*Corresponding Author:
Mohamed N Ibrahim,
Clínica Tres Torres, Barcelona, Spain
Email: felix.lugo@carmonadexeus.com
Abstract
Objective: In the past decades, suburethral sling operations have been the most common procedure for the treatment of female stress urinary incontinence (SUI). The objective of this study is to present the results of an alternative technique to the traditional operation based on transvaginal colpo-urhetropexy using autologous vaginal flaps, which has been performed in a series of 34 patients followed up to 20 years
Study Design: This was a retrospective study. The primary endpoint was the absence of urine leakage at 3, 6 and 12 months after sur- gery, as well as in routine annual controls thereafter by means of ob- jective clinical tests, such as the pad test, coughing test, Valsalva’s maneuver and anamnesis during the medical visit.
Result: Thirty-four patients were included in the study. All patients were clinically diagnosed of type II SUI, with preoperative urodynam- ic study in 6 cases. In 19 patients, SUI was associated to some type of genital prolapse or the sum of several pelvic floor alterations, the surgical repair of which was carried out at the time of the transvagi- nal colpo-urhetropexy procedure. None of the patients in this group had recurrent incontinence. Failures occurred in two cases: one pa- tient with morbid obesity and another patient who only experienced mild improvement of SUI after 12 months of surgery. The follow-up ranged between 1 and 19 years. There were no intraoperative or postoperative complications.
Conclusion: Transvaginal colpo-urhetropexy using autologous vag- inal flaps is a safe procedure with high effectiveness in the long-term and, therefore, may be considered a valid option in the treatment of SUI.
Keywords
Anamnesis; Surgery; Transvaginal colpo-urhetropex; Vaginal flaps; Valsalva’s maneuver
Introduction
Approximately 50% of women experience urinary incontinence at some time in their lives [1]. Urinary incontinence is a common disorder, and many women think that it is normal and they would not refer having symptoms of incontinence to the gynecologist, despite a negative impact on quality of life, sexual functioning and limitations on social activities. Anxiety, shame, embarrassment and frustration are also frequent, which can augment the feelings of low self-esteem and social isolation [2].
The efficacy of treatment of stress urinary incontinence (SUI) is based on a multidisciplinary approach with the patient, the gynaecologist and the physiotherapist forming a triad, which is indispensable for the coordination and planning of the therapeutic process [3]. It is necessary for the patient to acquire and strength certain habits that ultimately will help to improve the response to both pelvic floor rehabilitation exercises and the success of surgery [4].
In the last decades, suburethral sling procedures have been considered the gold standard operation in the management of SUI [5]. The two most common types of bladder slings are the TOT sling (transobturator tape sling) and the TVT sling (tension-free vaginal tape sling). In recent years, however, less invasive techniques including the single incision technique or mini-slings and adjustable mini-slings, have been introduced to reduce the risk of complications but maintaining the same cure rates than the TVT and TOT slings, but the cure rate is still lower [6].
In this respect, traditional surgical techniques have been displaced almost entirely by these new safe, standardized and reproducible procedures that also have the support of the industry. However, it should be remember that traditional techniques including abdominal retropubic urethropexia (Burch colposuspension), among others, in good hands are associated with an effectiveness quite close to that of suburethral slings but without the risk of complications or rejection of the prosthetic material. Further advantages inherent to the vaginal approach are obtained when these procedures are performed transvaginally, such as theour technique of transvaginal colpo-urhetropexy using autologous vaginal flaps [7-9].
Brief Anatomical and physiopathological review of sui anatomy
Every surgeon must have a thorough knowledge of the anatomical details of the surgical region in which the operation is going to be performed and, although this is not the objective of the study, a brief review of some structures that are actively involved in the control and maintenance of statics of the pelvic organs and urinary continence in women seems adequate [10]. The urogenital diaphragm and the pelvic diaphragm are two essential structures of the female pelvis.
Urogenital diaphragm: The deep transverse perineal muscle is the main pillar. It is composed by striated muscle and fibro connective tissue, lying in a horizontal plane with lateral ischiopubic insertions and a medial insertion in the perineal body, which is a rigid structure that separates the vulvar vestibule from the rectum [11]. The urogenital diaphragm also includes the superficial part of the anal sphincter and the vulvar constrictor muscle, as well as an aponeurotic sheet in which the roots of the clitoris covered by the bulbocavernous and ischiocavernous muscles converge, forming a firm tissue inserted in the outer surface of the diaphragm. The dorsal limit is constituted by a reinforcement of the entire tissue, known as superficial transverse perineal muscle, which delimits the entrance of the ischiorectal fossa.
Pelvic diaphragm: It is less complex than the urogenital diaphragm but more resistant. The pelvic diaphragm is composed of the two levatorani muscles and their superior and inferior fascial covering. The levatorani is inserted into the ventral and lateral surfaces of the pelvic walls. The most external part is separated from the pelvic wall by the ischiorectal fossa. An important insertion is found in the back of the pubis, which constitutes the basic point of support for the colpo-urhetropexy technique. The muscular fibers run through part of the vagina to attach to the lateral coccygeal walls. The pubococcygeus and puborectalis muscles are components of the levatorani muscle. Ventrally the muscular sheet of these two muscles leaves a midline gap for the urethra and vagina (urogenital hiatus) and the anal canal (anal hiatus). The relative fascial attachment weakness between the vagina with the retropubis allows surgicalmaneuvers such as colpo-urhetropexy (Figure 1).
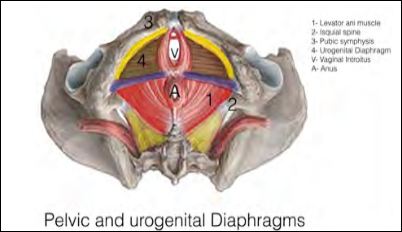
Figure 1: Pelvic diaphragm and urogenital diaphragm.
Physiopathology of SUI: The two more common causes of SUI are urethral hypermobility and intrinsic urethral sphincteric deficiency [3]. Urethral hypermobility results from weakening of the endopelvic fascia and levatorani muscles. The urethra tries to stop to flow of urine but contracture is insufficient to avoid involuntary leaking of urine. Intrinsic urethral sphincteric deficiency is the consequence of progressive hypotonicity of striated musculature around the bladder neck and the external sphincter is not able to fully close [4]. From a strict anatomical point of view, urethral hypermobility and urethral sphincter deficiency are the basis of SUI, but a series of predisposing or aggravating factors should be considered. From the adverse effect of different psychoactive drugs, the atrophy or hypotrophy of bladder and urethral mucosa associated with menopause, the gynaecologist should have a complete history of the patient before taking any decision based only on specific diagnostic studies of SUI.
Patients and Methods
This is a retrospective study based on a cohort of 34 female patients aged between 39 to 78 years old. All of them with clinical diagnosis (by means of objective clinical tests, such as the pad test, coughing test, Valsalva’s maneuver and anamnesis during the medical visit) of stress urinary incontinence due to a urethro-vesical junction (bladder neck) mobility with at least 12 month since the diagnosis was made.
All of the patients also have no other urinary tract symptoms, such as overactive bladder or cystitis, the urine culture was normal and they did not have any pelvic surgery background. Patients with a postvoid residual urine volume of >100 mL, a bladder capacity of <300 mL, impaired compliance or neurological lesions were excluded.
Some of the patients (12) have an anterior and/or posterior pelvic organ prolapse Stage II or less (Baden &Walker and POP -Q), correct- ed with a simple vaginoplasty in the same surgical procedure, just be- fore the colpo-urethropexy was done. The patients signed an informed consent for the procedure.
The primary endpoint was the absence of urine leakage at 3, 6 and 12 months after surgery, as well as in routine annual controls thereaf- ter by means of the same objective clinical tests, such as the pad test, coughing test, Valsalva’s maneuver and anamnesis during the medical visit.
Colpo-urhetropexy with bilateral vaginal autologous flaps
Colposuspensions include different surgical techniques the goal of which is to suspend and stabilize the urethra. The Burch retropubic urethropexy and placing instruments that allow increasing tension of suspension based on the original Vecchietti technique have been common procedures some years ago. These techniques, however, have become obsolete with the development of sling procedures based on the introduction of synthetic material (mesh) to create a sling that supports the urethra. Sling procedures have significantly and favour- ably impacted the field of surgical treatment of SUI. In these mini- mally invasive procedures, the surgeon places a thin piece of flexible, permanent surgical mesh under the urethra, like a sling, to prevent involuntary urine leakage using the retropubic approach (TVT) and the transobturator approach with the out-in (TOT) or in-out TOT-O) techniques. The sling is made of monofilament polypropylene mesh.
Sling procedures have represented an important step in the treat- ment of SUI but it is difficult to determine reliable data on the success and rejection rates of these operations. Our technique using the pa- tient’s own vaginal tissue was designed precisely to avoid any possibil- ity of rejection associated with the use of synthetic materials. Histori- cally, we have a precedent in the Bologna and Shlomo Raz procedures, in which two pedicles of vaginal flaps posterior to the urethral meatus are created and passed through the retropubic space to the suprapubic pelvic fascia to support the bladder neck, but the complications be- cause of this abdominal step are more frequent (Figure 2).
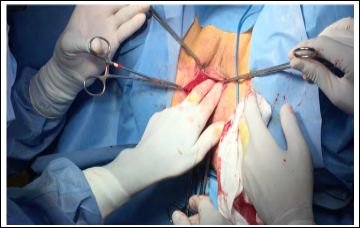
Figure 2: Colpo-Urhetropexy with Bilateral Vaginal Autologous Flaps.
Description of our procedure: It is based on the placement of an au- tologous tissue and, therefore, without possibility of rejection, which like a bridge should be inserted under the urethra near to the exit from the bladder and fixed to the retropubic periosteum and to the musculotendinous sheet in the basis of the implantation of the pelvic diaphragm. The vaginal flap is made by releasing a surplus vaginal mucosa, in some cases obtained after reduction of the cystocele. A vaginal flap, 5 mm width is deserted and with a sufficient length to maintain tension once fixed to the contralateral retropubis. The same maneuver is made with the other vaginal aspect opened prior to re- duction of the cystocele.
Both pedicles flaps are cross over one another forming and X-shape to support the urethra (Figure 3).
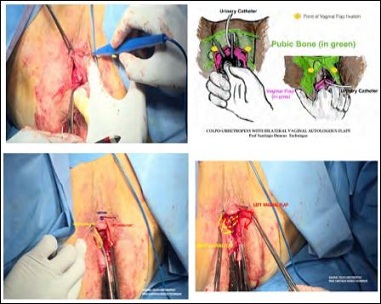
Figure 3: Colpo-Urhetropexy with Bilateral Vaginal Autologous Flaps Prof. Santiago Dexus Technique.
Result
The present series is limited to 34 patients, and although this number is insufficient to draw definite conclusions regarding effectiveness of the procedure, we have performed this technique in at least 100 patients. Unfortunately, the medical records of these patients could not be retrieved because we moved to another medical center and most patients continued to be followed at the hospital at which surgery was initially performed. However, despite the reduced number of cases, the present data based on the ages of the patients and the years with full continence in the majority of cases illustrate the excellent results obtained with this procedure.
Physiotherapy treatment before surgery was carried out in 6 patients. Urodynamic studies before surgery were also performed in 6 patients. At present, urodynamic studies are systematically performed preoperatively, and patients with morbid obesity or body mass index … are excluded from surgical repair.
In 19 patients, SUI was associated to different pathologies of the pelvic floor, such as uterine prolapse, cystocele, rectocele or the sum several alterations of pelvic statics, the surgical repair of which was carried out at the time of the trans-vaginal colpo-urhetropexy procedure. In this group of patients, 8 developed a new mild cystocele or rectocele, in one patient grade 2 cystocele appeared and in another patient, grade 3 rectal prolapse in the Douglas pouch occurred. None of these patients with posterior pelvic floor pathology has recurrent urinary incontinence after colpo-urhetropexy.
A total of two failures were observed: one case in a patient with morbid obesity who continued with SUI after operation (the obesity of this patient should have been previously treated) and another case in a patient with intermitted urinary incontinence, which was present only at some stressful circumstances. The rate of failure was 5.9% (2 out of 34 patients) using a very strict criteria for the inclusion of one case.
In our opinion, the age of the patients and the years being continent are interesting findings of the study. The youngest patient was treated at the age of 39 and is currently continent 20 years later. Three patients aged 83 years are also continent after 18, 10 y 5 years of surgery. Finally, the series include a patient who was operated on at 83 years of age, who remains continent at the last follow-up at the age of 91 years.
Conclusion
Bilateral colpo-urhetropexy is an easily performed surgical procedure that can be carried out together with repair of other pelvic floor disorders: vaginal hysterectomy, colpoperineoplasty surgery, anal sphincter reconstruction. The short- and long-term results have been satisfactory with no morbidity in our series. Insertion of synthetic mesh that increases the cost of the procedure and can be rejected is not necessary, so that colpo-urhetropexy with autologous vaginal flaps may be considered a valid, effective and safe option among the set of surgical procedures for the treatment of SUI.
References
- Bologna U (1978) A new surgical procedure for the correction of minary stress incontinence in the female. Urol Int 33: 150-158.
- Raz S (1981) Modified bladder neck suspension for female stress Urology 18: 82-84.
- Ulmsten U, Henriksson L, Johnson P, Varhos G (1996) An ambu- latory surgical procedures under local anesthesia for treatment of female urinary Int Urogynecol J Pelvic Floor Dysfunct 7: 81–85.
- Delorme E (2001) Transobturator urethral suspension: Miniinvasive procedure in the treatment of stress incontinence in women. Prog Urol 11: 1306-1313.
- Latthe PM, Singh P, Foon R, Toozs-Hobson P (2010) Two routes of transobturator tape procedures in stress urinary incontinence: a meta-analysis with direct and indirect comparison of randomized BJU Int 106: 68-76.
- Latthe PM, Foon R, Toozs-Hobson P (2007) Transobturator and ret- ropubic tape procedures in stress urinary incontinence: a system- atic review and meta-analysis of effectiveness and complications. BJOG 114: 522-531.
- Novara G, Galfano A, Boscolo-Berto R, Secco S, Cavalleri S, et (2008) Complication rates of tension-free midurethral slings in the treatment of female stress urinary incontinence: A systematic review and meta-analysis of randomized controlled trials comparing tension-free midurethral tapes to other surgical procedures and dif- ferent devices. Eur Urol 53: 288-308.
- Jiménez Calvo J, Hualde Alfaro A, Raigoso Ortega O, CebriánLos- tal JL, Alvarez Bandres S, et al. (2008) Our experience with mini tapes (TVT Secur and Miniarc) in the surgery for stress urinary in- ActasUrol Esp 32: 1013-1018.
- Navazo R, Moreno J, Hidalgo C, Herraiz MA, Vidart JA, et (2009) Contasure needleless: A single incision tot for the surgical treatment of stress urinary incontinence. Arch Esp Urol 62: 719-723.
- Baden WF, Walker TA (1992) Fundamentals, symptoms, and clas- sification: In surgical Repair of Vaginal Lippincott; Philadel- phia: 1992. pp. 1-23.
- Navalón V, Navalón P, Pallás Y, Ordoño F, Monllor E (2014) Outpa- tient surgical treatment of female stress urinary incontinence under local anesthesia-sedation with Contrasure Needleless Ac- tas Urol Esp 38: 49-54.
- Hom D, Desautel MG, Lumerman JH, Feraren RE, Badlani GH (1998) Pubovaginal sling using polypropylene mesh and Vesica bone anchors. Urology 51: 708-713.
Citation:Salcedo FL, Dexus S, Dexus D (2019) Colpo-Urhetropexy: Results of a Technique with Autologous Vaginal Flaps for Treating Stress Urinary Incontinence. J Perina Ped 3: 007.
Copyright: © 2019 Salcedo FL, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.