*Corresponding Author:
Dipika Mohanty,
Senior Consultant, Department of Laboratory Medicine, Apollo Hospitals, Bhubaneswar, Odisha, India
Tel: +080 93060025
E-mail: mohantydipika09@gmail.com
Abstract
This present study reports severe renal derangement in four cases of Sickle cell Anemia during vaso-occlusive crisis. All were Arab Indian haplotype.
All the cases had low Hemoglobin level and high reticulocyte and LDH level. Examination of urine revealed proteinuria, red cells in excess, hyposthenuria. High levels of serum urea ranging from 47 to 200mg/dl, Creatinine 0.58 to 6.2mg/dl and urea nitrogen 22 to 93mg/dl. The U.S abdomen mainly showed bilateral enlargement of kidney with Acute renal parenchymal changes. The kidney biopsy in one of the cases revealed Focal and Segmental Glomerulosclerosis (FSGS), cellular and fibrocellular crescents. Capillary lumina contained sickle RBC. Interstitial fibrosis and tubular atrophy was approximately 20 to 30%. Thus renal derangement during sickle cell crisis is not uncommon in India. However one has to be aware of this fact and has to treat it aggressively since it is an Emergency.
Keywords
Renal derangement; Renal function test; Sickle cell anemia; Vaso-Occlusive crisis
Introduction
Sickle cell disease substantially alter renal structure and function, and causes various renal syndromes and diseases. Such diverse renal outcomes reflect the uniquely complex vascular pathobiology of SCD and renal medulla because of its hypoxic, acidotic and hyperosmolar condition. The clinical manifestations of sickle cell disease vary tremendously between and among the major genotypes. The Arab-Indian haplotype prevalent in India is believed to have milder clinical manifestations. Paucity of reports from India regarding renal function derangement in sickle cell anemia cases during Vaso-occlusive crisis prompted us to report this present study. This will help us in taking necessary timely interventions in cases of SCD with renal derangement and prevent chronic or end stage renal disease. So, the present study was planned for observing the kidney function during and after the Vaso-Occlusive Crisis in a stable state. Out of sixty sickle cell homozygous cases reported to Apollo hospitals between June 2018 to July 2019 four cases showed severe renal function and structural derangement during Vaso-Occlusive Crisis. Out of four, two were males and the rest two patients were females. Age of the patients ranged from 20 to 60years. All patients presented with fever, weakness, generalized body and joint pain, shortness of breath & hematuria. Duration of symptoms varied from 4 to 6 days. Sickle cell crisis was detected by clinical presentation i.e. body & joint pain, jaundice , pallor and alteration of laboratory parameters like decrease in Hb level & increase in serum bilirubin( total & unconjugated) , Reticulocyte count, LDH ,circulating sickle cells in peripheral blood ( 5 to 6 or more/high power field) & nucleated RBCs. The Hemoglobin was reduced in all four cases ranging from 5.7 to 9 g/dl. Total leucocyte count was raised in all cases (range 5.5 to 15.5×103/ cmm) with neutrophilia. Platelet count of all the cases were within normal limit (range 144-174x103/ cmm), raised LDH & reticulocyte count (LDH–1000 to 3000 I.U/L, Retics -5.57 to 17.3%). Three out of four cases initially presented with proteinuria and all four cases had hematuria. Twenty four hours urinary protein ranged from 11 to 14 g/day. All the cases showed derangement of kidney function parameters (Table 1). Ultrasonography of abdomen revealed in two cases bilateral enlargement of kidney with acute renal parenchymal changes and three out of four cases showed bilateral pleural effusion.
Out of four cases, one had undergone renal biopsy. Light microscopy showed 16 glomeruli with associated tubules and vessels; of which two showed Focal and Segmental Glomerulosclerosis (FSGS). Another four glomeruli showed partial to near total sclerosis predominantly in perihilar region. One glomerulous showed a cellular crescent and three showed fibrocellular crescents. Capillary lumina contained sickled RBCs as well as normal RBCs. Interstitial fibrosis & tubular atrophy was approximately 20-30% (Figure 1). Fine granular fluorescence was present across peripheral capillaries and adjacent mesangium for IgM (Trace/+1) and C3c (+1) on immunofluorescence microscopy. So, final diagnosis was sickle cell glomerulopathy with focal and segmental glomerulosclerosis superadded by acute interstitial nephritis with crescents.
Hence, present study establishes the fact that in about 6.6% of homozygous sickle cell anemia cases there is gross derangement of renal function Table 1 during VOC. In these cases no other co-morbid factors like Type II diabetes and hypertension and autoimmune disease was present. This is the first report from India objectively demonstrating FSGS in sickle cell anemia during crisis. It may be noted that the renal function returned to normal after 2 weeks in these cases except the specific gravity of the urine, which remained low (hyposthenuria). These findings are in agreement with the reports from other countries like USA, Africa [1-4]. Haematuria and loss of concentrating ability are the most frequent renal complications seen in sickle cell anemia cases. The limitation of the present study is the small number of SCA cases.
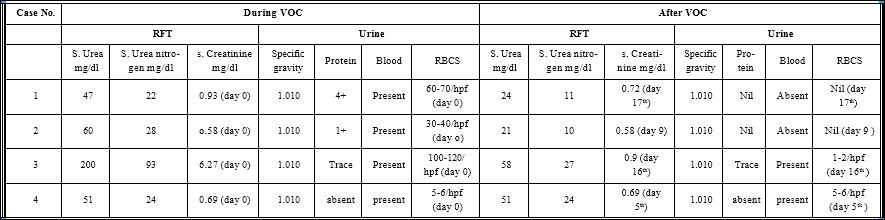
Table 1: Comparison of Different Renal Parameters during and After Vaso-Occlusive Crisis (VOC).
Abbreviations: RFT- Renal function test, S.U- Serum urea, S.UN- Serum urea nitrogen, S. creat-Serum creatinine, S.Gr-Specific gravity, Pr-protein, Bl-Blood, mg-milgram, dl-deciliter.
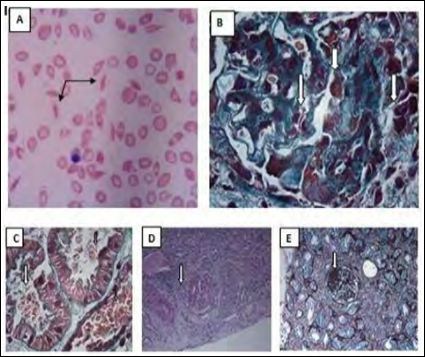
Figure 1: A) 400X peripheral smear showing features of sickle cell crisis-Leishman stain; B) 1000X Sickled RBCs in cresentric glomerular capillary- MT Stain (Masson Trichrome); C) 1000X Sickled RBCs in tubules-MT Stain; D) 200X Cellular crescents-PAS Stain (Periodic Acid Schiff Stain); E) 200X FSGS and IFTA - JMS Stain (Jones methenamine silver stain).
Furthermore this present study brings out the fact that renal involvement during sickle cell crisis is not uncommon. However, one has to look for the renal derangement so that proper timely management of the same can be undertaken for recovery of the cases. We stress here the utility of routine and microscopic urine examination of SCD patients for early detection of renal involvement. Biopsy should be undertaken to understand the extent of renal glomerular involvement and the degree of interstitial fibrosis & tubular atrophy. This will determine the long term prognosis as well as the appropriate treatment protocol required. Also the cellular crescent if present as in our case, requires aggressive therapy to salvage the kidney as it is a medical emergency.
References
- Nath KA, Hebbel RP (2015) Sickle Cell Disease: Renal manifestations and Nat Rev Nephrol 11: 161-171.
- Becker AM (2011) Sickle cell nephropathy: Challenging the conventional wis- Pediatr Nephrol 26: 2099-2109.
- Drawz P, Ayyappan S, Nouraie M, Saraf S, Gordeuk V, et al. (2016) Kidney Disease among patients with sickle cell disease, hemoglobin SS and SC. CLIN J Am Soc Nephrol 11: 207-215.
- Ranque B, Menet A, Diop IB, Thiam MM, Diallo D, et al. (2014) Early renal damage in patients with sickle cell disease in sub-saharan Africa: A multina- tional, prospective, cross-sectional study. Lancet Haematol 1: 64-73.
Citation: Jyotsna P, Dipika M, Nachiketa M, Sreeya D (2020) Alteration in Renal Function and Structure in Cases of Sickle Cell Anemia in India during Vaso-Occlucive Crisis (Voc). J Hematol Hemother 5: 011.
Copyright: © 2020 Jyotsna P, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and re- production in any medium, provided the original author and source are credited.