*Corresponding Author:
Alexis E Carrington,
Department of Dermatology, Univer- sity of California-Davis, California, USA
Tel: +1 9167346111
Email: aecarrington@ucdavis.edu
Abstract
Leprosy or Hansen’s disease is a chronic granulomatous infection caused by M. Leprae and M. Lepromatosis transmitted primarily through respiratory droplets. Although it has been classified under two distinct groups, Multibacillary (MB) and Paucibacillary (PB), there have been reports of clinical and histological presentations of both types. Here, we present a case of such an occurrence of a 23- year old female with a rash on the right leg for a year, along with an ill-defined right midline septal, friable mass. Biopsies of both location showed borderline tuberculoid leprosy. Given her presentation, of an abundance of bacteria on biopsy, she received a classification of possibly multibacillary, however had presentations consistent with Paucibacillary. Her exposure history was negative. This case shows there can be variations in presentations of leprosy. This occurrence emphasizes the importance of a comprehensive assessment, factoring in histological and sensory presentation, in addition to lesion presence.
Keywords
Hansen’s disease; Leprosy; Multibacillary; Paucibacillary
Introduction
Leprosy or Hansen’s disease is a chronic granulomatous infection caused by M. leprae and M. lepromatosis transmitted primarily through respiratory droplets. Although it has been classified under two distinct groups, Multibacillary (MB) and Paucibacillary (PB), there have been reports of clinical and histological presentations of both types [1,2]. Here, we present a case of such an occurrence.
Clinical Synopsis
A 23-year old female with no past medical history presented with a rash on the right leg for a year. She stated the rash was initially red then faded to dark spots, endorsing slow spreading. There was no associated dryness, pruritus, pain or peeling. She had a five month history of epistaxis, evaluated by ENT and found to have an ill-defined right midline septal, friable mass submitted for biopsy with results pending during this clinical visit. She did not have any prior treatment for the rash or epistaxis. Social history was significant for immigrating from Vietnam to California at age seven and has not traveled since nor any contact with armadillos. Review of systems was positive for loss of sensation on right knee otherwise negative.
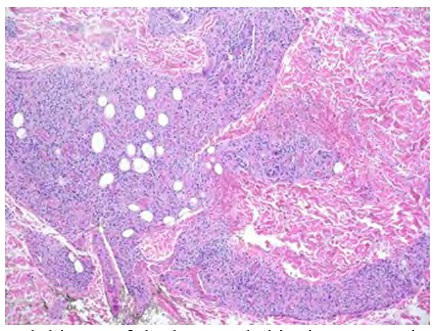
On examination, the patient had a dull erythematous to violaceous, hypertrophic nodule associated with slightly hyperpigmented, blanchable reticulated patches on the right thigh, knee and shin (Figure 1). She had decreased touch sensation over the affected areas and slight thickening of the right common peroneal nerve. ESR was found to be elevated (56mm/h), otherwise labs including Glucose 6 Phosphate Dehydrogenase, Quantiferon® TB Gold Plus, Hep C Antibody and Hep B surface antigen were within normal limits. Biopsy of the right nasal cavity biopsy showed focally ulcerated squamous epithelium with acute and lymphohistiocytic inflammation with abundant acid-fast bacilli (Figure 2a). Both the right knee and shin punch biopsy showed sausage-shaped granulomatous dermatitis following neurovascular bundles, highly suspicious for tuberculoid leprosy (Figure 2b). She received a diagnosis of Borderline Tuberculoid Leprosy, possibly multibacillary given the presence of an abundance of bacteria on biopsy. Treatment plan included Multidrug Therapy (MDT) of dapsone 100mg daily, rifampicin 600mg once monthly, and clofazimine at 300mg monthly along with 50mg daily for a period of one year and referral to CDC leprosy clinic in Los Angeles. Given clofazimine wasn’t obtainable, her current therapy includes Minocycline (100mg daily), Dapsone (100mg daily), Rifampicin 600mg once a month for 2 years.
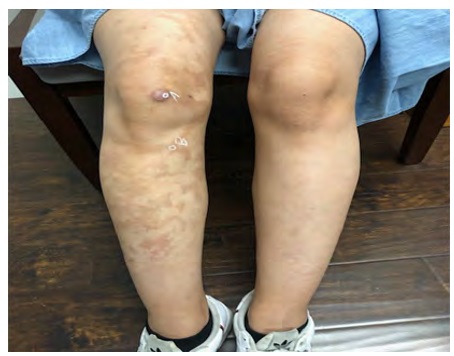
Figure 1: Dull erythematous to violaceous, hypertrophic nodule associated with slightly hyperpigmented, blanchable reticulated patches on the right thigh, knee and shin.
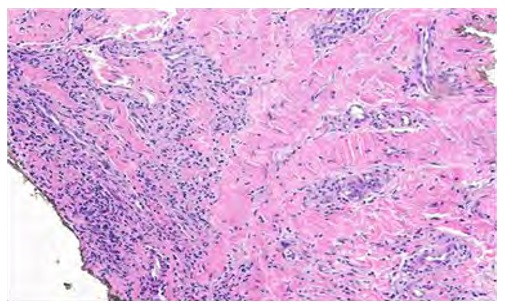
Figure 2a: Biopsy of the right nasal cavity showed focally ulcerated squamous epithelium with acute and lymphohistiocytic inflammation with abundant ac- id-fast bacilli.
Discussion
This case is of interest given the possibility of being either PB or MB in nature. According to the World Health Organization (WHO) Classification of leprosy, PB presents as one to five lesions, hypoesthesia, asymmetrical distribution and negative bacterial smears at all sites; multibacillary presents as positive smear with greater than five lesions and symmetrical distribution [3]. Our patient presented with both abundant bacteria, two lesions, asymmetrical distribution and hypoesthesia, creating a mixed presentation favoring both of the WHO’s classifications.
Although the WHO classification was tailored for areas with limited diagnostic modes, some deem the use of that classification as inappropriate given variations of PB and MB presentations [4]. Several reports have demonstrated MB classification in patients with 1-5 lesions. One study of 62 leprosy patients with 1-5 lesions showed about 24% classified under MB, causing a call to perform comprehensive clinico-bacteriological assessment, especially given MB is treated more aggressively than PB leading to possible mistreatments [5].
The lack of recent exposure to leprosy or armadillos is another intriguing feature of this case. Although she immigrated from Vietnam, she denied any visitation since. Interestingly, the presence of leprosy in Vietnam has significantly changed since 1983 following the use of MDT [6]. In addition, several other cases of leprosy have occurred without any exposure, suggesting that a significant exposure is not always present [7].
Conclusion
This case shows there can be variations in presentations of leprosy. This occurrence emphasizes the importance of a comprehensive assessment, factoring in histological and sensory presentation, in addition to lesion presence.
References
- 1. Rao PN, Pratap D, Ramana Reddy AV, Sujai S (2006) Evaluation of leprosy patients with 1 to 5 skin lesions with relevance to their grouping into paucibacillary or multibacillary Indian J Dermatol Venereol Leprol 72: 207-210.
- 2. Kar PK, Arora PN, Ramasastry CV, Sayal SK, Dhaka RS (1994) A clini- co-pathological study of macular lesions in leprosy. Indian J Lepr 66: 435-442.
- 3. Crecelius EM, Burnett MW (2019) Leprosy (Hansen’s Disease). J Spec Oper Med 19: 105-107.
- 4. Ansari AS, Saxena K, Singh KK, Choudhary A, Singh A, et al. (2020) Clinicobacteriological evaluation of leprosy patients with 1-5 skin le- Int J Mycobacteriol 9: 209-211.
- 5. Bolognia JL, Jorizzo JL, Schaffer JV, Callen JP, Cerroni L, et (2012) Dermatology. Elsevier London, UK.
- 6. Khang TH, Thao NM, Doanh LH (2019) Epidemiology of leprosy in viet- nam and the effectiveness of Multidrug Therapy (MDT) in the manage- ment of the disease. In: Rodriguez-Morales AJ (eds.). Current topics in neglected tropical diseases. IntechOpen, London, UK.
- 7. Aslam S, Peraza J, Mekaiel A, Castro M, Casanas B (2019) Major risk factors for leprosy in a non-endemic area of the United States: A case ID Cases 17.
Citation:Carrington AE, Sivamani RK (2021) A Mixed Presentation of Paucibacillary and Multibacillary Leprosy. J Case Repo Imag 5: 032.
Copyright: © 2021 Carrington AE, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.


