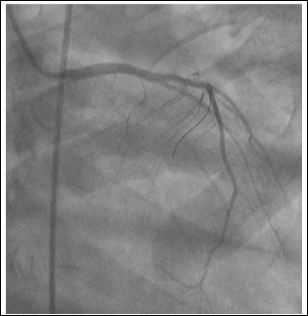
Figure 2B: Coronary angiography after angioplasty with stent implantation from the left main to the anterior descending artery.
Discussion
In STEMI patients presenting with CS in which Percutaneous Coronary Intervention (PCI) mediated reperfusion is estimated to occur>120 min, immediate fibrinolys is and transfer to a PCI center shouldbe considered. In these cases, as soon as arrive at the PCI center, emergent angiography is indicated, regard less of the ST resolution and the time from fibrinolys is administration [2].
Fibrinolytic treatment in the contex to frefractory CA in STEMI is not well established and showed no improvement in survivalat hospital discharge [3,4], however, in this case, it was decided to performs in diagnosis of STEMI was prior to CA andCA was witnessed and promptly assisted.
In these circumstances if a fibrinolytic drug is given, consider performing CPR for atleast 60-90 min before termination of resuscitation attempts [5].
Atbest, standard manual CPR produces coronary and cerebral perfusion that is just 30% of normal. Providing high-quality manual chest compressions can be challenging and there is evidence that CPR quality deteriorates with time. Although there are no differences in clinical out comes compared manual CPR to AMCC devices, but AMCC may enable the delivery of high-quality compression sespecially in difficult circumstances: CPR in a moving ambulance, prolonged CPR (e.g., during fibrinolytic therapy)and CPR during certain procedures (e.g., coronary angiography), many of these characteristics verified in this case [5,6].
Extracorporeal CPR (eCPR) shouldbe considered as rescue therapy for those patients in who minitial ALS measures are unsuccessful and/or to facilitate specific interventions (PCI). Observational studies suggeste CPR for cardia carrest is associated with improved survival when there is a reversible cause for cardia carrest (e.g., myocardial infarction) [5]. Probablye CPR wouldbe a good strategy for this patient, however, the patient was admitted in a hospital without mechanical circulatory support.
There is limited evidence for recommending routine transport to a hospital with ongoing CPR in the case of CA during STEMI. The decision will depend on patient selection and must take into consideration a realistic chance of survival, witnessed cardia carrest with an initial shock able rhythm, by stander CPR and intermittent return of spontaneous circulation. There are no large out come studies available, but small case series suggest benefit in the seselected cases [7].
In this clinical case, Ca was witnessed and immediately assisted, fibrinolytic treatment was started, and despite being a non-defibrillate rhythm, the patient was young without severeco-morbidities,within one hour of symptom onset. As we were facing a refractory CA, under fibrinolytic treatment in the hospital without mechanical circulatory support capacity, with a hemodynamic labat 20 minutes distance, and it was possible to ensure high-quality cardiopulmonary resuscitation with the AMCC during transportation, it was decided to transport the patient in CPR to rescue PCI.
After left main angioplasty spontaneous circulation was observed, however, a few hours later the patient died. In this case, the cardiac arrest would probably have been more secondary to pump failure than ischemia, given the rhythm of arrest. Possibly the outcome could be different if a defibrillate rhythm was presented.
Conclusion
Transport of the patient to primary angioplasty in CRP is not consensual, there are not controlled studies confirming the outcome, however, reports of small series suggest that there may be a benefit in selected cases, especially, when de CA is seen and when high-quality cardiopulmonary resuscitation is possible. The AMCC allows ensuring high-quality CPR, especially in long resuscitation. In this case, the AMCC enabled coronary revascularization and consequently the return of spontaneous circulation. However, the degree of left ventricular dysfunction, more than ischemia, determined the prognosis of the patient.
References
- Nikolaoua N, Arntz HR, Bellou A, Beygui F, Bossaert LL, et al. (2015) European resuscitation council guidelines for resuscitation 2015 Section 8. Initial management of acute coronary syndromes. Resuscitation 95: 264-277.
- Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, et al. (2018) 2017 ESC guidelines for the management of acute myo- cardial infarction in patients presenting with st-segment elevation: The task force for the management of acute myocardial infarction in patients presenting with st-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 39: 119-177.
- Bernoche C, Timerman S, Polastri T, Giannetti NS, Siqueira AW, et (2019) Atualização da diretriz de ressuscitação cardiopulmonar e cuidados cardiovasculares de emergência da sociedade brasilei- ra de cardiologia - 2019. Arq Bras Cardiol 113: 449-663.
- Böttiger BW, Arntz HR, Chamberlain DA, Bluhmki E, Belmans A, et al. (2008) Thrombolysis during resuscitation for out-of-hospital cardiac N Engl J Med 359: 2651-2662.
- Soar J, Nolan J, Böttiger B, Perkins GD, Lott C, et al. (2015) Euro- pean resuscitation council guidelines for resuscitation 2015: Sec- tion Adult advanced life support. Resuscitation 95: 100-147.
- Lafuente-Lafuente C, Melero-Bascones M (2013) Active chest com- pression-decompression for cardiopulmonary Co- chrane Database Syst Rev.
- Truhlár A, Deakinc C, Soar J, Khalifa GEA, Alfonzo A, et al. (2015) European resuscitation council guidelines for resuscitation 2015: Section 4. Cardiac arrest in special circumstances. Resuscitation 95: 148-201.
Citation:Faria B, Fernandes M, Ribeiro S, Lourenço A (2020) Automated Mechanical Chest Compression as a Bridge to Primary Percutaneous Coronary Intervention: Case Report. J Case Repo Imag 4: 012.
Copyright: © 2020 Faria B, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.


