*Corresponding Author:
Eustaquio Maria Onorato,
Centro Cardiologico Monzino, IRCCS, University of Milan, Italy
Tel: +39 3486939883
E-mail: eustaquio.onorato@gmail.com
Abstract
Heart Failure with preserved Ejection Fraction (HFpEF) may be a challenging diagnosis and has a limited medical treatment available. We describe a case of HFpEF requiring diastolic stress assessment as confirmatory test and creation of a restrictive interatrial communication as palliative therapy.
Keywords
Atrial septostomy; Heart failure with preserved ejection fraction; Left atrial decompression; Treatment
Introduction
Current evidence for interatrial shunting is based on observational studies and small randomized trials showing the feasibility, safety and preliminary efficacy in patients with Pulmonary Arterial Hypertension (PAH) and Heart Failure (HF). These data seem to be insufficient to modify current clinical practice but support the use of interatrial shunting as a palliative therapy in selected patients with left HF who remain symptomatic despite optimal treatment based on current guidelines. Several ongoing randomized trials will provide definite evidence about the exact role of this strategy for the treatment of HF patients.
Case Report
A 71-year-old woman presented with 3 months of progressive dyspnea on exertion and volume overload. The patient’s medical history was notable for long-standing arterial hypertension and permanent atrial fibrillation. Her earliest Trans-Thoracic Echocardiogram (TTE) 1 year previously showed biatrial enlargement, normal Left Ventricular (LV) function with moderate concentric hypertrophy, moderate mitral regurgitation, normal right ventricular function, and mild tricuspid regurgitation with a peak regurgitant velocity of 3.1 m/s. She was under beta-blockers (bisoprolol 2.5 mg/day), ACE inhibitors, apixaban and furosemide (25 mg). ECG showed atrial fibrillation with an average heart rate of 85 bpm and diffuse ST segment abnormalities. Laboratory test results showed increased brain natriuretic peptide (BNP 452 pg/ml). The six-minute walking test (6MWT) distance was 380 m (Table 1). TTE demonstrated preserved LV Ejection Fraction (LVEF), moderate mitral regurgitation (Supplementary Movie 1 A) and mild tricuspid regurgitation with an estimated pulmonary pressure of 50 mmHg. There was a rightward systolic displacement of the atrial septum, while E/e’ ratio was 11.2 indicating increased LV filling pressure. The patient underwent cardiac catheterization which demonstrated postcapillary pulmonary hypertension with a prominent V-wave in the pulmonary wedge pressure tracing. Coronary arteries were normal. Mitral regurgitation was moderate on LV angiography while LVEF (65%). She was discharged home with a therapy including spironolactone and increased furosemide (75 mg/ day) and beta-blockers (bisoprolol 5 mg/day). No clinical benefit was reported at 3 months. To assess the relative role of mitral regurgitation and diastolic dysfunction the patient underwent a simultaneous invasive and non-invasive diastolic stress test. Pulmonary Capillary Wedge Pressure (PCWP) increased from 15 to 25 mmHg whereas mitral regurgitation became trivial at peak exercise.
The patient gave informed consent to undergo restrictive atrial septostomy. Using real-time Transesophageal Echocardiographic (TEE) guidance, the inter-atrial septum was crossed through a patent foramen oval with a multipurpose catheter. A balloon-based atrial septostomy was performed with a 14-mm non-compliant over-thewire balloon (Figure 1), the balloon diameter being 6 mm larger than the planned fenestration diameter of the Atrial Flow Regulator (AFR) device (8 mm).
The Atrial Flow Regulator (AFR) device (Occlutech, Helsingborg, Sweden) (Figures 2A and 2B, Supplementary Table 1) with an 8-mm fenestration, 5-mm height and 21-mm discs diameter was implanted into the interatrial septum (Figure 3). Postoperative TEE showed left-to-right interatrial shunting through the device (Figure 4), significantly reduced mitral annular area and trivial residual mitral regurgitation (Figure 5). Post-procedural right heart catheterization demonstrated a drop in PCWP (12 mmHg), an increase in RA and a 1.2 QP/QS ratio (Table 1). At 3-months follow-up the patient was asymptomatic (NYHA I), BNP decreased to 380 ng/L and the 6MWT distance increased to 470 m. TTE showed AFR patency, mild mitral regurgitation (Figure 6, Supplementary Movie 1, B), moderate tricuspid regurgitation with mildly enlarged but normally functioning right ventricle.
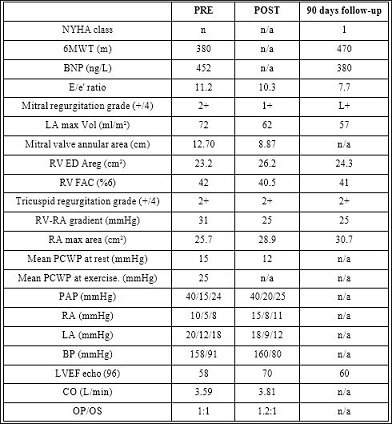
Table 1: Clinical and hemodynamic characteristics.
Note: 6MWT: 6-Miniutes Walking Distance; BNP: Brain Natriuretic Peptide; CO: Cardiac Output; ED: End-Diastolic; FAC: Fractional Area Change; LA: Left Atrium; LVEF: Left Ventricular Ejection Fraction; NYHA: New York Heart Association; PAP: Pulmonary Artery Pressure; PCWP: Pulmonary capillary wedge pressure; QP/QS: Pul- monary/Systemic flow ratio; RV: Right ventricle; Vol: Volume; RA: Right Atrium.
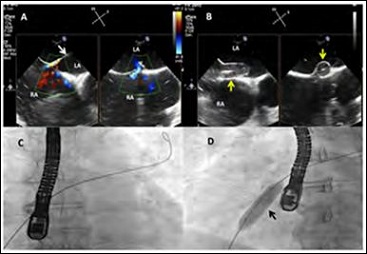
Figure 1: A) Two-dimensional color Doppler Transesophageal Echocardiography (TEE) biplanar view showing the guide wire (white arrow) crossing a patent foramen ovale; B) Dilatation of the atrial septum with a noncompliant balloon (yellow arrow); C) Fluoroscopic image of the guide wire placed into the upper left pulmonary vein; D) Inflated over-the-wire balloon (black arrow).
Note: RA: Right Atrium; LA: Left Atrium
Discussion
Heart Failure with preserved Ejection Fraction (HFpEF) is a frequent disease with limited medical treatment available [1]. Studies have shown that the pathophysiological hallmark of this condition is elevated left atrial pressure while exertional dyspnea is its main clinical manifestation [2,3]. In our patient PCWP was increased both at rest and during stress test providing “definite” diagnosis of HFpEF. However, the presence of secondary mitral regurgitation was a confounding factor. In fact, an increase in the degree of MR during exercise may have been the main factor determining an increase in PCWP and could have deserved surgical correction. Simultaneous invasive and non-invasive diastolic stress test excluded this condition, because PWCP increased and MR decreased during exercise. Optimal medical therapy for HFpEF comprises diuretics, beta-blockers, mineral receptor antagonists, renin-angiotensin-aldosterone system inhibitors, while use of Sacubitril/Valsartan in HFpEF is still a controversial option. In our patient symptoms persisted although medical therapy had been optimized.

Figure 2: A) The Occlutech AFR is a self-expandable double-disc wire mesh device constructed from nitinol braided into two flat discs connected by a waist without fabric inside; a central fenestration enables bidirectional flow. A welded ball connector located on the device’s proximal disc serves as an adapter to connect the delivery system (Flex II Pusher) for deployment. The device is easy to handle, self-centers following deployment, and is retrievable prior to release. B) Hemodynamic and echocardiographic measurements with sizing instructions. The Atrial Flow Regulator (AFR) device is available in 8 mm and 10 mm fenestration diameter and in 5 mm and 10 mm height.
Note: PCWP: Pulmonary Capillary Wedge Pressure
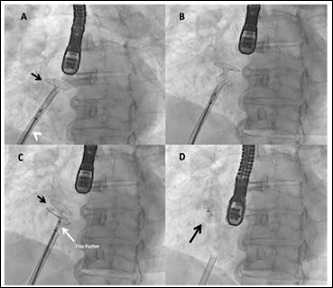
Figure 3: Procedural steps of the Atrial Flow Regulator device implantation. A) opening of the distal disc (black arrow) while the delivery system (arrowhead) is pulled back ensuring back tenting at the level of interatrial septum; B) opening of the waist and proximal disc; C) Fully opening of the device (black arrow) with persistent anchoring to Flex Pusher (white arrow); D) Final deployment of the device (black arrow).
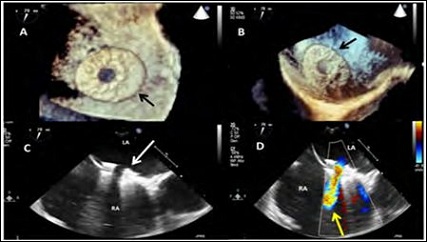
Figure 4: A-B: 3D TEE enface views showing the implanted AFR device (black arrow). C-D: TEE two-dimensional color Doppler showing the fenestrated device (white arrow) embedded in the atrial septum and the device patency with a left-to-right shunting (yellow arrow).
Note: RA: Right Atrium; LA: Left Atrium.
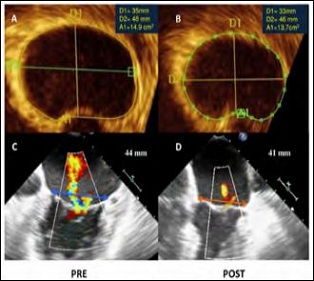
Figure 5: Pre and Postoperatively 3D TEE (A-B) measurement of dimensions and area of the mitral anulus and 2-D color-Doppler (C-D) assessment of mitral regurgitation.
Note: Blue line: pre-procedure mitral annulus dimension; Orange line: post-procedure mitral anulus dimension
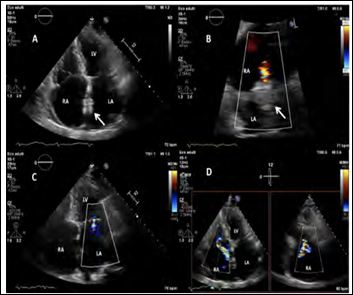
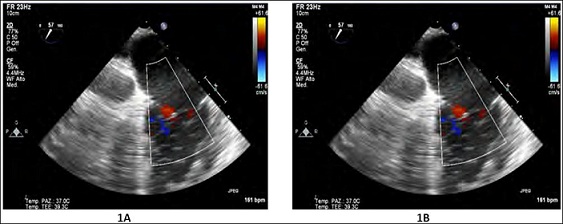
Figure 6: TTE at 3-month-follow-up. The apical four-chambers A) and subcostal B) views confirm the stable position of the device (white arrow) with persisting left-toright shunt. The apical four-chamber C) and biplanar D) views demonstrate mild mitral and moderate tricuspid regurgitation.
Note: RA: Right Atrium; LA: Left Atrium; LV: Left Ventricle
Left atrial decompression by means of the creation of unidirectional but restrictive left-to-right interatrial shunt has recently been emerging as a new therapeutic strategy in patients suffering from both HFpEF and HFrEF [4]. Three dedicated devices (interatrial septal device system-IASD, V-Wave and AFR) are currently available [5-7]. Several clinical studies have demonstrated the safety of this approach, with encouraging results in terms of hemodynamic parameters improvement.
The AFR , CE marked in 2019, is a self-expanding double-disc wire mesh device constructed from nitinol braided into two flat discs with a central fenestration which enables bidirectional flow [Supplementary Move 1], providing an innovative, minimally invasive treatment alternative to address the significant unmet medical needs in HF patients.
The AFR device differs from the competing devices mostly because it is made of nitinol mesh without fabric and the interatrial communication is larger than the V-Wave (5mm) and equal or larger compared to the IASD [8mm]. Sizing of AFR device is based on LA pressure and atrial septum thickness (Figure 2B).
In our patient variations in surrogate parameters seen 3-month after the procedure are consistent with those observed in published studies: NYHA class decrease from II to I, BNP decreased by 3.9% [mean 2,8% pro BNP decrease (p=0.25)] was observed in patients with HFpEF in the AFR PRELIEVE trial [7], and the 6MWT distance increased by 29% [mean 17% 6MWT distance increase (p=0.01)] was observed in a single-arm open-label study using the V-wave system in patients with both HFrEF and HFpEF) [6]. In our case a marked reduction in mitral annular area was documented after AFR implantation as a likely consequence of reduction in LA volume. This may determine a reduction in MR severity triggering an hemodynamic virtuous circle.
Conclusion
HFpEF is a frequent condition with a diagnosis that is often difficult and limited therapeutic armamentarium. Left atrial decompression through restrictive septostomy represents a novel option for patients with HFpEF who remained symptomatic despite optimal medical therapy.
Acknowledgments
The authors express their appreciation to Antonio Iavernaro, MD, Staff Member of the Cath Lab of UOC Cardiologia, Ospedale di Bassano del Grappa, Azienda Sanitaria ULSS 7 Pedemontana, Bassano del Grappa, Italy.
The authors also thank the engineering and marketing staff at Occlutech for technical descriptions of the device and for illustrations.
Conflict of Interest
Eustaquio Maria Onorato is a consultant for Occlutech, manufacturer of the device. The remaining Authors declare no confict of interest relevant to this publication.
References
- Borlaug BA, Paulus WJ (2011) Heart failure with preserved ejection fraction: pathophysiology, diagnosis, and Eur Heart J 32: 670-679.
- Dorfs S, Zeh W, Hochholzer W, Jander N, Kienzle RP, et (2014) Pulmonary capillary wedge pressure during exercise and long-term mortality in patients with suspected heart failure with preserved ejection fraction. Eur Heart J 35: 3103-3112.
- Wolsk E, Kaye D, Borlaug BA, Burkhoff D, Kitzman DW, et (2017) Resting and exercise hemodynamics in relation to 6-minute walk test in patients with heart failure and preserved ejection fraction. Eur J Heart Fail 20: 715-722.
- Burkhoff D, Maurer MS, Joseph SM, Rogers JG, Birati EY, et al. (2015) Left atrial decompression pump for severe heart failure with preserved ejection fraction: Theoretical and clinical ACC Heart Fail 3: 275-282.
- Feldman T, Mauri L, Kahwash R, Litwin S, Ricciardi MJ, et al. (2018) Transcatheter interatrial shunt device for the treatment of heart failure with preserved ejection fraction (REDUCE LAP-HF I [Reduce Elevated Left Atrial Pressure in Patients with Heart Failure]): A phase 2, randomized, Sham-controlled Circulation 137: 364-375.
- Rodes-Cabau J, Bernier M, Amat-Santos IJ, Ben Gal T, Nombela-Franco L, et (2018) Interatrial shunting for heart failure: Early and late results from the first-in-human experience with the V-wave system. JACC Cardiovasc Interv 11: 2300-2310.
- Paitazoglou C, Ozdemir R, Pfister R, Bergmann MW, Bartunek J, et (2019) The AFR-PRELIEVE trial: A prospective, non-randomised, pilot study to assess the Atrial Flow Regulator (AFR) in heart failure patients with either preserved or reduced ejection fraction. EuroIntervention 15: 403-410.
Supplementary Information
Supplementary Movie 1: Two-dimensional color Doppler Transthoracic Echocardiography (TTE) apical four-chambers views. The moderate mitral regurgitation at baseline (A) became mild at three months postoperatively (B).
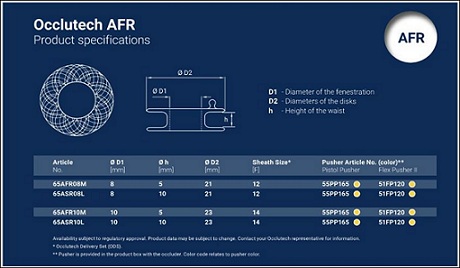
Supplementary Table 1: Product specifications Occlutech Atrial Flow Regulator (AFR) device.
The device is available in 8-mm and 10-mm fenestration diameters and two waist heights (5-mm and 10-mm) to suit the atrial septal thickness with a total device diameter of 21 and 23 mm, respectively, delivered via 12-F and 14-F sheath. Dedicated delivery systems (Pistol Pusher, Flex II Pusher) for deployment are listed.
Citation: Chirillo F, Cucchini U, Carasi M, Zadro M, Onorato EM (2020) Left Atrial Decompression as Palliative Therapy for Heart Failure Patients with Preserved Ejection Fraction. J Cardio Cardiovasu Med 4: 017.
Copyright: © 2020 Chirillo F, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.


