*Corresponding Author:
Jan David Süss,
Department of Vascular and Endovascular Surgery, St.-Antonius-Hospital Eschweiler, Eschweiler, Germany
Tel: +49 15222757688
E-mail: jandsuess@yahoo.de
Abstract
Failed needle cannulation of AVF due to insufficient maturity of the vein can be caused by outflow obstruction. These stenoses are common in the central venous system or cephalic arch but also seen in the upper arm in case of forearm fistula. In our opinion, competitive flow of well-developed collaterals and elbow perforating vein would be the reasons for immaturity. In the overview of diagnostics, we did not recognize peripheral outflow obstruction.
Keywords
Arteriovenous fistula failure; Hemodialysis; Perforating vein; Peripheral outflow obstruction
Introduction
Physical examination in combination with medical history are the first steps for detecting access failure [1]. Second step should be duplex ultrasound access examination. It is important performing gradually diagnostic. Finally, invasive methods such as fistulography should be performed [2].
Common mechanism of access failure is venous out flow stenosis [3]. Central venous obstruction in subclavian, axillary or brachioce- phalic veins is common. In cases of radio-cephalic forearm fistula, the out flow obstruction can be located at the upper arm. Therefore, the assessment of flow pattern in the outflow vein is necessary. Develop- ment of collaterals of the forearm are hinds (signs) of a main outflow obstruction. Diagnostic testing must be performed to assess the cause of such an obstruction. Outflow near the elbow and beyond has to be evaluated.
At first look, high flow rate can mask such out flow obstruction due to the three veins (elbow perforator, basilic vein, cephalic vein) that can keep the forearm out flow intact.
We present a case in which unrecognized out flow obstruction at the upper arm in combination with rash indication for surgery risked the occlusion of the fistula.
Case Report
A 66-year-old male patient was sent to our department by his nephrologist, because of failure of maturation of the fistula. In December 2017, the creation of a distal forearm fistula (radiocephalic AVF) was performed in a different institution. A surgical revision of stenosis of the anastomosis and insufficient maturation were performed by creating a new fistula proximal at the forearm in our institution in May 2018.
After surgical revision, needle cannulation of the cephalic vein was still unsuccessful. Dialysis was carried out by a tunneled catheter.
At time of presentation a continuous thrill was present. The duplex ultrasound showed diameter of the cephalic vein of the forearm to be 4.5 to 6.0 mm. In addition, we verified a deep subcutaneous course as well as two prominent draining branches. The measurement of the peak systolic velocity of 600 cm/s at the venous out flow adjacent to the anastomosis identified a stenosis. The flow rate was measured at 1000 ml/min. Due to these diagnostic findings we initiated a percutaneous intervention.
We chose a retrograde access to the cephalic vein. Catheteter angiography confirmed the ultrasound test results (Figure 1). Out flow of the cephalic vein was through basilic vein, cephalic vein of the upper arm and deep venous system in the cubital fossa via drainage through the perforating vein (Figure 2). We performed a balloon angioplasty of the arteriovenous fistula with a plain balloon (4 mm) at the end of the procedure.

Figure 1: Retrograde access to the cephalic vein of the forearm showing the stenosis of the anastomosis and the two draining branches.
After explaining the results of the angiography to our patient, we decided to perform a long-segment autologous patch angioplasty. We used the radial located venous branch as an autologous transplant. We ligated the second venous branch and the perforating vein additionally. Finally, the cephalic vein was transposed. The transit time ultrasonic flow measurement performed after suturing the patch revealed a flow rate of 140 ml/min. We identified reduced arterial inflow because of venous stenosis near the arteriovenous anastomosis. For this reason, the anastomosis was created more proximally. Characteristic post thrombotic lesions of the vascular wall have caused the stenosis. At the end of the procedure the measured flow rate was still unsatisfactory at 190 ml/min. The operation was finished, and it was decided to observe the fistula to determine whether reduced flow rate was caused by vasospasm.
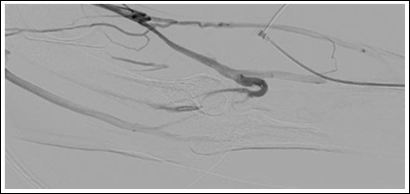
Figure 2: Angiogram showing the perforating vein (à).
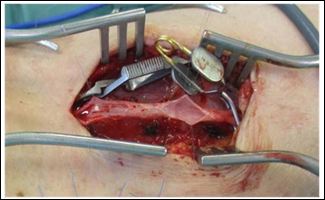
Figure 3: Trabecular, post thrombotic lesions of the cephalic vein of the upper arm.
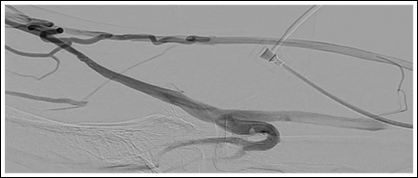
Figure 4: Stenosed segment of the cephalic vein of the upper arm (}).
We examined the angiography again and identified a stenosed segment of the cephalic vein at the distal upper arm. Regarding to the missing well-developed collaterals maintaining venous out flow before the fistula was at risk for occlusion. Hence, we performed surgical revision of the stenosis using an interposition graft (PTFE 6 mm). This segment showed post thrombotic lesions as well with trabecular morphology. The flow rate measured 550 ml/min and there was continuous thrill in the fistula. The temperature of the hand was warm, and pulses were palpable at the wrist.
The patient was discharged on the sixth postoperative day with a primarily healing wound. After six months the AVF matured well with flow rate of 1000 ml/min and without needle access problems.
Discussion
To provide adequate maturation an arteriovenous fistula needs an inflow, peripheral out flow and central venous out flow [4]. Considering the main aspects of what a functional AVF needs to get needle access conduit, we do not really recognize peripheral out flow failure.
Catheter angiography shows vascular anatomy of the fistula with out flow obstruction at the upper arm cephalicvein (Figure 3) and well-developed collaterals (Figures 1 and 4). Troubleshooting was not such as adequate as we did appreciate preexisting problems in this case. Figure 1 demonstrates primary flow is drained through the collateral in the basilic system. Figure 2 shows inadequate drainage into the deep venous system through elbow perforator with lesions in upper arm cephalic vein and non-visualization of median cubital vein.
References
- Abreo K, Amin BM, Abreo AP (2019) Physical examination of the hemodialysis arteriovenous fistula to detect early dysfunction. J Vasc Access 20: 7-11.
- Murphy EA, Ross RA, Jones RG, Gandy SJ, Aristokleous N, et al. (2017) Imaging in vascular Cardiovasc Eng Technol 8: 255- 272.
- MacRae JM, Ahmed A, Johnson N, Levin A, Kiaii M (2005) Cen- tral vein stenosis: A common problem in patients on hemodialysis. ASAIO J 51: 77-81.
- MacRae JM, Dipchand C, Oliver M, Moist L, Lok C, et (2016) Ar- teriovenous access failure, stenosis, and thrombosis. Can J Kidney Health Dis 3.
Citation: Süss JD, Fürste K, Gawenda M (2020) Misunderstood Outflow Pattern of the Outflow Vein Risks AV Fistula (AVF) Occlusion. J Cardio Cardiovasu Med 4: 012.
Copyright: © 2020 Süss JD, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.


