*Corresponding Author:
Mariem Jabeur,
Department of Cardiology, Grenoble Alpes University, Grenoble, France
Tel: +33 476766823
E-mail: Mariemjabeur2@gmail.com
Abstract
A 78-year-old female with prior Orthotopic Heart Transplant (OHT) underwent a percutaneous Left Atrial Appendage (LAA) occlusion using a WATCHMAN device. The procedure was technically challenging due to anatomical changes following biatrial anastomosis. We describe in this article the different stages of the procedure. This case demonstrates the feasibility of LAA occlusion using WATCHMAN device in OHT.
Keywords
Left atrial appendage occlusion; Orthotopic heart transplantation; Watchman device
Abbreviations
AF: Atrial Fibrillation
LAA: Left Atrial Appendage
OHT: Orthotopic Heart Transplant
TEE: Transesophageal Echocardiography
TTE: Transthoracic Echocardiography
Introduction
Percutaneous Left Atrial Appendage (LAA) closure using a WATCHMAN device has been shown to be an effective alternative therapy to warfarin for stroke prevention in patients with non-valvular atrial fibrillation [1,2].
Biatrial anastomosis Orthotopic Heart Transplant (OHT) is associated with development of atrial arrhythmias, including atrial fibrillation and flutter [3]. This type of anastomosis also creates large atria, scar tissue in the interatrial septum from surgical manipulations, and usually leaves the heart rotated leftward in the chest [4].These changes can complicate percutaneous LAA occlusion.
Case Report
A 78-year-old active woman had undergone orthotopic heart transplantation in 2008. She developed paroxysmal Atrial Fibrillation (AF) six years after transplantation and was started on oral anticoagulation. Two years later, oral anticoagulant therapy was stopped due to repeated severe arm hematomas, despite her high thromboembolic risk. Following a multidisciplinary team evaluation, LAA occlusion was therefore indicated. Cardiac tomography assessment revealed a chicken wing LAA (Figure 1, Panel B), measurements were 40*29mm.
LAA orifice diameter was 30mm and the depth was 40mm on Transesophageal Echocardiography (TEE) (Figure 1, Panel A). Despite of anatomical changes post biatrial anastomosis OHT, the standard WATCHMAN TEE implantation views were adequate (Figure 1, Panel A). A BRK© transseptal needle with an accentuated 30°curve was used to puncture the interatrial septum. A 33mm plug was successfully delivered to the LAA on the first attempt (Figure 1, Panels D and E). The patient was discharged on Clopidogrel and Aspirin therapy.
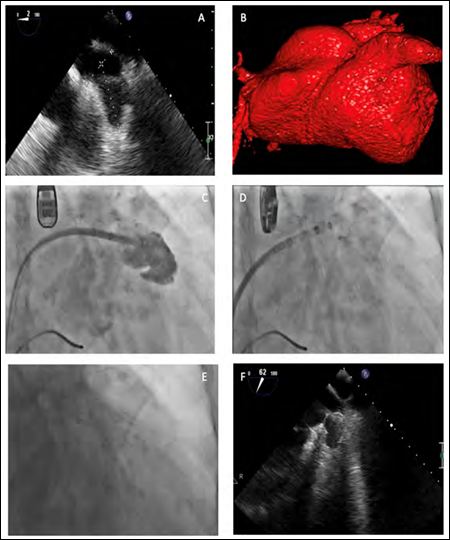
Figure 1: A) Transesophageal Echocardiography (TEE) view of the Left Atrial Appendage (LAA) ostium maximum diameter (30mm). B) Tomography reconstruction of the LAA. C) LAA opacification. D and E) Fluoroscopic view of a 33mm Watchman device successful deployment. F) Good device position after deployment on TEE.
A TEE at 30 days demonstrated no thrombus and no residual flow in the LAA. Clopidogrel was discontinued after one month and the patient wasplaced on Aspirin in long term. After a 6 months follow-up the patient is free from bleeding and cardioembolic events.
A transthoracic Echocardiography (TTE) at 6 months revealed no peri device leak.
Discussion
LAA occlusion is currently recommendedfor patients with non-valvular atrial fibrillation at high risk of stroke and systemic embolism, and with a contraindication to oral anticoagulation [5]. For cases where LAA anatomy is not suitable for endocardial occlusion, alternative epicardial approaches such as the Lariat suture device or surgical ligation can be considered [6]. The Lariat device cannot be used for LAA width larger than 40mm, superiorly oriented LAA with the LAA apexdirected behind the pulmonary trunk, posteriorly rotated heart or inpatients with previous cardiac surgery [7]. Surgical ligation, althoughmore invasive, remains an alternative option for patients but isassociated with persistent necks, residual leaks and lacks randomizedcontrolled trial data demonstrating efficacy in stroke prevention [7].
Anatomical changes post biatrial anastomosis OHT can significantly complicate a WATCHMAN implant procedure. Due to morphological changes in atrial anatomy and leftward rotation of the heart in the chest, the standard WATCHMAN TEE implantation views (0, 45, 90, and 135°) [8] may not be adequate. In this case, TEE 0° view allowed for the desired LAA ostial view and ensured proper device sizing.
In addition, carrying out a safe site-specific transseptal puncture in the inferio-posterior location of the fossa ovalis necessary for WATCHMANdevice delivery in the transplanted heart can be challenging for the same reasons listed above [7]. The septum may be scarred and thickened making traditional transseptal needle puncture difficult. For this reason, using radiofrequency enhanced transseptal access can make access to the left atrium simpler and safer. Reshaping the transseptal needle to accentuate the curve may be required for adequate septal tenting given the dilated right atrium [7]. Occasionally, balloon dilation of the previously manipulated septum may be necessary to allow the LAA occlusion delivery sheath to be advanced into the LAA [7].
In this case, a BRK© transseptal needle with an accentuated 30° curve was used to cross the septum in the desired location, without any complication. No radiofrequency needle and no balloon dilation of the septum were required.
Conclusion
This case demonstrates that LAA occlusion using a WATCHMAN device in a patient with prior OHT is feasible. This procedure should be proposed if indicated to patients with heart transplant.
References
- Majule DN, Jing C, Rutahoile WM, Shonyela FS (2018) The efficacy and safety of the watchman device in laa occlusion in patients with non-valvular atrial fibrillation contraindicated to oral anticoagulation: A focused Ann Thorac Cardiovasc Surg 24: 271-278.
- Reddy VY, Doshi SK, Kar S, Gibson DN, Price MJ, et al. (2017) 5-Year Outcomes after left atrial appendage closure: From the PRE- VAIL and PROTECT AF J Am Coll Cardiol. 70: 2964-2975.
- Thajudeen A, Stecker EC, Shehata M, Patel J, Wang X, et (2012) Arrhythmias after heart transplantation: Mechanisms and manage- ment. J Am Heart Assoc.
- Dell’Aquila AM, Mastrobuoni S, Bastarrika G, Praschker BL, Agüero PA, et al. (2012) Bicaval versus standard technique in orthotopic heart transplant: Assessment of atrial performance at magnetic res- onance and transthoracic echocardiography. Interact Cardiovasc Thorac Surg 14: 457-462.
- Hindricks G, Potpara T, Dagres N, Arbelo E, Bax JJ, et al. (2021) 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J 42: 373-498.
- Lakkireddy D, Afzal MR, Lee RJ, Nagaraj H, Tschopp D, et al. (2016) Short and long-term outcomes of percutaneous left atrial ap- pendage suture ligation: Results from a US multicenter evaluation. Heart Rhythm 13: 1030-1036.
- Poulin M-F, Mohamedali B, Kavinsky CJ, Krishnan K (2019) Left atrial appendage occlusion using a Watchman device in a trans- planted heart with biatrial anastomosis. Catheter Cardiovasc Interv 93: 758-760.
- Wunderlich NC, Beigel R, Swaans MJ, Ho SY, Siegel RJ (2015) Percutaneous interventions for left atrial appendage exclusion: Op- tions, assessment, and imaging using 2d and 3d JACC Cardiovasc Imaging 8: 472-488.
Citation: Jabeur M, Jacon P, Defaye P (2021) Left Atrial Appendage Occlusion in an Orthotopic Transplanted Heart: A Case Report. J Cardio Cardiovasc Med 5: 021.
Copyright: © 2021 Jabeur M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.


