*Corresponding Author:
Anubha Bajaj,
Department of Histopathology, AB Diagnostics, New Delhi, India
Tel: +91 9811693956
Email: anubha.bajaj@gmail.com
Abstract
Nevus of Ota is an extensive, blue-tinged patch arising due to melanocytic dissemination amidst dermal collagen fibres engendering dermal pigmentation. Eyelids, bulbar and palpebral conjunctiva, sclera, forehead, alae nasi, scalp, ears, cheek and palatal mucosa are incriminated. Classical Tanino’s classification incorporates features as gender, age at disease commencement, applicable therapy, proportionate discolouration, eyelid involvement and alternative treatment modalities, apart from laser therapy. Dermal accumulation of intensely pigmented, dendritic melanocytes and melanophages is encountered. With efficacious therapy, an estimated 40.3% instances are denominated as cured or excellent alleviation, around 29.9% candidates display good improvement, nearly 16.4% subjects depict fair improvement, roughly 4.5% individuals delineate a poor or inferior outcome and approximately 9.0% subjects lack modification. Cryosurgery, surgical excision, skin grafts, dermaabrasion, cryo-therapy and topical hydroquinone are beneficially employed. Laser photo-thermolysis demonstrates variable response.
Keywords
Cryosurgery; Dermal pigmentation; Nevus of ota
Introduction
Nevus of Ota was initially scripted by Ota in 1939 and is described as an extensive, blue-tinged patcharising on account of melanocytes principally disseminated between dermal collagen fibres with consequent dermal pigmentation. Nevus of Ota essentially incriminates the eyelids, bulbar and palpebral conjunctiva, sclera, forehead, alae nasi, scalp, ears and mucosal surfaces of cheek and palate. Nevus of Ota is additionally designated as oculodermal melanocytosis or nevus fuscoceruleus opthal mom axillaris [1].
Epidemiology and Classification
Nevus of Ito was initially described by Ito in 1954 and simulates nevus of Ota although distribution of lesions is along the posterior and lateral supraclavicular nerves besides lateral cutaneous brachial nerve. Nevus of Ito commonly implicates the shoulder, lateral neck and supraclavicular region [1,2]. Nevus of Ota is exceptional in Caucasians and males whereas a female preponderance is observed with an estimated 80% of lesions discerned within the female population. Nevus of Ota is generally cogitated in Asians, Hispanics, Africans and native Americans. Approximately 60% of subjects demonstrate congenital lesions and an estimated 60% of candidates are accompanied by dermal and ocular incrimination [1,2]. Nevus of Ota can coexist with nevus of Ito. Nevus of Ota and Ito are primarily dermal melanocytic nevi. With predominant incrimination of Asian subpopulation, nevus of Ota usually implicates around 0.02% to 0.8% of Asians with a prevalence of 0.8% within the Japanese. Tanino’s classification is acceptable for categorizing nevus of Ota. Described by Tanino in 1939, subdivisions are contingent to incrimination of diverse cutaneous surfaces. Cogent characteristics evaluated by Tanino’s classification are gender, age of disease onset and pertinent therapy, proportionate discolouration achieved by the nevus, incrimination of eyelids and adoption of alternative treatment modalities, apart from laser therapy. However, several instances remain unexplained with the classification [1,2].
Cogent classifications universally accepted classifications for cat- egorizing nevus of Ota are comprised by Tanino’s classification, Peking Union Medical College Classification and Three Point Severity Scale Tanino’s classification is designated as Type 1a: Incrimination of eyelids, periorbital and temporal region Type 1b: Incrimination of zygomatic area, infra-palpebral fold, nasolabial fold and lower eyelid. Type 1c: Incrimination of forehead region. Type 1d: Incrimination of nostrils, alae nasi. Type II: Incrimination of upper and lower eyelids, periocular and zygomatic region, temple and cheek Type III: Incrimination of scalp, forehead, eyebrow and nose Type IV: Enunciation of bilateral lesions. Hori’s nevus: Acquired bilateral nevus of Ota like macules. Sun’s nevus: Acquired unilateral nevus of Ota [2,3]. Peking Union Medical College Classification (PUMCH) is comprised of sub- divisions pertaining to the innervation of trigeminal nerve. Type 1: Demonstrates pigmentation within a singular branch of trigeminal nerve. Type II: delineating pigmentation within two branches of tri- geminal nerve. Type III: exhibiting pigmentation contingent to three branches of trigeminal nerve. Type IV: bilateral variant of nevus of Ota [2,3]. Type V: nevus of Ota with accompanying cutaneous complications. Three point severity scale is a categorization denominated with ≈ mild lesions encompassing betwixt ≤one third to one half of face ≈ moderate disease implicating betwixt >one third to ≤ two thirds of face severe disease exceeding >two thirds of facial incrimination. Tanino’s classification is applicable since 1939 and adequately describes nevus of Ota and the classification is contingent to disease severity with pertinent, arbitrary subdivisions of the face [2,3]. Discrepancies of Tanino’s method of categorization are ambiguity of diverse segments of the body, unsatisfactory proportion of coverage and a lack of consensus amongst dermatologists. Approximately 19.7% subjects may not be adequately categorized with Tanino’s classification. The contemporary classification of (PUMCH) incorporates features such as innervated regions of trigeminal nerve, symmetry of pigmentation and complications encountered with nevus of Ota as vitiligo and haemangiomas, even though certain instances may be inappropriately categorized. Nevertheless, the designated 15 subtypes appear exuberant and clinical outcomes contingent to severity scale lack concordance [2,3]. Currently, a singular, ideal classification is lacking. Possible factors influencing various classification systems are presence of eyelid lesions, bilateral nevi, comparative Tanino’s classification, enumerable treatment sessions, photo-type of skin, and colour of lesions and age of therapeutic commencement. Frequency of treatment is a cogent factor in lesion improvement as frequent sessions result in superior outcomes. Occurrence of eyelid lesions lack concurrence with disease severity, classification and clinical outcomes [3]. Tanino’s classification is not concordant with percentage of disease alleviation although eye-lid lesions and Tanino’s classification appear concurrent with clinical outcomes. Age of therapeutic initiation and clinical outcomes lack concordance. Contingent to three point’s severity scale of classification, an estimated 86.6% of subjects demonstrate mild to moderately severe lesions, usually occupying ≤ two thirds of the face. Tanino‘s classification categorizes around 64.2% of lesions whereas PUMCH classification can characterize nearly 91% patients. However, aforesaid classifications lack concurrence, especially with frequency of excellent outcomes (Table 1) [2,3].
|
|
Three point scale |
Tanino’s classifi- cation |
PUMCH classification |
|
Categoriza- tion |
Extent of facial involvement |
Frequency of structural incrim- ination |
Pattern of pigmentation along trigeminal nerve, symmetry, complications |
|
Enumeration |
Three |
Seven |
Fifteen |
|
Proportion |
100% |
64.2% |
91% |
|
Favourable features |
Convenient, simple, valid, reproducible |
Popular and conventional |
Extensive coverage, combined and symmetric features, well-designed |
|
Unfavourable features |
Poorly defined pathophysiology, bilateral and com- bined lesions lack concordance, lack of consensus |
Inadequate coverage, ambig- uous demarcation betwixt subtypes, conventional and imperfect |
Extensive categories with exclusion of specific subjects |
Table 1: The selected concentrations for each heavy metal.
Clinical Elucidation and Histological Elucidation
Distribution of lesions is commonly restricted to first and second branches of trigeminal nerve whereas lesions upon the trunk are exceptional [1,2].
Unilateral or bilateral, brownish or blue-tinged discoloration is exhibited upon facial surfaces, particularly within zones innervated by trigeminal nerve. Nevus of Ota, as designated in 1939, is described as an uncommon hamartoma appearing within periorbital and temporal cutaneous surfaces [4].
Commonly, a macule circumscribed with irregular, blue grey pigmentation is delineated, situated within the distribution of first and second division of trigeminal nerve. Nevus of Ota is a persistent lesion and extends in a localized manner. Prominence of lesion enhances within the elderly and during pubertal or post menopausal phase. Nevus of Ota is commonly associated with ipsilateral glaucoma, intracranial melanocytosis and exceptionally with cutaneous, ocular or intracranial melanoma and vascular nevus [4,5] Transient pigmentary modifications occur in an estimated 8% to 25% subjects whereas around 3% individuals demonstrate atrophic scarring. Evaluation of percentage of lesion reoccurrence necessitates an extended follow up. Lack of concurrence of classification with clinical outcomes emerges in minimal, discernible instances. Histological analysis of nevus of Ota is recommended for appropriate classification [4,5]. Upon cogent histological examination, a melanocytic hamartoma is enunciated within the dermis. Additionally, dermal accumulations of in tensely pigmented, dendritic melanocytes and melanophages are encountered. Also, dissecting bundles of collagen fibres are exemplified within the reticular dermis [5,6]. Histological features of nevus of Ota are well illustrated in Figures 1 to 9.

Figure 1: Melanocytosis with nevus of Ota.
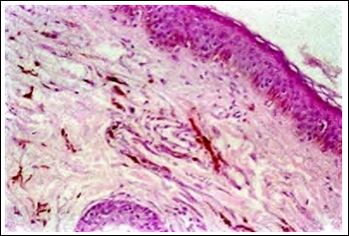
Figure 2: Nevus of Ota with accumulation of dermal melanophages, melanocytes and dermal collagen fibres.
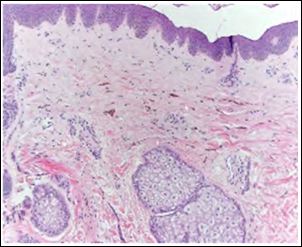
Figure 3: Nevus of Ota with aggregates of dermal melanophages, melanocytes, dermal collagen and an attenuated superimposed epithelium.
Differential Diagnosis
Nevus of Ota requires segregation associated facial dermal melanocytosis such as acquired bilateral nevus of Ota- like macule (Hori’s nevus), café-au lait-patch and speckled lentiginous nevus [2].
Prognostic Outcomes photographs of lesion are obtained at initial and ultimate session and graded as≈cured or excellent wherein lesions demonstrate 95% to 100% improvement ≈ good response wherein lesions display 75% to 94% improvement ≈ fair response of lesions accompanied by 50% to 74% alleviation ≈ poor response of sions associated with 25% to 49% alleviation ≈ negligible modification of lesions with 0% to 24% improvement.
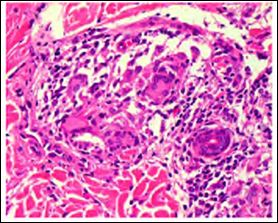
Figure 4: Nevus of Ota with accumulation of melanocytes and melanophages within the dermis in addition to collagen fibres situated within the reticular dermis.
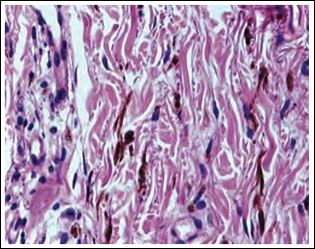
Figure 5: Nevus of Ota with nests of melanocytes and melanophages within the dermis along with aggregated collagen fibres.
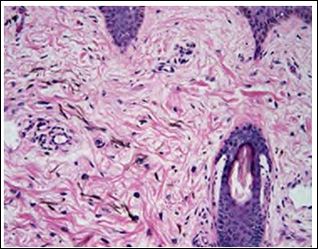
Figure 6: Nevus of Ota with dissemination of melanocytes and collagen fibres within the reticular dermis.
Individuals are subdivided into a “cured group” and “unattained group”. The cured group is composed of young individuals with minimal incrimination of eyelids, necessitate frequent sessions of laser therapy and are commonly subjected to a singular mode of laser technique, in contrast to the unattained group [7,8]. With the adoption of efficacious therapy, an estimated 40.3% instances are denominated as cured or excellent alleviation, around 29.9% candidates display good improvement, nearly 16.4% subjects depict fair improvement, roughly 4.5% individuals as poor or inferior outcome and approximately 9.0% subjects are devoid of alteration of lesions [2,3]. An estimated 3% of treated candidates demonstrate complications such as emergence of a depressed scar. Around 26.8% subjects delineate varying proportions of corrugated cutaneous surfaces. Improvement of pigmentation along with alleviation of cutaneous roughness is a necessary therapeutic target while treating nevus of Ota [1,2].
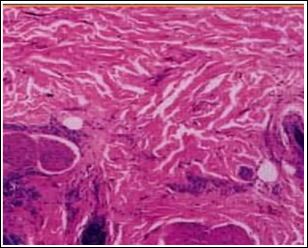
Figure 7: Nevus of Ota with accumulation of collagen within the reticular dermis and disseminated melanophages.
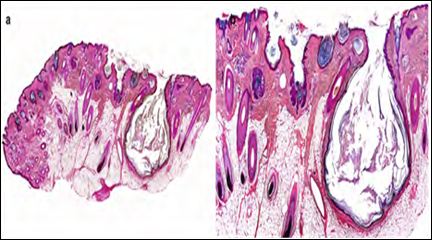
Figure 8: Nevus of Ota with collagen fibres within the reticular dermis and dispersal of melanocytes, melanophages with an attenuated superimposed epithelial lining.
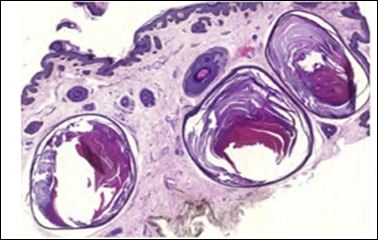
Figure 9: Nevus of Ota with clusters of pigmented melanocytes disseminated within reticular dermal fibres of collagen.
Therapeutic options diverse treatment options are available and can be adapted for managing the infamous “patch on the face”. In the preliminary phase, cryosurgery, adequate surgical excision, skin grafts and derma-abrasion are typically employed and beneficial. Appropriate selection of contemporary therapies for treating nevus of Ota can be challenging [6]. Cogent therapy is comprised of utilization of cosmetic products. Combination of derma-abrasion and carbon dioxide snow methodology can be utilized. However, adoption of cryosurgery or microsurgery induces scarring whereas chemical bleaching incurs depigmentation, hence aforesaid procedures are not recommended [6,7]. Various contemporary laser techniques are applicable in treating benign pigmentary lesions. The Q- Switched (QS) laser system is suitable for treating nevus of Ota as it is associated with minimal scarring and superior outcomes. Multiple laser systems can be variously combined with QS lasers in decimating nevus of Ota. Extreme, brief emissions of QS lasers are absorbed by melanosomes and are imbued with sufficient energy to decimate incriminated soft tissue with minimal collateral thermal damage wherein aforesaid technology is nomenclated as “selective photo-thermolysis”. Multiple sessions of laser photo-thermolysis are adopted in order to circumvent further darkening of skin and lesion extension, following a preliminary diagnosis. Laser therapy demonstrates variable responses in different subtypes. Application of QS lasers as a singular, efficacious treatment modality for nevus of Ota is accompanied by significant improvement of lesions, particularly with the utilization of 1064 QSNY laser [6,7]. Cogent laser therapy can activate laser induced decimation of pigment along with regeneration of dermal collagen fibres. Thus, dermal fibrosis ensues in addition to disappearance of cutaneous pigmentation following laser irradiation along with deterrence of residual pigment. Long pulsed and quasi- long- pulsed laser techniques can be incorporated within the therapy. Long pulsed lasers induce and stimulate collagen remodelling on account of concurrent thermal and mechanical effects [7,8]. Utilization of Intense Pulsed Light (IPL) with 560 nm filter can be employed, contingent to aforesaid mechanism, wherein diffuse epi- dermal necrosis occurs on account of pertinent distribution of energy. Appropriate spot sizeand laser pulse fluence is required for comprehensive alleviation of lesions [8]. Efficacy of laser treatment can be assessed by evaluating factors such as varieties of laser modalities and frequency of therapeutic sessions. Lesion alleviation exceeding > 95% can be accepted as a reasonable therapeutic end point [1,2]. Adoption of various combinations of laser therapy, in the absence of homogeneity can affect clinical results and attenuate significance of various therapies. Amalgamated laser methodologies can be adopted for superior cosmetic outcomes, which may not be significant or consistent. Minimally pigmented nevus of Ota can be cured with consistent and repetitive laser therapy [8]. Nevus of Ota can be also managed with adjuvant modalities such as cryotherapy and topical hydroquinone. Nevertheless, therapeutic outcomes of different modalities are identical [8].
References
- 1.Ota M, Tanino H (1939) Nevus fusco-caeruleus ophthalmo- maxil- Tokyo Med J 63: 1243-1245.
- 2.Nam JH, Kim HS (2017) Treatment and classification of Nevus of Ota: A seven year review of a single institution’s experience. Ann Dermatol 29: 446-453.
- 3.Ho SG, Chan HH (2009) The Asian dermatologic patient: Review of common pigmentary disorders and cutaneous disease. Am J Clin Dermatol 10: 153-168.
- 4.Wang HW, Liu YH, Zhang GK, Jin HZ, Zuo YG, et al. (2007) Anal- ysis of 602 Chinese cases of nevus of Ota and the treatment re- sults treated by Q-switched alexandrite laser. Dermatol Surg 33: 455-460.
- 5.Seo HM, Choi CW, Kim WS (2015) Beneficial effects of early treat- ment of nevus of Ota with low-fluence 1064-nm-Q- switched Nd: YAG Dermatol Surg 41: 142-148.
- 6.Choi JE, Lee JB, Park KB, Kim BS, Yeo UC, et al. (2015) A retro- spective analysis of the clinical efficacies of Q-switched alexandrite and Q-switched Nd: YAG lasers in the treatment of nevus of ota in Korean J Dermatolog Treat 26: 240-245.
- 7.Zong W, Lin T (2014) A retrospective study on laser treatment of nevus of ota in chinese children--a seven-year follow-up. J Cosmet Laser Ther 16: 156-160.
- 8.Yoo MG, So BJ, Lee JM, Kim DH, Park HC, et al. (2015) Influence of pulse type on subcellular selective photothermolysis of melano- somes in adult zebrafish skin following 1064-nm Q-switched Nd: YAG laser irradiation: A pilot Ann Dermatol 27: 230-232.
Citation:Bajaj A (2020) Aberrant Dermal Pigmentation-Nevus of Ota Recapitulated. J Case Repo Imag 4: 022.
Copyright: © 2020 Bajaj A. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.


