*Corresponding Author:
Ruchit Patel,
Department of cardiothoracic and vascular surgery, Post Graduate Institute of Medical Education & Research, Chandigarh, India
Tel: + 91 8872260595
E-mail: ruchitmbbs@gmail.com
Abstract
Though coronary artery anomalies are frequent in dTGA, high origin coronaries are rarely observed. Patient with high origin coronaries are more prone to coronaryinjury during coronary button transfer in arterial switch operation with immediate and late postoperative presentation. So coronary anatomy should be preoperatively elicited with appropriate imaging and injury can be avoided with proper planning. We described a case of dTGA with high coronaries successful surgical management.
Keywords
Arterial switch operation; Dextro transposition of great arteries; High origin of coronary arteries
Abbreviations
TGA- Transposition of Great Arteries
ASO- Arterial Switch Operation
TEE- Transesophageal Echocardiography
RCA- Right Coronary Artery
LCA- Left Coronary Artery
VSD- Ventricular Septal Defect
Introduction
Transfer of the coronaries has been a concern in performing Arterial Switch Operation (ASO). Though Jatene and colleagues overcame this issue in 1975, during early era of ASO, the early and midterm outcomes of the procedures were undesirably affected by coronary complications [1]. Over the years, development of techniques of coronary transfer with certain modifications has substantially improved mortality and morbidity rates lower than 3% [2].
Coronary anomalies are frequently present in cases of TGA (Transposition of great arteries) [3], but high origin of coronaries is rarely observed. In children with anomalous coronary anatomy, risk of early and late coronary complications are almost twice that of those with usual coronaries [4]. Various studies have shown coronary patterns like “inverted” coronaries, single (or mixed common trunk) and intramural coronaries to be significant risk factors for perioperative as well as late complications [5,6].
Here, we present a case of a 4 months old child with d-TGAwithhigh origin of coronary arteries that underwent successful arterial switch operation in our institute.
Case Summary
A four months old baby referred to our departmentwith diagnosis of d-TGA for corrective surgery. Child had mild cyanosis with predominantly failure symptoms. Pansystolic murmur was heard over precordium.
Preoperative trans-thoracic echo revealed d-TGA with large subpulmonic VSD and small OS-ASD. Additional basal muscular VSD was seen. Child was taken up for ASO. After induction of anaesthesia as per institutional protocols, Transesophageal Echocardiography (TEE) was done using a Philips S8-3t transesophageal probe and iE33 workstation. On mid-esophageal aortic valve short axis view at an omniplane angle of 60°, pulmonary artery was posterior and to the right. Aorta was anterior and left. The right coronary artery was coursing from the right coronary sinus towards the right ventricle without any branching (Figure1). Left coronary artery was coursing to itsbifurcation at an omniplane angle of around 20°, indicating the two coronaries were not in the same plane (Figure 2).
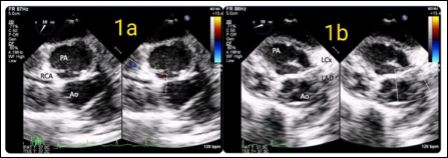
Figure 1: Transesophageal mid-esophageal short axis view showing right and posteriorly places Pulmonary Arteries (PA), left and anteriorly placed Aorta (Ao) and the Right Coronary Artery (RCA) originating from the right facing sinus.
The child underwent ASO under moderate hypothermic CPB. Aortic cannulation was high, at the base of innominate artery. Greater arteries were in side by side relation. Large subpulmonic was closed with PTFE patch and basal muscular VSD was closed directly with stitch. There was higher than usual origin of left coronary artery with two separate ostia for left and right coronary arteries. Proximal most portion of left coronary had intramural course, which was mobilized and slit opened. RCA button was separately excised. Neo PA was reconstructed using pericardial patch. After neoaorta anastomosis, aortic clamp was released transiently to see proper alignment and positions for both coronary buttons on neoaorta. Coronary buttons were reimplanted using modified closed transfer. Left coronary button was implanted above the anastomosis. Distal PA reconstruction was completed after Le Compte maneuver, shifting anterior to aorta. Post operative course was uneventful and child is doing well on follow up.
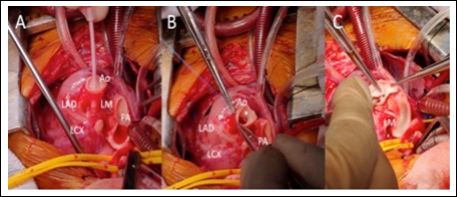
Figure 2: Transesophageal modified mid-esophageal short axis view showing the left coronary artery originating from the left facing sinus and dividing into to left Anterior Descending (LAD) and left Circumflex (LCx) arteries.
Discussion
Meticulous transfer of the coronary arteries is the most important technical aspect of the arterial switch procedure. For avoiding proximal tortuosity of coronary arteries, it is crucial to preserve the initial proximal patterns of the coronary arteries, which can lead to kinking and stenosis [1].
Coronary anomalies are associated with 30-35% cases with TGA, being more common when greater arteries are in side-by-side relation [3]. Most common coronary pattern is where circumflex arises from the RCA, contributing to fifty percent of unusual patterns. This anomaly associated with TGA has not been shown to imitate postoperative outcomes [4]. Those with most threatening types of coronary anomalies are existent in approximately 1-2% of TGA cases. Coronary arteries arising from a single ostium and those with intramural course carry a significant risk of death [5]. Highest mortality is seen with an intramural course of coronary, more than a 6-fold increase compared with the usual coronary arrangement (OR 6.5, 95% CI 2.9 to 14.2) in a study by Mettonet al [6].
Anatomical studies have variously defined a high take off of coronary arteries as an origin at or above the sinotubular junction. Para commissural origin has been defined as a distance of less than 20% the width of the sinus at the sinotubular junction between the commissure and the origin. In a case series of 277 TGA, incidence of high-take off, paracommissural or tangential take off of coronary arteries was around 20%, further adding to the potential complexity of ASO [3].
The current case had higher than usual origin of coronary arteries withantero-posterior relationship of great arteries. On intraoperative TEE, origins of both coronaries were not clearly demonstrated, leading to a suspicion of coronary anomalies. A high index of suspicion is necessary to decide on the need for additional preoperative imaging. The current guidelines recommend cardiac Computed Tomographic Angiography (CTA) or Cardiac MRI (CMRI) over coronary angiography. The combination of Dual Source Computed Tomography (DSCT) and TTE can provide a safe and effective imaging alternative modality for preoperative evaluation [7].
High origin coronaries have usually intramural course with likelihood of paracommisural ostia. By necessity, a coronary artery with an initial intramural course leaves the aorta with an abnormal acute angle, which increases the risk of kinking or stretching of the artery at the level of aortic take-off after coronary transfer. Implantation using a medially hinged trap-door usually solves the problem. Another is closed technique of coronary transfer, where implantation is done after aortic anastomosis to avoid kinking and mismatching. We also do posterior aortoplasty to allow matching size of vessels atneoaortic anastomosis. Aortic cannulation and level of transection should be higher than usual level.
Development of significant coronary stenosis in the early and late postoperative follow-up period of ASO stemmed from ostia fibrosis, intimal thickening, coronary artery stretching with growth, and kinking or reactive injuries during surgical manipulations [8]. Many asymptomatic obstructive stenosis cases have been reported which may also culminate into sudden adverse cardiac events later during follow-up.Early postoperative period, close observation for coronary complication should be considered, first before hospital discharge and, again, before school age. All patients with reimplanted coronaries are recommended to have a coronary angiography once in adulthood.If coronary lesions are suspected, myocardial perfusion imaging should be considered and re-operation should be undertaken if required.
Conclusion
Detailed preoperative imaging and meticulous coronary implantation techniques can avoid a significant coronary complication and mortality risks. Owing to the risk of early and late coronary complications, despite an uneventful initial postoperative course, all patients need to be followed up very closely.
References
- Jatene AD, Fontes VF, Paulista PP, Souza LC, Galantier M, et al. (1976) Anatomic correction of transposition of the great J ThoracCardiovascSurg 72: 364-370.
- Cain MT, Cao Y, Ghanayem NS, Simpson PM, Trapp K, et al. (2014) Transposition of the great arteries-outcomes and time interval of early neonatal repair. World J Pediatr Congenit Heart Surg 5: 241-247.
- Loukas M, Andall RG, Khan AZ, Patel K, Muresian H, et (2016) The clinical anatomy of high take-off coronary arteries. Clin Anat 29: 408-419.
- Pasquali SK, Hasselblad V, Li JS, Kong DF, Sanders SP (2002) Coronary artery pattern and outcome of arterial switch operation for transposition of the great arteries: A meta-analysis. Circulation 106: 2575-2580.
- Thrupp SF, Gentles TL, Kerr AR, Finucane K (2012) Arterial switch operation: Early and late outcome for intramural coronary Ann Thorac Surg 94: 2084-2090.
- Metton O, Calvaruso D, Gaudin R, Mussa S, Raisky O, et (2010) Intramural coronary arteries and outcome of neonatal arterial switch operation. European Journal of Cardio-thoracic Surgery 37: 1246-1253.
- Xie L-J, Jiang L, Yang Z-G, Shi K, Xu H-Y, et al. (2017) Assessment of transposition of the great arteries associated with multiple malformations using dual-source computed tomography. PLoS ONE 12.
- Tsuda T, Bhat AM, Robinson BW, Baffa JM, Radtke W (2015) Coronary artery problems late after arterial switch operation for transposition of the great arteries. Circ J 79: 2372-2379.
Citation: Mishra AK, Patel R, Upadhyay V, Bansal V, Neogi SG, et al. (2021) High Origin of Coronary Arteries in Transposition of Great Arteries. J Cardio Cardiovasc Med 5: 026.
Copyright: © 2021 Mishra AK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.


