*Corresponding Author:
Rima Chaddad,
Department of Cardiology, Lebanese University, Beirut, Lebanon
E-mail: rimach.9991@hotmail.com
Abstract
Intermittent Left Bundle Branch Block (LBBB) has been reported in the literature following certain conditions such as cardiac blunt trauma, Myocardial Infarction (MI) or exercise induced LBBB. In the majority of cases, the patients usually have underlying coronary artery disease. We describe a case of patient who presented with intermittent LBBB associated with chest pain, and subsequently the patient was taken to the catheterization laboratory for emergency coronary angiogram, which revealed 50% non obstructive atherosclerotic plaque of the mid- LAD .
Keywords
Chest pain; Intermittent left bundle branch block; Non obstructive coronary artery disease
Introduction
LBBB is often a marker of Coronary Artery Disease (CAD), hypertensive heart disease, aortic valve disease, and cardiomyopathy.
Intermittent left bundle branch block is an uncommon conduction disturbance. Patients with intermittent Left Bundle Branch Block (LBBB) have periods of conduction with LBBB and periods of conduction without LBBB [1].
Over time, these patients are at increased risk for development of permanent BBB, CAD, cardiomyopathy, and CHD-related as well as all-cause mortality.
We report a case of intermittent LBBB who posed diagnostic dilemma and difficulties in decision making. Chest pain syndrome associated with intermittent left bundle branch block (LBBB) in the absence of myocardial ischemia has been described as “painful LBBB syndrome” [2].
The proposed mechanisms include dyssynchronous systolic motion of the septum and generalized interoceptive sensitivity [3].
Treatment options, which include submaximal exercise regimens, β-blockers, and Right Ventricular (RV) and biventricular pacing, have yielded only modest success. Permanent His Bundle Pacing (HBP) has shown decreased rates of heart failure compared to traditional RV pacing as well as reversal of dyssynchrony-induced cardiomyopathy.
Case Presentation
A 58 year old male patient with relevant family history of premature CAD (his brother underwent CABG at the age of 40 years old), presented for elective knee arthroscopy. He is smoker (15 pack/y), has no history of alcohol intake and no illicit drug use. Physical exam and cardiac auscultation were normal. Preoperative ECG showed a regular sinus rhythm with T wave inversion in the precordial leads (V1-V4) (Figure 1).
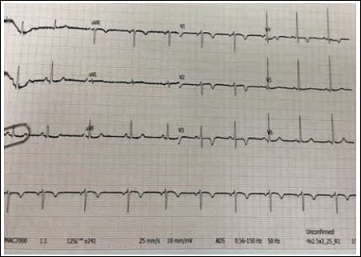
Figure 1: Preoperative electrocardiogram revealing normal sinus rhythm with anteroseptal T wave inversion.
Day zero post operation, patient suddenly had chest pain. He described the pain as severe retrosternal, radiating to the left arm associated with severe diaphoresis and shortness of breath. On physical examination, he was hemodynamically stable, blood pressure of 115/52 mmHg, pulse of 78 bpm, with normal saturation on room air.
ECG was immediately obtained, it consistently showed (LBBB) during chest pain episode (Figure 2). Patient was started on aspirin 325 mg, loading dose of Ticagrelor 180 mg, heparin drip, and was subsequently taken for emergent coronary angiogram. The coronary angiogram showed a 50% non obstructive atherosclerotic plaque of the mid-LAD (Figure 3), calculated using Quantitative Coronary Angiography (QCA). A trial of intracoronary nitroglycerin fails to relieve the stenosis as well as the chest pain, which may argues against vasospastic mechanism of his pain .The lack of availability of IVUS or FFR in the catheterization laboratory is a limitation step. A high sensitivity cardiac troponin value turned negative for 2 sets. Echocardiogram showed normal left ventricular ejection fraction without any regional wall motion abnormalities.
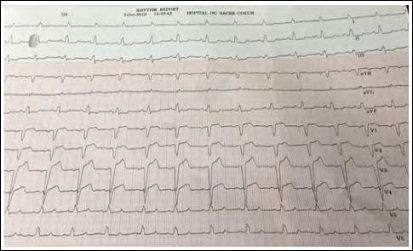
Figure 2: Electrocardiogram during the episode of chest pain revealing complete LBBB with a HR of 78 bpm.
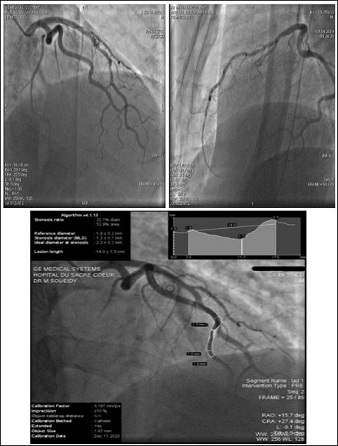
Figure 3: Coronarography showed the non obstructive coronary plaque of the mid LAD. (4a-RAO CRA viex/4b-LAO CAU view) using the QCA showed a 53% stenosis ratio.
The diagnosis of painful LBBB was made and the patient was started on medical treatment, which provided symptomatic relief.
Repeated ECG before discharge, showed precordial T wave inversion same as preoperative ECG, called “cardiac memory”. The follow up ECGs after 1, 3 and 6 months showed persistent LBBB with complete resolution of pain (Figure 4). There are several possible mechanisms for this rare occurrence. First, it could be that the patient did indeed have undiagnosed CAD. However, the absence of significant stenosis and laboratory tests suggestive of ischemia argue against this possibility .Second option may be rate related BBB, but the difference of rate pre and post operation (65 vs 78 bpm) is non significant and no evidence of intraoperative tachycardia or HTN. Another possibility is drug related, may be due to anesthesia and this option can’t be excluded.
Discussion
LBBB occurs when normal conduction through the HisPurkinje system is disturbed due to slowing of anterograde conduction or retrograde invasion of the left bundle, leading to prolongation of ventricular depolarization and widening of the QRS complex. The etiology of this entity is multifold and includes structural heart disease, abberant conduction in the absence of structural heart disease, and electrolyte abnormalities. The phenomenon of Cardiac memory has been observed since 1940s [4]. Cardiac memory is seen in association with Intermittent left bundle branch block.
Intermittent LBBB was reported in the literature. Most of the time, it presents in patients with underlying coronary arteries disease, and rarely described in patients with normal coronary vasculatures [5].
Many cases of intermittent LBBB are discussed in the literature, the possible causes are:
- Rate dependent LBBB, and the mechanisms are attributed to phase 3 and 4 block and concealed conduction
- Transient LBBB in acute pulmonary embolism may be induced by slower rate which can slow conduction along the right bundle
- LBBB during cardiac interventions such as TAVI or Watchman device and attributed to injury of the short LBBB trunk
- Transient LBBB after Mad Honey poisoning may be caused by tachycardia , bradycardia or hypotension
- Drug –induced episodic LBBB , such as propafenone or flecainide
- Transient LBBB in acute pancreatitis with unclear mechanism
- LBBB due to changes of intrathoracic pressure triggered by laughter
Vieweg et al. [6] were first reported intermittent LBBB in patients with normal coronary arteries.
This case is unique and rare in the literature, we report an acute coronary syndrome associated with intermittent LBBB and non obstructive coronary artery disease. Most of the time, coronary angiogram is needed to rule out coronary artery disease. The conversion from intermittent to permanent LBBB that results in resolution of pain [7], argue against ischemia as well. Dyssynchronous ventricular contraction is described as the possible cause of pain [8].
This is a complex case of intermittent LBBB in a patient presenting with suspicion of acute coronary syndrome after knee arthroscopy, with non obstructive coronaries. Painful episode of LBBB occurred just after receiving locoregional anesthesia that may be the trigger and also a rare phenomenon.
Our patient started on medical treatment with beta blocker and statin with a clinical follow up and ECG at 1, 6 months, which demonstrate a complete resolution of his symptoms with a permanent LBBB on his surface ECG.
Conclusion
Intermittent LBBB was reported in the literature, in patients with underlying coronary arteries disease, and rarely described in patients with normal coronary vasculatures. This case is rare in the literature, we report an intermittent painful LBBB with non obstructive coronary artery disease that occurs post operation and resolved when the patient is free of symptoms.
This can raise the question: Does every new LBBB associated with chest pain, is indicative of obstructive coronary artery disease? And what are the trigger and the exact mechanism behind this rare phenomenon? And what are the options of treatment?
References
- Neeland IJ, Kontos MC, de Lemos JA (2012) Evolving considerations in the management of patients with left bundle branch block and suspected myocardial infarction. J Am Coll Cardiol 60: 96-105.
- Loubeyre C (1991) Le bloc de branche gauche douloureux d’effort. Ann Cardiol Angeiol (Paris) 40: 613-617.
- Virtanen KS, Heikkilä J, Siltanen P (1982) Chest pain and rate-dependent left bundle branch block in patients with normal coronary Chest 81: 326-331.
- Campbell M (1942) Inversion of T waves after long paroxysms of Br Heart J 4: 49-56.
- Kumar V, Venkataraman R, Aljaroudi W, Osorio J, Heo J, et al. (2013) Implications of left bundle branch block in patient treatment. Am J Cardiol 111: 291-300.
- Vieweg WV, Stanton KC, Alpertet JS, Hagan AD (1976) Rate-dependent left bundle branch block with angina pectoris and normal coronary Chest 69: 123-124.
- Bory M, karila P, Sainsous J, Cohen SB, Djiane P, et al. (1985) Apparition simultanee de precordialgie et d’un bloc de branche gauche a l’effort. Etude chez 6 patients avec coronarographie normale. Arch Mal Cœur Vaiss 78: 1326-1331.
- Perin E, Petersen F, Massumi A (1991) Rate-related left bundle branch block as a cause of non-ischemic chest pain. Cathet Cardiovasc Diagn 22: 45-46.
Citation: Chaddad R, Soueidy M (2020) Intermittent Left Bundle Branch Block - A Challenging Case. J Cardio Cardiovasc Med 4: 020
Copyright: © 2020 Chaddad R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.


