*Corresponding Author:
Xuexun Li,
Department of Cardiology, Beijing Chaoyang Hospital, Capital Medical University and The Affiliated Hospital of Medical College, Qingdao University, Beijing, China
Tel: +86 13910835371
E-mail: shflahopw@sina.com
Abstract
Left Ventricular Summit (LVS) is the most common region of origins of idiopathic epicardial Ventricular Arrhythmias (VAs). VAs originating from this region can be eliminated by catheter ablation applied by using approaches like pericardiocentesis, the coronary venous system, adjacent structures. However, VAs from LVS remain challenging for the risk of coronary artery injury. Many tools like Computed Tomographic Angiography (CTA), Cardiac Magnetic Resonance (CMR) or Intracardiac Echocardiography (ICE) may be helpful, but all these methods have some limitations. A more efficient and safer strategy of VAs originating from LVS guided by CARTOUNIVUTM module has been reported. This novel approach could integrate coronary artery angiogram with 3D map on the CARTO3 system with CARTOUNIVUTM module. It could accurately reveal the distance between the site of ablation catheter and the coronary arteries in the real time to decrease the risk of coronary artery injury.
Keywords
Ablation; CARTOUNIVUTM; Left ventricular summit; Ven- tricular arrhythmias
The Left Ventricular Summit (LVS) most superior to the Left Ventricular (LV) outflow tract is a triangular area bounded by the bifurcation of the left anterior descending artery and the left circumflex artery and the first septal perforating branch. The LVS is the most common Site of Origins (SOO) of idiopathic epicardial Ventricular Arrhythmias (VAs) [1]. Although the understanding of the electrocardiographic and electrophysiological characteristics of VAs originating from the LVS has improved, ablation of this VAs is still challenging due to the proximity to the coronary arteries.
When VAs are located in the LVS site, catheter ablation can be more complicated and is associated with higher rates of recurrence, and potential risk of coronary artery injury.
The common approach used in the LVS ablation is that after the targeted ablation site had been located by the activation mapping and pacing mapping, coronary angiography would be performed to identify the distance between the ablation catheter and the closest coronary artery in order to prevent accidental coronary artery lesions. Ablation application would be avoided if two perpendicular projections showed that the ablation catheter was <5 mm away from the coronary artery. When the targeted ablation site is close to the coronary artery with the distance <5mm, adjacent structures ablation appear to be a safe alternative. Contrast-enhanced CT Angiography (CTA) or Cardiac Magnetic Resonance (CMR) performed prior the procedure is also used by some physicians to the location of the ablation catheter relative to the coronary arteries in some center [2].
Recently, enriquez et al. found Intracardiac Echocardiography (ICE) displayed with the CartoSoundTM module (Biosense Webster, Diamond Bar, CA, USA) had the advantage over CT or MRI [3]. ICE could be performed online during the procedure, and images could be integrated into the mapping system immediately. Besides, the ostium and course of the coronary artery could be located with Doppler flow and reconstructed on the map. However, it should be noticed that all these methods above have different deficiencies, such as complicated procedures, integration resolution errors, insufficient locating accuracy, etc.
We developed a novel ablation strategy of premature ventricular contractions originating from LVS guided by CARTOUNIVUTM module, which is more efficient and safer [4]. In the study, we reported our experience of VAs originating from LVS region catheter ablation in combination with the CARTOUNIVU™ module in order to integrate the coronary artery angiogram. CARTOUNIVUTM module initially developed by Biosense Webster to reduce X ray exposure could integrate the fluoroscopic images into 3d Electroanatomical Mapping Systems (EAMS) [5].
First the registration process of CARTOUNIVUTM module must be finished. A fluoroscopic image should be captured with the fluoroscopy arm placed over the registration plate in the anterior posterior orientarion. Then the captured image would be delivered to CARTO system, and the table is repositioned to finish the registration process. If VAs originating from the LVS was doubted from the 12-lead Electrocardiogram (ECG) analyzation, Coronary artery angiography from multiangular projections would be performed immediately after the registration process.
Immediately, fluoroscopy images captured in different projections would be sent to the CARTO 3 system before they were integrated into the EAMS.
Then the ablation catheter could create an exquisite electroanatomical map with the context of captured images. Anatomical shells of Great Cardiac Vein (GCV), aortic root, and LV would be created accurately and displayed on the map viewer with the fluoroscopy image. After that a detailed activation mapping of all LV summit and adjacent structures was performed to locate the SOO of VAs. If the activation mapping is not satisfactory, a pace mapping could be applied on the precise anatomical shell.
A detailed anatomical relationship between the SOO and adjacent structures could be revealed. Distance of the SOO to the closest cor- onary artery could be revealed precisely and measured accurately in real time. It is more accurate than CTA or CMR image. Though ICE could clearly show anatomical LV structures, it could not precisely represent coronary artery due to the obscure echo image like this ap- proach, and not be convenient like this method either.
To our knowledge, this is the first study demonstrating the ablation of VAs originating from LV summit with CARTOUNIVUTM to accurately identify the distance between the targeted ablation area and coronary artery. During the ablation, the distance between the ablation catheter and coronary artery can be observed in real time, which effectively ensures the safety of the operation and avoids the risk of coronary artery injury. The flow of the procedure is represented in the schematic diagram (Figure 1). Coronary artery angiography was immediately performed after the registration process. Then a 3D electroanatomical mapping would be finished. Finally, fluoroscopy images captured in different projections would be integrated with 3D mapping shell before the ablation procedure.
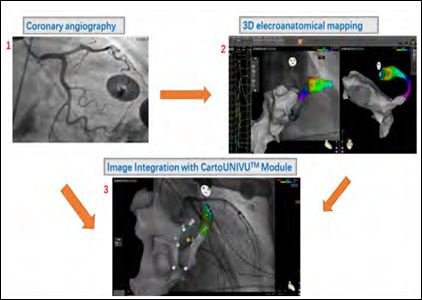
Figure 1: Schematic diagram of the work flow.
Note:
Step1. Coronary artery angiography was performe.
Step2. 3D electroanatomical mapping was finished.
Step3. Fluoroscopy images were integrated with 3D mapping shell.
CARTOUNIVUTM module has been widely used in the ablation of all kinds of cardiac arrhythmias mainly to reduce radiation exposure [6]. Our study confirmed that it could reduce more procedural and fluoroscopic time than traditional approach. Shirai Y et al. reported the procedural time and fluoroscopic time were 342 ± 98 minutes and 45.0 ± 21.5 minutes in the ablation of VAs linked to the coronary venous system with traditional approach [7]. The procedural and fluoroscopic time reported in our study was as low as 78.6 ± 22.7 minutes and 12.5 ± 3.1 minutes respectively.
We believe this approach could also be applied in other kinds of VAs ablation to avoid coronary artery lesions. A similar approach was applied by Alazard et al. in the ablation of posteroseptal accessory pathway specially in children worked well too [8]. Apparently, it could also be used in epicardial ablation of VTs with percutaneous epicardial approach by overlaying the map with an angiogram of the coronary arteries to avoid epicardial vessel lesions.
Our experience suggests that a standard coronary angiogram with two perpendicular projections is not sufficient to accurately show the distance between the coronary artery and ablation catheter. Coronary angiogram integrated to the CARTOUNIVUTM module system should be a better approach since it allows a more precise and constant assessment of the security margin in a 3D map. Though this approach is more convenient and safer, a coronary angiography is still necessary after the ablation procedure.
References
- Yamada T, McElderry HT, Doppalapudi H, Okada T, Murakami Y, et al. (2010) Idiopathic ventricular arrhythmias originating from the left ventricular summit: Anatomic concepts relevant to Circ Arrhythm Electrophysiol 3: 616-623.
- Carrigan TP, Patel S, Yokokawa M, Schmidlin E, Swanson S, et al. (2014) Anatomic relationships between the coronary venous system, surrounding structures, and the site of origin of epicardial ventricular J Cardiovasc Electrophysiol 25: 1336-1342.
- Enriquez A, Malavassi F, Saenz LC, Supple G, Santangeli P, et al. (2017) How to map and ablate left ventricular summit arrhythmias. Heart Rhythm 14: 141-148.
- Li X, Li J, Chu H, Liu X (2020) A novel ablation strategy of premature ventricular contractions originating from summit guided by CartoUNIVU Clin Cardiol.
- Cano O, Alonso P, Osca J, AndrésA, Sancho-Tello MJ, et al. (2015) Initial experience with a new image integration module designed for reducing radiation exposure during electrophysiological ablation J Cardiovasc Electrophysiol 26: 662-670.
- Christoph M, Wunderlich C, Moebius S, Forkmann M, Sitzy J, et (2015) Fluoroscopy integrated 3D mapping significantly reduces radiation exposure during ablation for a wide spectrum of cardiac arrhythmias. Europace 17: 928-937.
- Shirai Y, Santangeli P, Liang JJ, Garcia FC, Supple GE, et (2019) Anatomical proximity dictates successful ablation from adjacent sites for outflow tract ventricular arrhythmias linked to the coronary venous system. Europace 21: 484-491.
- Alazard M, Lacotte J, Horvilleur J, Ait-Said M, Salerno F, et (2018) Preventing the risk of coronary injury in posteroseptal accessory pathway ablation in children: Different strategies and advantages of fluoroscopy integrated 3D-mapping system (CARTO-UNIVU). J Interv Card Electrophysiol 52: 127-135.
Citation: Li X, Liu X (2020) Ablation of Idiopathic Ventricular Arrhythmias Origi- nating from the Left Ventricular Summit with CARTOUNIVUTM Module. J Cardio Cardiovasu Med 4: 016.
Copyright: © 2020 Li X, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.


